Cognitive Decline And Dementia
Cognitive decline refers to a decrease in thinking abilities including attention, visuo-spatial skills, memory, planning, judgement, and language. Dementia is defined as cognitive decline that affects a persons ability to carry out their daily activities. Read an excellent overview of cognitive decline in Parkinsons.
Cognitive profile
Whereas Alzheimers disease is characterized by memory loss, with other cognitive domains or areas affected at later stages, PD dementia typically has a different profile. Executive dysfunction or the ability to plan and organize activities in order to solve problems and complete tasks with multiple steps, is often one of the first difficulties to be noticed. Visuo-spatial dysfunction in which a person has trouble navigating the world around him/her is often seen as well. Other cognitive domains can be affected as the dementia progresses.
On the flipside, apathy, or an actual lack of interest or motivation in activities, is common in advanced PD which causes people with advanced PD to disengage from social interactions. Regardless of the attempts of others to connect with the person with advanced PD, motor difficulties, speech difficulties and cognitive difficulties all conspire to make the person with PD retreat from these interactions.
Is it Parkinsons disease dementia or Dementia with Lewy bodies?
Non-drug approaches
Medication approaches
How Do I Cope With Depression Related To Parkinsons Disease
Besides treatments, other strategies can boost your mood and increase your self-worth:
- Ask for help. Remember, depression isnt a sign of weakness. Its caused by chemical changes in your brain.
- Connect with Parkinsons disease support groups in person or online.
- Exercise several times a week.
- Maintain your hobbies and activities.
- Schedule fun activities in advance so you have things to look forward to.
- Identify small tasks you can accomplish each day, such as completing a chore, exercising or calling a friend.
- Take part in social activities so you dont feel isolated.
- Try complementary therapies, such as music therapy, relaxation techniques, massage, acupuncture and meditation.
Evaluation Of Depression In Parkinsons Disease
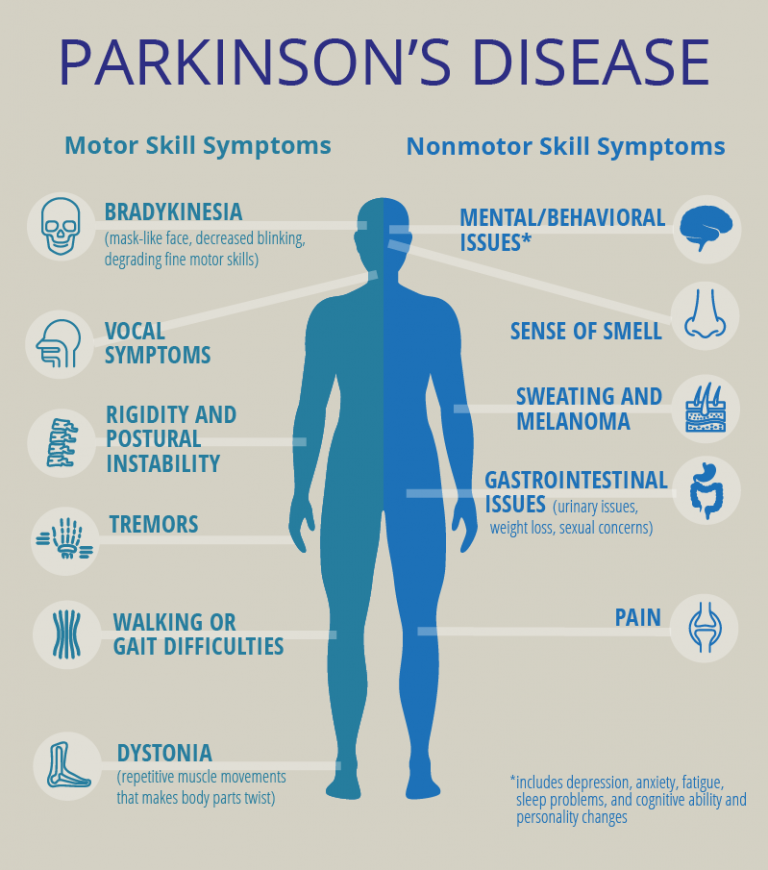
Recognizing depressive symptoms in Parkinsons disease can be challenging because the psychomotor slowing and blunted affect commonly seen in depression can resemble the bradykinesia and masked facial expression of Parkinsons disease. Additionally, somatic features of depression such as decreased appetite, low energy, and sleep disturbances are commonly seen in patients with Parkinsons disease who do not have depression. Furthermore, depression must be differentiated from apathy, which commonly occurs in Parkinsons disease, is characterized by diminished motivation, and has significant overlap with depressive symptoms. A potentially useful discriminating feature is mood, which is negative in depression and neutral in apathy . It is important to remember that the differential diagnosis for depression is broad and includes other psychiatric disorders such as bipolar disorder, cognitive disorders, neoplastic processes affecting the central nervous system, metabolic and endocrine abnormalities, infections, hypoxemia, sleep disorders, medication side effects, and substance use, as well as hypoactive delirium caused by a variety of underlying illnesses.
