What Is Parkinsons Disease
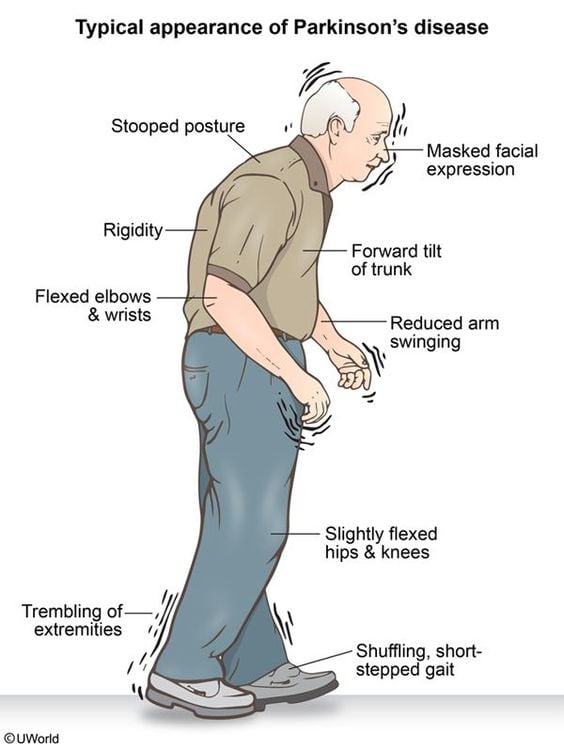
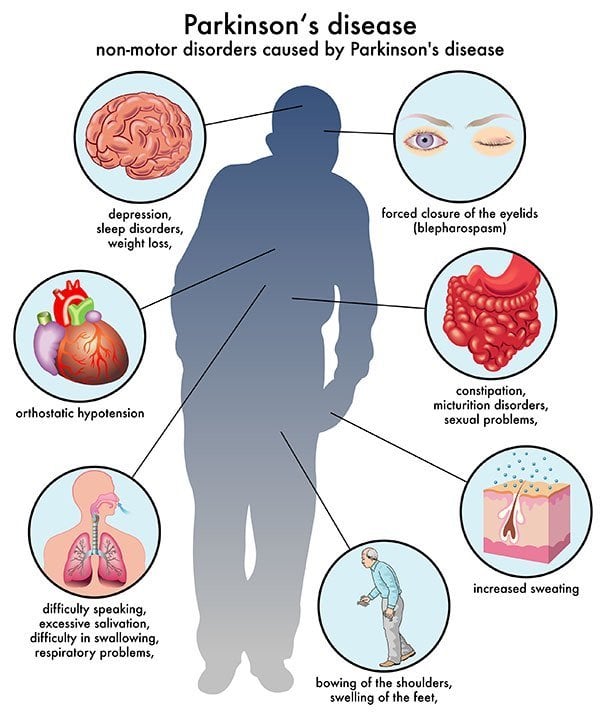
Parkinsons disease is a nervous system disease that affects your ability to control movement. The disease usually starts out slowly and worsens over time. If you have Parkinsons disease, you may shake, have muscle stiffness, and have trouble walking and maintaining your balance and coordination. As the disease worsens, you may have trouble talking, sleeping, have mental and memory problems, experience behavioral changes and have other symptoms.
