Multiple System Atrophy Formerly Called Shy
As predicted by the name of this parkinsonism, multiple system atrophy affects multiple systems of the body. It affects both the motor skills movement system and the involuntary system of the body. Though the symptoms can often be treated with medications, there is no cure. In addition, there are no drugs that are able to slow the progress of MSA.
Whats The Difference Between Vascular Parkinsonism And Parkinsons
As the name implies, vascular parkinsonism is caused by cerebrovascular disease which affects the blood supply to the brain. Vascular parkinsonism is caused by one or more small strokes, while Parkinsons is caused by a gradual loss of nerve cells. One major difference from Parkinsons is that its not progressive, while Parkinsons becomes worse with time. Another difference is that there are no tremors in vascular parkinsonism.
For more information on vascular parkinsonism, read this journal article.
A Reappraisal Of The Ten Steps Test For Identifying Atypical Parkinsonism
Clinical Neurology and Neurosurgery 2014, 119: 1-3
INTRODUCTION: Gait abnormalities are prominent in atypical parkinsonian disorders and clinical signs such abnormal tandem walk have been suggested as a red flag for differential diagnosis. The objective is to determine the sensibility and specificity of the ten-steps test to discriminate atypical parkinsonisms from Parkinson’s disease.
METHODS: A sample of subjects with a parkinsonian disorder was evaluated. The ten-steps test was applied to all subjects. A Bayesian analysis model was used to calculate sensibility and specificity.
RESULTS: A total of 32 subjects with atypical parkinsonism and 54 subjects with Parkinson’s disease were included. Abnormal tandem gait had a sensitivity of 90.6% and specificity of 66.6% to differentiate between groups. When adjusted to the actual atypical parkinsonism prevalence the positive predictive value fall from 61.7% to 13.8%.
Full Text Links
Find Full Text Links for this Article
Also Check: Community Resources For Parkinson’s Disease
Early Freezing Of Gait: Atypical Versus Typical Parkinson Disorders
Abraham Lieberman
1Muhammad Ali Parkinson Center , Barrow Neurological Institute, St. Josephs Hospital and Medical Center, Phoenix, AZ, USA
Abstract
In 18 months, 850 patients were referred to Muhammad Ali Parkinson Center . Among them, 810 patients had typical Parkinson disease and 212 had PD for 5 years. Among the 212 patients with early PD, 27 had freezing of gait . Forty of the 850 had atypical parkinsonism. Among these 40 patients, all of whom had symptoms for 5 years, 12 had FOG. FOG improved with levodopa in 21/27 patients with typical PD but did not improve in the 12 patients with atypical parkinsonism. FOG was associated with falls in both groups of patients. We believe that FOG unresponsive to levodopa in typical PD resembles FOG in atypical parkinsonism. We thus compared the 6 typical PD patients with FOG unresponsive to levodopa plus the 12 patients with atypical parkinsonism with the 21 patients with typical PD responsive to levodopa. We compared them by tests of locomotion and postural stability. Among the patients with FOG unresponsive to levodopa, postural stability was more impaired than locomotion. This finding leads us to believe that, in these patients, postural stability, not locomotion, is the principal problem underlying FOG.
1. Introduction
2. Materials and Methods
| Patient demographics | |
| Hoehn and Yahr stage 4 | 7/18 |
3. Results
4. Discussion
Conflict of Interests
Acknowledgments
References
Copyright
More related articles
Role Of Imaging In The Differential Diagnosis Of Parkinsonism
Metabolic or structural imaging may improve the accuracy of clinical diagnosis for the various forms of parkinsonism. In particular, several SPECT tracers for dopamine transporter imaging have become widely available and allow early differentiation of PD from other tremor syndromes or vascular parkinsonism as discussed above . However, DaTSCAN as a marker of presynaptic dopaminergic degeneration is not suitable to differentiate PD from atypical parkinsonism. Recently, FDG-PET analysis using sophisticated statistical methods reliably discriminates between PD, PSP and CBS, and may improve the diagnostic accuracy of PD by around 20% and several years before clinical diagnosis is certain . The major disadvantage of PET is its high cost and the limited availability of the PET cyclotron.