TABLE 1. Management of Depression in Parkinsons Disease
| Evaluation |
You May Like: Parkinson’s Donations In Memory Of
Depression And Anxiety In Parkinson Disease
volume 6, pages 243245
Evidence suggests that both anxiety and depression might have pathophysiological links with Parkinson disease , as these mood disorders are more prevalent in individuals with PD than in patients with other chronic conditions. A new study reports that depression and anxiety are associated with different patterns of PD-related factors, suggesting divergence between the underlying mechanisms.
Anxiety and depression frequently occur and often coexist in patients with Parkinson disease . In such individuals, the lifetime risk of developing depression or anxiety is 60%, with the cross-sectional prevalence for each disorder being 3040%., By contrast, the average prevalence of clinically relevant depression syndromes in the general population has been reported to be 13.5%, while the prevalence of anxiety disorders in adults aged > 60 years has been found to lie somewhere between 1.2% and 14%. As these affective disorders have a strong effect on quality of life and also increase patient disability, additional knowledge of the prevalence, characteristics, pathophysiology and management of anxiety and depression in PD is urgently needed. A cross-sectional epidemiological study by Nègre-Pagès et al. aimed to further our understanding of such disorders in this setting.
This is a preview of subscription content, access via your institution
Living With A Dog With Parkinsons Disease
Living with a dog with any kind of degenerative disease can be challenging. Your dog is likely very confused about what is going on with their body. A dog with Parkinsons disease will feel out of control and betrayed by their body almost.
Its important to be gentle with your dog during this time.
Though Parkinsons disease is incurable and progressive, there are some things your vet may recommend that will help with your dogs quality of life for as long as possible.
Also Check: Foods Not To Eat With Parkinson’s Disease
How Can Parkinsons Disease Cause Depression
For many people, the challenges of Parkinsons disease are enough to cause depression.
But scientists believe that depression in Parkinsons might also come from changes to certain chemicals in the brain:
- Losing interest in activities you once enjoyed.
- Losing interest in eating or taking care of yourself.
- Moving or talking too slow.
- Thinking a lot about dying or wishing to die.
Neuroimaging Of Apathy In Pd
There were 14 neuroimaging studies of apathy in PD . Similar to the studies of depression and anxiety in PD, most imaging studies of apathy in PD utilized either PET or SPECT techniques 14, 17, 55, 56, 57, 58, 59, 60, 61 and focused on measuring cerebral glucose metabolism with the exception of two PET studies 17, 60 and one SPECT study 61 examining dopaminergic changes associated with apathy. Of the 14 studies, five involved T1weighted imaging 14, 62, 63, 64, 65, two used RSFMRI 40, 64 and one study performed DTI in addition to T1weighted imaging 65. Approximately half of the studies used ROI methods with caudate, putamen and limbic regions being the most common ROIs. All 14 studies excluded patients with cognitive symptoms and seven of them included patients who remained on antiparkinsonian medication during MRI scanning. Additionally, three of the 14 studies recruited patients who were on mood stabilizers. Amongst the 14 studies, five studies clearly excluded patients with depression 55, 57, 58, 59, 61, whilst seven studies did not 14, 17, 60, 62, 63, 64, 65 and two did not indicate whether patients with depression were excluded from the studies 40, 56.