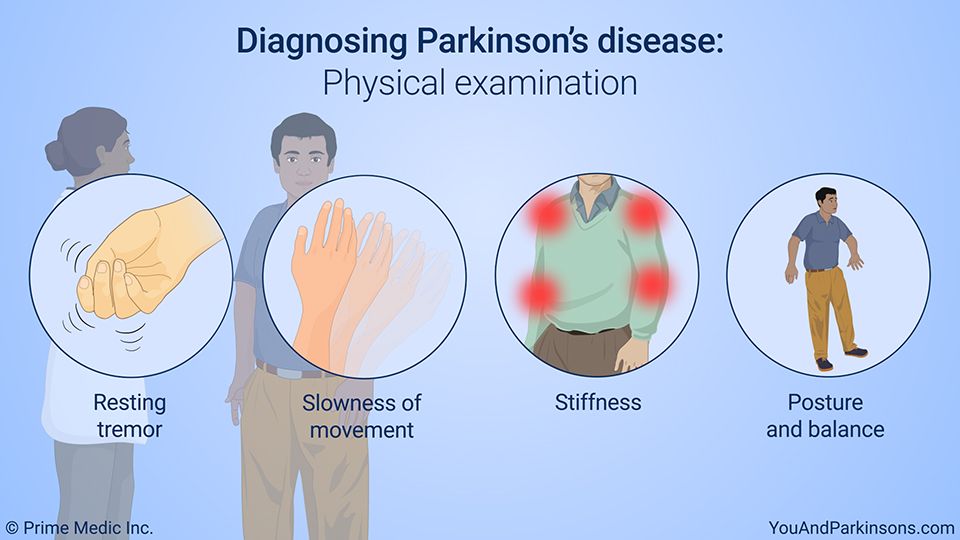
Physical And Neurological Examination
Your doctor will conduct a physical and neurological examination. This can involve observing your behavior, movements, and mental state and conducting tests or asking you to perform certain exercises.
These are some of the symptoms of Parkinsons your doctor can determine visually:
- Fewer spontaneous movements or hand gestures
- Reduced frequency of blinking
- Tremors in your hands while they are at rest, often only in one hand
- Hunched posture or forward lean while walking
- Stiff movements
These are some of the exercises your doctor may ask you to do to evaluate your movements, balance, and coordination:
- Opening and closing your fist
- Tapping your fingers, toes, and heels
- Holding your arms out in front of you
- Moving your finger from one point to another
- Rotating your wrists or ankles
- Standing from a chair
Surgery For People With Parkinsons Disease
Deep brain stimulation surgery is an option to treat Parkinsons disease symptoms, but it is not suitable for everyone. There are strict criteria and guidelines on who can be a candidate for surgery, and this is something that only your doctor and you can decide. Surgery may be considered early or late in the progression of Parkinsons. When performing deep-brain stimulation surgery, the surgeon places an electrode in the part of the brain most effected by Parkinsons disease. Electrical impulses are introduced to the brain, which has the effect of normalising the brains electrical activity reducing the symptoms of Parkinsons disease. The electrical impulse is introduced using a pacemaker-like device called a stimulator. Thalamotomy and pallidotomy are operations where the surgeon makes an incision on part of the brain. These surgeries aim to alleviate some forms of tremor or unusual movement, but they are rarely performed now.
Read Also: Can You Have Parkinson’s Without Shaking
Physical Examination And Tests
A trip to the neurologists office often includes what seems like dozens of questions, along with multiple tests.
There currently are no diagnostic blood tests for Parkinson’s disease, but your doctor may do some routine blood and urine tests to assess your overall health. Your blood pressure will be taken sitting and standing to look for orthostatic hypotension.
A movement disorder specialist will do a variety of physical tests to assess you as well.
Determining Diagnosis Through Response To Parkinsons Medication
If a persons symptoms and neurologic examination are only suggestive of Parkinsons disease or if the diagnosis is otherwise in doubt, the physician may, nevertheless, prescribe a medication intended for Parkinsons disease to provide additional information. In the case of idiopathic Parkinsons, there is typically a positive, predictable response to Parkinsons disease medication in the case of some related Parkinsonian syndromes, the response to medication may not be particularly robust, or it may be absent entirely.
Unfortunately, there are no standard biological tests for the disease, such as a blood test. However, researchers are actively trying to find biomarkers in blood and other bodily fluids that could help confirm the diagnosis.
Also Check: How Can You Test For Parkinson’s Disease
Conditions Misdiagnosed As Parkinson’s Disease
Parkinsons disease, especially in its early stages when symptoms are mild, is not an easy disease to diagnose. The non-specific, and easily overlooked nature of the signs of Parkinsons make it difficult to spot, and unlike many illnesses, there is no one laboratory test or radiological exam that will provide a definitive diagnosis of Parkinsons disease.
Patients exhibiting Parkinsons-like symptoms may undergo blood and urine tests, or CT or MRI scans to exclude other conditions, but none of these will provide a diagnosis of Parkinsons disease. The best way to test for Parkinsons disease is to conduct a systemic neurological examination that includes tests to gauge a patients reflexes, muscle strength, coordination, balance, gait, and overall movement. Even so, according to information presented on The Michael J. Fox Foundation for Parkinsons Research, up to 25 percent of Parkinsons disease diagnoses are incorrect.