Figure 1
Brain MRI in sagittal plane of a patient with progressive supranuclear palsy . Note the marked midbrain atrophy adopting the appearance of a hummingbird .
Don’t Miss: Cleveland Clinic Parkinson’s Doctors
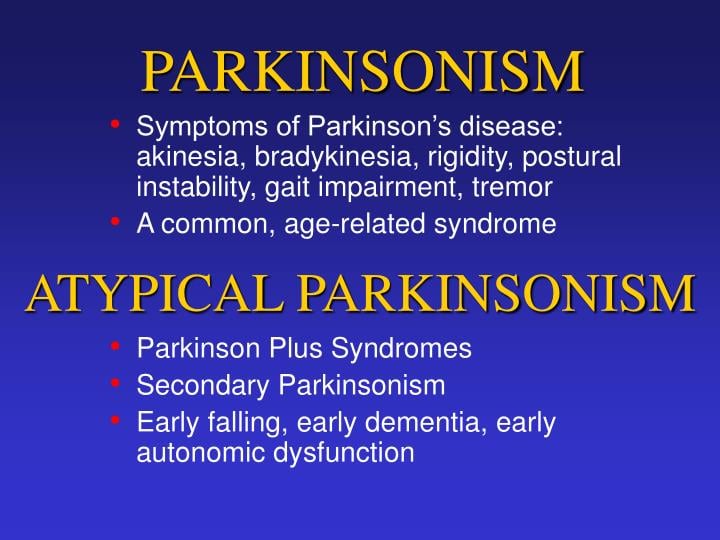
Parkinsonism: Cardinal Features Of A Neurological Syndrome
Parkinsonism is a neurological syndrome with four cardinal signs: bradykinesia, muscle rigidity, tremor at rest and impairment of postural reflexes. The diagnosis depends on the presence of bradykinesia, which denotes slowness of movements with a characteristic decrement on repetition . Related symptoms are deterioration of handwriting , slowing of walking , loss of facial expression and speech volume . A key feature of bradykinesia is the difficulty of performing automatic sequential and simultaneous movements, which is essential for habitual motor control in activities of daily living . Dopamine depletion of nigrostriatal pathways, ultimately leading to underactivation of basal ganglia thalamo-cortical loops, reflects the pathophysiological basis . Recently, the motor impairment of bradykinesia has been conceptualised within the frame of a dual behavioural control system: a habitual and a goal-directed system . The former is characterised by rapid and parallel processing and the latter by slow and serial processing. Accordingly, in the parkinsonian state patients, due to the disrupted habitual loop, depend significantly more on activation of the relatively intact goal-directed system. Thus, usually highly automated movements such as walking lose their implicitness and become goal-directed, thereby requiring substantial attention resources. As a consequence, parkinsonian patients are trapped in an arduous goal-directed motor control .
Differentiation Of Parkinsons Disease And Secondary Parkinsonism
Differentiating primary from secondary causes of parkinsonism relies chiefly on taking of a detailed medical history and careful clinical examination. The most common secondary causes are vascular white matter disease , which usually manifests with gait problems including freezing of gait with absent or only mild parkinsonian signs of the upper extremities and drug-induced parkinsonism, which should be suspected in patients treated with dopamine antagonists. Other toxic causes as well as Wilsons disease are uncommon but also important to recognise because they can be reversible or treatable. Since secondary parkinsonism is not the focus of this review, we will not further elaborate on it. In the vast majority of cases secondary causes can be ruled out clinically and with knowledge of the natural history of PD. Whenever doubts on the primary cause arise, either from the history, the clinical exam or the documented lack of levodopa response, further tests are indicated.