You May Like: Parkinson’s Disease And Brain Function
Treatment For Anxiety And Depression
Your doctor might suggest medication, talk therapy, and lifestyle changes like exercise and social activities. Many doctors find that a combination of treatments works best.
Everyoneâs different, so the doctor will base your treatment on your needs. Be patient. It may take time to figure out what works best for you.
Your doctor can prescribe antidepressants like SSRIs, SNRIs, or benzodiazepines, which are anti-anxiety medications. They might adjust the levels of your Parkinsonâs medications to see how it impacts your mood.
Talk therapy, which is also called psychotherapy, can help you understand your anxiety and depression and give you tools to manage your symptoms.
Your therapist may try cognitive behavioral therapy, or CBT, to help you change negative thought patterns and learn how to react to situations in a better way.
You can also get help through group therapy or support groups. Theyâre good for connecting with other people who relate to what youâre going through, sharing your thoughts, and learning from other peopleâs experiences.
Prefrontal Physiomarkers Of Anxiety And Depression In Parkinsons Disease
- 1Department of Neurological Surgery, University of California, San Francisco, San Francisco, CA, United States
- 2Department of Psychiatry, University of California, San Francisco, San Francisco, CA, United States
- 3Department of Neurology, University of California, San Francisco, San Francisco, CA, United States
Objective: Anxiety and depression are prominent non-motor symptoms of Parkinsons disease , but their pathophysiology remains unclear. We sought to understand their neurophysiological correlates from chronic invasive recordings of the prefrontal cortex .
Methods: We studied four patients undergoing deep brain stimulation for their motor signs, who had comorbid mild to moderate anxiety and/or depressive symptoms. In addition to their basal ganglia leads, we placed a permanent prefrontal subdural 4-contact lead. These electrodes were attached to an investigational pulse generator with the capability to sense and store field potential signals, as well as deliver therapeutic neurostimulation. At regular intervals over 35 months, participants paired brief invasive neural recordings with self-ratings of symptoms related to depression and anxiety.
Interpretation: These findings suggest a physiological basis for anxiety and depression in PD, which may be useful in the development of neurostimulation paradigms for these non-motor disease features.
Recommended Reading: Parkinson’s And Muscle Cramps
Anxiety And Antiparkinsonian Medications
There is no consensus on whether antiparkinsonian medications are responsible for symptoms of anxiety in Parkinsons disease.
Stein et al found that the levodopa dose was similar in anxious and non-anxious patients. Hendersonet al noted that 44% of patients with Parkinsons disease noticed anxiety symptoms before starting levodopa. Menza et al found that the levodopa dose did not significantly correlate with anxiety levels: they suggested that anxiety in patients with Parkinsons disease is unlikely to be a side effect of levodopa treatment. In contrast, Vasquez et al found that panic attacks were related to levodopa therapy but not to other agonist drugs.
Lang reported anxiety in five of 26 patients when pergolide was added to their treatment regimen. Menza et al found no differences in measures of anxiety in patients receiving or not receiving pergolide. Menzaet al found no differences in measures of anxiety in patients receiving or not receiving selegeline.
The temporal relationship between panic attacks and off periods have led some authors to suggest that panic attacks may be related to falling brain levodopa levels. Anxiety fluctuations may be an important component of levodopa induced fluctuations. In a double blind placebo controlled trial, Maricle et al found that anxiety levels fell and motor performance improved during a levodopa infusion.