So, why is there confusion about diagnosing Parkinsons disease? The simple answer is that symptoms of Parkinsons disease are not clear cut, and therefore, it is easy to mistake them for other conditions, or to classify them as parkinsonian when they are not.
Here is a brief overview of the top ten conditions mistaken for Parkinsons disease:
Beyond those top three, there are other conditions that are often confused with Parkinsons disease, including:
After A Parkinsons Disease Diagnosis: What Comes Next
If you receive a Parkinsons disease diagnosis, your doctor will work with you to find the best treatment plan for your needs. Doctors also have a responsibility to communicate their findings to your caregivers to ensure you receive adequate help and support.
A team of medical professionals will also monitor the stages of Parkinson using the Hoehn and Yahr rating scale. Sometimes it takes years for Parkinsons to progress, but there is no telling how the disorder will affect you on an individual level. Your doctors will work with you to monitor your symptoms and suggest new treatment when appropriate. In the latter stages of Parkinsons, you may need round-the-clock care.
Its important to seek help and support after a Parkinsons disease diagnosis, as the condition can take an emotional toll. It’s also a good idea to get as informed as possible about your health so that you and your family know what to expect. There is currently no cure for Parkinsons disease, but medication and physical therapy can ease symptoms and help you enjoy a better quality of life.
You May Like: How Long Does It Take Parkinson’s To Progress
What Is The Prognosis And Life Expectancy For Parkinson’s Disease
The severity of Parkinson’s disease symptoms and signs vary greatly from person to peson, and it is not possible to predict how quickly the disease will progress. Parkinson’s disease itself is not a fatal disease, and the average life expectancy is similar to that of people without the disease. Secondary complications, such as pneumonia, falling-related injuries, and choking can lead to death. Many treatment options can reduce some of the symptoms and prolong the quality of life.
Will I Get A Parkinsons Disease Diagnosis
Its important to see your doctor if you notice Parkinsons disease symptoms over a period of time, especially if they are interfering with your daily life. You will be given a confirmed diagnosis if you meet Parkinsons disease diagnosis criteria, as long as your symptoms cannot be explained by another condition.
To be diagnosed with Parkinsons, you must show signs of bradykinesia a marked slowing of movement and reduced arm swing when walking as well as one or more of the following symptoms:
- Muscular rigidity
- Postural instability
Recommended Reading: How Can You Get Parkinson’s
How Parkinson’s Disease Is Diagnosed
Claudia Chaves, MD, is board-certified in cerebrovascular disease and neurology with a subspecialty certification in vascular neurology.
There’s no “gold standard” test that will diagnose Parkinson’s disease . Instead, a physician relies on their own clinical observations and judgment, along with a patient’s description of possible signs and symptoms, to make the diagnosis. That, of course, makes a physical examination very important in this process. Much of your doctor’s exam will be aimed at assessing whether you have the so-called cardinal signs of Parkinson’s: resting tremor, rigidity , bradykinesia and postural instability .
Having Parkinsons Is Not A Death Sentence
Parkinsons disease is not fatal, and your life expectancy depends highly on the type of Parkinson’s you have. If the type of disease isn’t causing issues with brain function, you can potentially live as long as people without the disease.
However, if someone has an atypical case of the condition that occurs at the same time as other conditions such as dementia, this can negatively affect their life expectancy.
Also Check: Signs Of Parkinson Disease Early Symptoms
Support For People With Parkinsons Disease
Early access to a multidisciplinary support team is important. These teams may include doctors, physiotherapists, occupational therapists, speech therapists, dietitians, social workers and specialist nurses. Members of the team assess the person with Parkinsons disease and identify potential difficulties and possible solutions.There are a limited number of multidisciplinary teams in Victoria that specialise in Parkinsons disease management. But generalist teams are becoming more aware of how to help people with Parkinsons disease.
How Parkinsons Disease Is Diagnosed
Diagnosing Parkinsons disease can be complicated because there isnt a specific blood test or screening test that can determine whether or not you have it.