Don’t Miss: Management Of Parkinson’s Disease
Phase : Screening Questionnaire
The VIPD-Q was developed by neurologists and ophthalmologists to detect a broad range of ophthalmologic disorders in PD patients. It is based on an extensive literature study, previous questionnaires, and common and disabling visual disorders in both PD patients and healthy older people . The questionnaire includes 22 questions on visual problems, plus a standard set of demographic data . Answers are given on a 4-point Likert scale ranging from never have problems to daily problems, without possibility to give a neutral answer. As a second step, we grouped the questions according to the anatomical location of a visual disorder. These domains were agreed upon by a consensus procedure involving three independent ophthalmologists . They were asked to categorize the questions in four domains . Consensus was reached during a meeting with the three ophthalmologists. Six questions could not be categorized in one domain, but rather indicate the involvement of more than one anatomical domain. The VIPD-Q is designed as a patient self-scoring instrument and takes about 20min to complete.
Table 1 Domains and corresponding questions with possible diagnosis
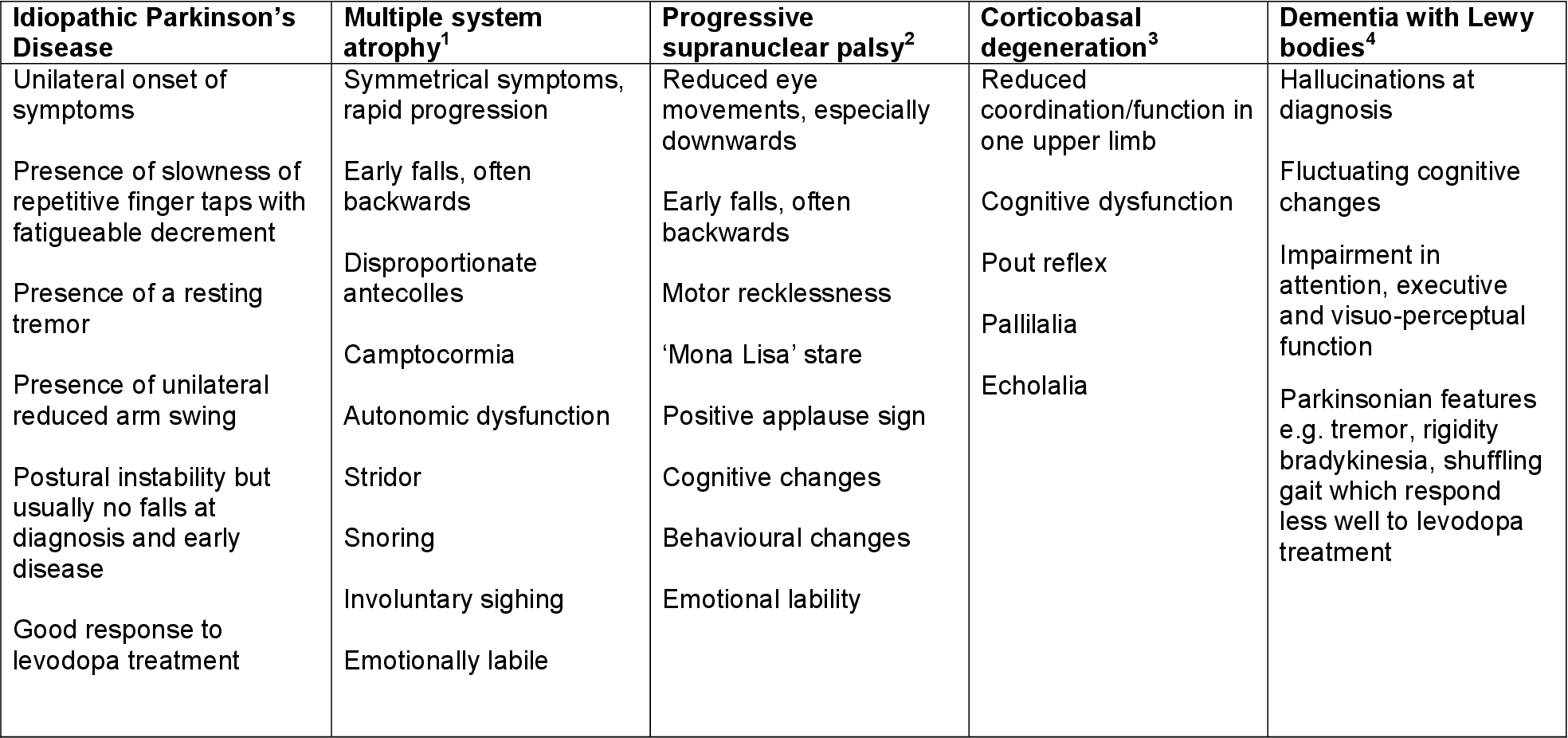
Differentiation Of Parkinsons Disease And Atypical Parkinsonism
A major confounder in the early clinical diagnosis of PD is atypical parkinsonism. A clinico-pathological study has shown that a diagnostic accuracy of over 90% can be achieved by strict application of clinical criteria, but only at the cost of missing 32% of true PD cases . Differentiation of PD and atypical parkinsonism is important, as the response to dopaminergic treatment is excellent in PD, but only poor or rapidly weaning in atypical parkinsonism . Dopaminergic drugs may even be harmful by potentially worsening atypical features such orthostatic hypotension or confusion in cognitively impaired patients . Also, patients with atypical parkinsonism should not be treated by deep brain stimulation , which is an effective treatment for PD only . Finally, prognosis is better in PD, whereas atypical parkinsonism is generally associated with more rapid progression .
| Table 2: Oculomotor signs in parkinsonism. |
| Probably, late |