Recommended Reading: What Is Parkinsons Disease And How Do You Get It
How Is Depression Treated In People With Parkinsons Disease
Depression must be treated differently in people who have Parkinsons disease. Many people can be treated with a type of antidepressant called serotonin reuptake inhibitors . However, some other Parkinsons symptoms may worsen from SSRI use in a very small number of people.
SSRIs shouldnt be taken if youre currently taking selegiline . This is a commonly prescribed medication to control other symptoms of Parkinsons.
If both are taken at once, it could cause serotonin syndrome. Serotonin syndrome occurs when theres excessive nerve cell activity, and it can be fatal. Symptoms can include:
- confusion, disorientation, or hallucinations
- digestive issues like diarrhea or nausea
- rapid heartbeat, or tachycardia
- overactive reflexes, or hyperreflexia
Some medications used to treat other symptoms of Parkinsons, like dopamine agonists, may have an antidepressant effect. These appear to be particularly helpful in those who experience periods when their medication isnt effective. This is also known as on-off motor fluctuation.
Read Also: Emory Parkinson’s Disease Research
Depression Diagnosis Challenges In Pd
Depression in Parkinson’s can be hard to recognize. Certain depression symptoms overlap with those of PD. For example, sleep problems and feeling slowed down occur in both conditions.
Some experts think that depression in PD often involves frequent, shorter changes in mood versus a constant state of daily sadness. Other things that can complicate a Parkinson’s depression diagnosis include:
- Facial masking, a symptom cause by Parkinson’s effect on face muscles that can make it difficult for a person with Parkinson’s to visibly express emotion.
- People with Parkinsons often do not recognize they have a mood problem or are unable to explain symptoms, so they don’t seek treatment. It’s helpful to ask a care partner or loved one if they have noticed any mood changes.
Do I Need Health Insurance To Receive This Service
The referral service is free of charge. If you have no insurance or are underinsured, we will refer you to your state office, which is responsible for state-funded treatment programs. In addition, we can often refer you to facilities that charge on a sliding fee scale or accept Medicare or Medicaid. If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
Recommended Reading: Parkinson’s Disease Inheritance Pattern
Anxiety And Parkinsons Research
What does this finding mean for the future of diagnosis or treatment of Parkinsons? Ongoing research is compelling, says Pontone. Part of what we are doing is looking at anxiety disorders that occur long before the onset of Parkinsons to see if there are characteristics that may differentiate that anxiety or predict an increased risk of Parkinsons disease.
Meanwhile, because theres an established link between anxiety and Parkinsons disease, patients and their families should be upfront with their doctors about anxiety symptoms. Behavioral therapy and medications for example, anti-anxiety meds or antidepressants can effectively treat anxiety disorders. Theres no need for anyone to suffer in silence.
Also Check: Is Coffee Bad For Parkinsons Disease
How Can I Notice Depression Symptoms Earlier
The earlier you notice and report symptoms of depression, the earlier your healthcare providers can help you. Consider the following:
- Ask a friend or family member to look out for any changes in your mood, since you might not notice.
- Bring a loved one to your appointments. They can contribute to conversations about your mood.
- Ask a healthcare provider to screen you for depression at least once a year. Many questionnaires and tools are able to identify depression.
- Talk with your healthcare providers about your mood at every appointment. Mention if your mood has changed since your last appointment or if you have any symptoms of depression.