Instead, Parkinsons is diagnosed clinically, which means a doctor will examine you, review your symptoms and medical history, and diagnose accordingly.
Parkinsons disease is a neurological condition that can make movement difficult. If your general practitioner thinks you might have Parkinsons, they may refer you to a neurologist who specializes in movement disorders for a diagnosis.
It can be challenging to catch Parkinsons in the early stages because the symptoms may be too mild to notice or meet the diagnostic criteria. Also, early Parkinsons symptoms are often mistaken for typical signs of aging.
The symptoms of Parkinsons disease are also similar to those of other health conditions, which may be misdiagnosed as Parkinsons at first. Your doctor may suggest specific tests and scans to help eliminate other conditions that can mimic the symptoms of Parkinsons disease.
You May Like: Can Medication Cause Parkinson’s
Tom Thought That Because Some Pink Tablets Relieved His Symptoms This Meant He Was Ok He Didn’t
I first suspected there was something wrong when I was travelling and I was writing a postcard to a friend of mine in, in Australia whose name is Anthony Diecopolis. And, and I got to the Anthony Diec and I couldnt finish the opolis. And its very strange my hand had sort of gone into a sort of spasm and it just wouldnt, wouldnt finish writing the, the, the word. And so thats a bit strange.
And so I went when, when I got I, I went to the doctor and said, What on earths going on? And I had since then Id also developed this slight tremor in my right hand. He said, Well its probably, Essential Tremor or trapped nerve or something like that. And anyway, then it got a bit worse and then I was, I was recommended to go to a neurologist. And the neurologist had a look at me and gave me some pills. And he said, Come back and tell me if these work.
This is about, about sort of, nine months after my, my not being able to finish the, the postcard. And, and he said, Take these pills. And the pills worked. Magically the tremors stopped and I thought this is wonderful. And so I went back to the neurologist and I said, Yes everythings fine now. The pills have, the pills have worked. And far from looking happy about this he looked rather, rather grave and he said, I think youd better go to another neurologist.
Questions To Ask Your Doctor
If you receive a Parkinson’s disease diagnosis, you will understandably have questions for your doctor. Here are some questions you might want to ask to help further your understanding of the condition:
- What are the pros and cons of each medication/ treatment?
- What kind of support will I need at home?
- Are there clinical trials I can take part in?
- What lifestyle modifications should I explore to help me feel better?
- How can I manage stress related to Parkinsons disease?
- Are there any foods, supplements or medications I should avoid?
- Can you recommend any Parkinsons support groups?
Read Also: Active Music Therapy And Parkinson’s Disease Methods
Dementia With Lewy Bodies
Related pathologically to PD dementia, DLB is a relatively common cause of dementia. There are diagnostic criteria, but an important feature is development of dementia temporally associated with motor parkinsonism. Patients with PD usually develop dementia only after years with the disease and with severe motor symptoms. In patients with DLB, parkinsonism is usually relatively mild, and tremor is a less common finding than in PD. Treatment of psychiatric symptoms with cholinesterase inhibitors could worsen motor symptoms. Studies have not shown this to be common, but patients should be monitored .
Pd Diagnosis Disease Severity And Disease Progression
The diagnosis of PD is essentially clinical , and we believe that the clinical evaluation of patients will not be replaced by modern imaging techniques. Nevertheless, as pointed out earlier, misdiagnosis can approach 20% of cases . Recently, in line with the European Union, the U.S. FDA approved DAT scan as a diagnostic tool to help differentiate between PD and Essential Tremor. This is the only current FDA-approved subsidiary examination to aid in PD diagnosis.
The role of magnetic resonance imaging in the diagnosis of PD is still not fully established. Traditionally, it has been seen as a means to potentially exclude alternate diagnoses such as vascular parkinsonism, or more importantly , atypical forms of degenerative parkinsonism such as MSA or progressive supranuclear palsy . Traditional structural MRI findings of these latter diagnoses such as increased pallidal iron, rim of putaminal hyperintensity, hot cross bun sign and/or cerebellar atrophy in MSA or the hummingbird or penguin sign in PSP may not be reliable, particularly in early disease.
Figure 5. Multimodal MRI in PD. Differences are noted between patients with PD and controls through voxel-based analysis of R2, mean diffusivity, and fractional anisotropy maps.