| PD = Parkinsons disease, PSP = progressive supranuclear palsy, CBD = corticobasal degeneration, MSA = multiple system atrophy, DLB = dementia with Lewy bodies, RS = Richardson syndrome, MSA-C = cerebellar variant, *may be slowed late, ** may be slowed horizontally. |
Don’t Miss: Why Is There No Cure For Parkinson’s Disease
Whats The Difference Between Progressive Supranuclear Palsy And Parkinsons
People with PSP generally progress more rapidly than people with Parkinsons. A person with Parkinsons tends to lean forward while a person with PSP tends to lean backward. Tremors are common in people with Parkinsons and rare in people with PSP. Speech and swallowing abnormalities are more severe and show up sooner in those living with PSP.
For more information on progressive supranuclear palsy, read this fact sheet and insights from the CurePSP organization website.
Dementia With Lewy Bodies
Dementia with Lewy bodies causes movement problems such as tremor, slowness and stiffness and significant thinking andmemory problems . DLB dementia affects thinking more than memory, and people have difficulty processing information, following steps in a process and seeing things in three dimensions to make a mental picture of their surroundings. In DLB, dementia and movement symptoms typically come on at the same time or within a year of each other.
DLB is related to Parkinsons disease dementia , which also causes dementia and movement symptoms. People with PDD first show movement symptoms and, after many years or decades of living with Parkinsons, develop dementia. Because DLB and PDD share symptoms and brain cell changes , doctors and researchers group them under the umbrella term Lewy body dementia. After Alzheimer’s disease, Lewy body dementia is the second most common cause of neurodegenerative dementia.
In addition to dementia and movement problems, Lewy body dementia can cause:
- Visual hallucinations and delusions
- Fluctuating attention and alertness
- Acting out dreams and other sleep problems
- Mood changes, such as depression or anxiety
- Behavioral changes, such as agitation or aggression
- Loss of motivation
- Blood pressure changes
Researchers are working out exactly why Lewy body dementia occurs. Genetics, environmental factors and aging all likely play a role.