Also Check: How Can You Get Parkinson’s
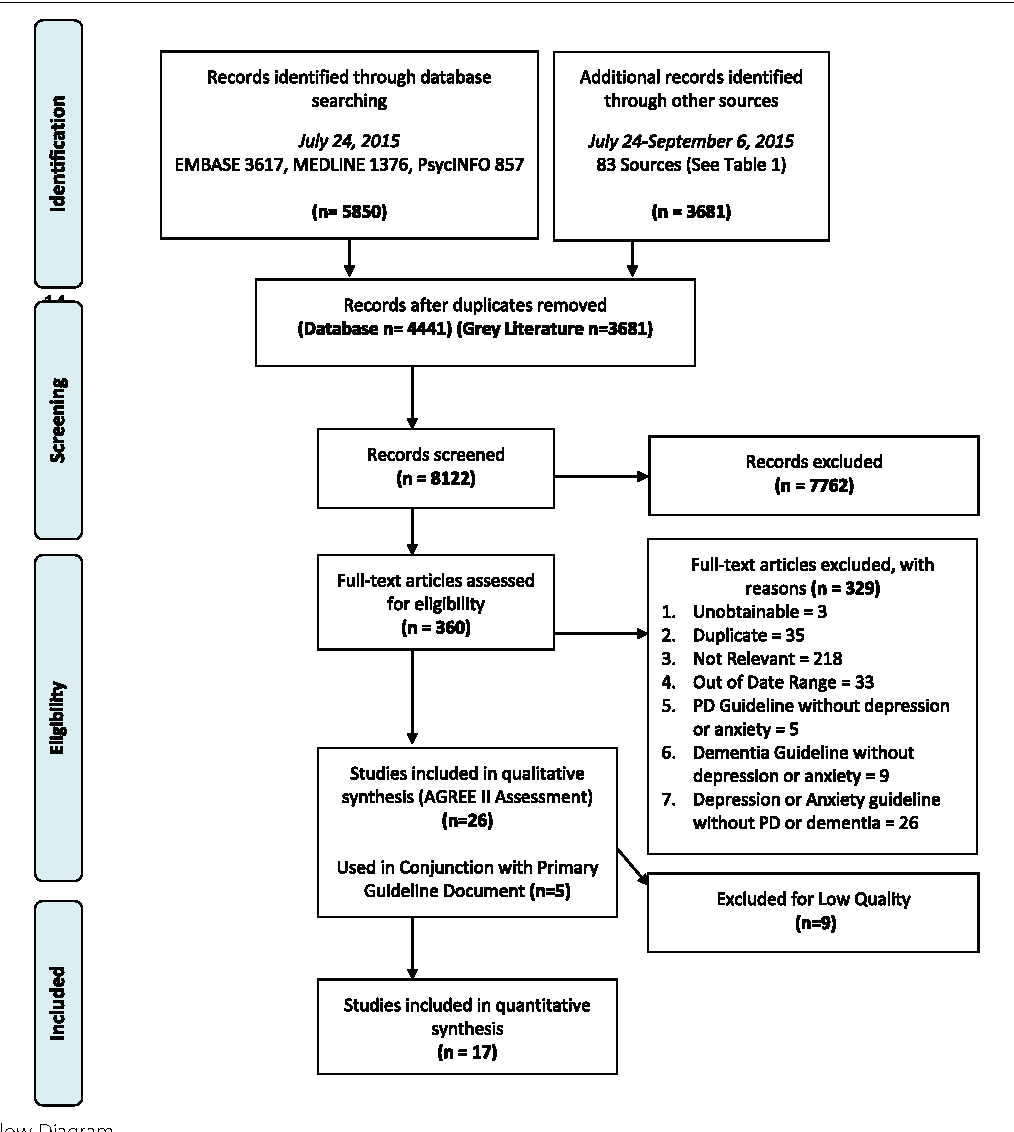
Management Of Depression In Parkinsons Disease
Although traditionally considered a purely motor disorder, Parkinsons disease is increasingly recognized as a complex disease process with diverse neuropsychiatric complications in addition to its motor symptomatology. The range of neuropsychiatric complications associated with Parkinsons disease is broad and includes depression, anxiety, apathy, psychosis, cognitive impairment, impulse control disorders, and sleep disturbances. These neuropsychiatric complications become increasingly prevalent over the course of the disease and are often associated with poorer quality of life, increased disability, worse outcomes, and greater caregiver burden . As mental health providers commonly encounter depression in the Parkinsons disease population, it is important to be familiar with available, validated treatment options for this illness.