Brent A. Vogt, in, 2019
You May Like: Joy Milne Parkinson’s Disease
Diagnosis Of Parkinson Disease: Motor Symptoms
The clinical diagnosis of Parkinson’s disease is based on the presence of characteristic motor symptoms: bradykinesia, rigidity, postural instability, and resting tremor but neuropathology is still considered the gold standard for definite diagnosis. Differentiating PD from other movement disorders can be challenging throughout the disease course, because signs and symptoms often overlap. Indeed, neuropathology studies reveal that clinical diagnosis of PD can be confirmed with an accuracy of about 75%. Good response to levodopa is often used to support the diagnosis of PD. However, cases of pathologically proven PD with poor response to levodopa have also been reported.
Misdiagnosis of PD can occur for several reasons. In a community-based study of patients taking antiparkinsonian medication, the most common misdiagnosis were essential tremor, Alzheimer’s disease, and vascular parkinsonism. In addition, many of the prominent features of PD may also occur as a result of normal aging or from comorbid and multifactorial medical conditions .
R. Savica, … G. Logroscino, in, 2016
What Doctors Look For When Diagnosing Parkinsons
Certain physical signs and symptoms noticed by the patient or his or her loved ones are usually what prompt a person to see the doctor. These are the symptoms most often noticed by patients or their families:
-
Shaking or tremor: Called resting tremor, a trembling of a hand or foot that happens when the patient is at rest and typically stops when he or she is active or moving
-
Bradykinesia: Slowness of movement in the limbs, face, walking or overall body
-
Rigidity: Stiffness in the arms, legs or trunk
-
Posture instability: Trouble with balance and possible falls
Once the patient is at the doctors office, the physician:
-
Takes a medical history and does a physical examination.
-
Asks about current and past medications. Some medications may cause symptoms that mimic Parkinsons disease.
-
Performs a neurological examination, testing agility, muscle tone, gait and balance.
Read Also: Effect Of Exercise On Parkinson’s Disease
Medications For People With Parkinsons Disease
Symptoms of Parkinsons disease result from the progressive degeneration of nerve cells in the brain and other organs such as the gut, which produce a neurotransmitter called dopamine. This causes a deficiency in the availability of dopamine, which is necessary for smooth and controlled movements. Medication therapy focuses on maximising the availability of dopamine in the brain. Medication regimes are individually tailored to your specific need. Parkinsons medications fit into one of the following broad categories:
- levodopa dopamine replacement therapy
- dopamine agonists mimic the action of dopamine
- COMT inhibitors used along with levodopa. This medication blocks an enzyme known as COMT to prevent levodopa breaking down in the intestine, allowing more of it to reach the brain
- anticholinergics block the effect of another brain chemical to rebalance its levels with dopamine
- amantadine has anticholinergic properties and improves dopamine transmission
- MAO type B inhibitors prevent the metabolism of dopamine within the brain.
What Lifestyle Changes Can I Make To Ease Parkinsons Symptoms
Exercise: Exercise helps improve muscle strength, balance, coordination, flexibility, and tremor. It is also strongly believed to improve memory, thinking and reduce the risk of falls and decrease anxiety and depression. One study in persons with Parkinsons disease showed that 2.5 hours of exercise per week resulted in improved ability to move and a slower decline in quality of life compared to those who didnt exercise or didnt start until later in the course of their disease. Some exercises to consider include strengthening or resistance training, stretching exercises or aerobics . All types of exercise are helpful.
Eat a healthy, balanced diet: This is not only good for your general health but can ease some of the non-movement related symptoms of Parkinsons, such as constipation. Eating foods high in fiber in particular can relieve constipation. The Mediterranean diet is one example of a healthy diet.
Preventing falls and maintaining balance: Falls are a frequent complication of Parkinson’s. While you can do many things to reduce your risk of falling, the two most important are: 1) to work with your doctor to ensure that your treatments whether medicines or deep brain stimulation are optimal and 2) to consult with a physical therapist who can assess your walking and balance. The physical therapist is the expert when it comes to recommending assistive devices or exercise to improve safety and preventing falls.
Recommended Reading: Is Beer Good For Parkinson’s