What Is The Outlook For Depression With Parkinsons Disease
Many people with Parkinsons disease have depression but dont get help for it. They may not notice their symptoms, or may think the symptoms are unavoidable with Parkinsons.
What they may not realize is that medications, therapy and lifestyle changes can help. Many people find some relief from depression. And that helps reduce their symptoms of Parkinsons disease.
Don’t Miss: Orthopedic Surgery And Parkinson’s Disease
Cognitive Behavioral Therapy Can Help Alleviate Depression And Improve Quality Of Life Rutgers Study Finds
People with Parkinsons disease who engage in cognitive behavioral therapy a form of psychotherapy that increases awareness of negative thinking and teaches coping skills are more likely to overcome depression and anxiety, according to a Rutgers study.
The study was published in the journal Neurology.
About 50 percent of people diagnosed with Parkinsons disease will experience depression, and up to 40 percent have an anxiety disorder.
The psychological complications of Parkinsons disease have a greater impact on the quality of life and overall functioning than the motor symptoms of the disease, said lead author Roseanne Dobkin, a professor of psychiatry at Rutgers Robert Wood Johnson Medical School. Untreated, depression can accelerate physical and cognitive decline, compromise independence and make it more difficult for individuals to proactively manage their health, like taking medication, exercising and visiting the physical therapist.
Depression in Parkinsons patients is underrecognized and often goes untreated. Among those who receive treatment, antidepressant medication is the most common approach, though many patients continue to struggle with depressive symptoms. The researchers investigated how adding cognitive behavioral therapy to the care individuals were already receiving would affect their depression.
Alternative Treatments And Lifestyle Changes
Your doctor could also recommend alternative therapies like:
- Relaxation techniques
Lifestyle changes can also help manage your symptoms. Regular exercise boosts your mood, helps you sleep better, and could ease symptoms. Eating healthy food, getting enough sleep, and making time to relax might help too. Having social support can make a big difference.
If medication, therapy, and alternative treatments donât work, your doctor may consider things like vagal nerve stimulation, electroconvulsive therapy, or other therapies.
Also Check: What Are Signs And Symptoms Of Parkinson’s
Getting Help For Mood Changes
When a person with PD experiences mood changes, they may withdraw from seeking help. However, talking about symptoms with a healthcare professional helps create more of a sense of control and enables the doctor to better understand how PD is affecting the patient. Many treatment options are available to relieve mood disorders like depression and anxiety.1
Electrode Locations And Tractography
To localize ECoG electrodes in individual patients, the preoperative T1 MRI was used to reconstruct cortical surface models in FreeSurfer . A CT scan taken 23 months after surgery was used to determine the location of each cortical electrode. We projected ECoG contacts onto the cortical surface mesh with the imgpipe toolbox using a surface vector projection method . Once we identified cortical locations for each ECoG electrode on individualized cortical reconstructions, we projected all patients recording electrodes onto the Desikan-Killiany atlas brain .
For tractography, we obtained High Angular Resolution Diffusion Imaging on a 3 Tesla MR scanner , using a spin-echo echo-planar imaging pulse sequence , FOV 28 cm × 28 cm, at least 70 axial slices, 2 mm3 isotropic voxels, b-value = 2000 s mm2 in 55 non-collinear gradient directions and a signal to noise ratio > 60. In PD1, b-value was 1,000 s mm2 in 32 non-collinear gradient directions. A single non-diffusion-weighted b0 image was also obtained. The diffusion-weighted tractography was explored using a deterministic tractography software package . Preoperative MRI, postoperative CT and HARDI scans were automatically merged and corrected for distortion. The ECoG contacts used for recordings were manually segmented on the CT scan. The regions of interest were then created by adding 2 mm to each contact and using these as seed regions for fiber tracking analyses, using an FA threshold of 0.17 and a minimum length of 8 cm.
Also Check: Falls With Parkinson’s Disease