You May Like: Medications For Parkinson’s Disease And Side Effects
What Are The Symptoms Of Atypical Parkinsonian Disorders
Like classic Parkinsons disease, atypical Parkinsonian disorders cause muscle stiffness, tremor, and problems with walking/balance and fine motor coordination.
Patients with atypical Parkinsonism often have some degree of difficulty speaking or swallowing, and drooling can be a problem. Psychiatric disturbances such as agitation, anxiety or depression may also be part of the clinical picture.
Dementia with Lewy bodies can cause changes in attention or alertness over hours or days, often with long periods of sleep during the day. Visual hallucinations typically of small animals or children, or moving shadows in the periphery of the visual field are common in DLB. DLB is second only to Alzheimers disease as a cause of dementia in the elderly, and it most commonly affects patients in their 60s.
Patients with progressive supranuclear palsy may have difficulties with eye movements, particularly when looking downward, and with balance when descending stairs, for instance. Backward falls are common and may occur during the early course of the disease. PSP is not usually associated with tremor, unlike Parkinsons disease.
Parkinson’s Disease and Movement Disorders Center
Pathogenesis Underlying Neurodegeneration In Parkinsonism
Aggregation of misfolded proteins is considered a hallmark of the neurodegenerative process in parkinsonism. Therefore, parkinsonian disorders are conceived as proteinopathies involving two main types of protein: Tau and -synuclein. Accordingly, proteinopathies are subdivided into Tauopathies and -synucleinopathies. Tau is a microtubule-associated protein playing an important role in axonal transport. There are several isoforms comprising two main groups classified according to the repeat numbers in the microtubule-binding domain: 4 repeat and 3 repeat Tau. The former is prevalent in PSP, CBD and FTDP 17 and the latter in Picks disease. The PSP and CBS phenotype is highly specific for tauopathies . -Synuclein is a presynaptic protein whose function is unknown. Neuronal accumulation of -synuclein defines PD and LBD while glial deposition is characteristic of MSA . Hence this molecular pathological classification corresponds to specific phenotypic disorders and may influence clinical nosology in the future. Type and distribution of neuropathology determines clinical presentation . For instance, 4R tauopathy predominant brainstem distribution is characteristic for PSP-P whereas predominant cortical deposition of -synuclein containing Lewy bodies typifies LBD.
Don’t Miss: How Do They Test You For Parkinson’s Disease
Article / Publication Details
Number of Print Pages: 16Number of Figures: 2
Whats The Difference Between Dementia With Lewy Bodies And Parkinsons
In dementia with Lewy bodies, dementia always appears first. There can also be changes in alertness as well as visual hallucinations. However, because of the presence of Lewy bodies throughout the entire brain, characteristics of this disease not only include cognitive characteristics, but also physical, sleep, and behavioral changes. As the disease progresses, the motor symptoms common to Parkinsons such as tremor, slowness, stiffness, and walking and balance problems will appear.
For more information on dementia with Lewy bodies, visit www.lbda.org.
Also Check: Young Onset Parkinson’s Symptoms
Ten Steps To Identify Atypical Parkinsonism
- Medicine
- Journal of Neurology, Neurosurgery & Psychiatry
- 2011
- 2017
- View 5 excerpts, cites results, methods and background
- 2012
- View 1 excerpt, cites background
- Arquivos de neuro-psiquiatria
- 2011
- Zhurnal nevrologii i psikhiatrii imeni S.S. Korsakova
- 2016
- Psychology
- 2016
- Arquivos de neuro-psiquiatria
- 2011
- The Lancet
- 2011
- The Lancet
- 2011
- Archives of clinical neuropsychology : the official journal of the National Academy of Neuropsychologists
- 2017
Types Of Atypical Parkinsonism
Atypical Parkinsonism has several forms or types that are known to co-occur with Parkinsons disease symptoms. These include:
- Corticobasal degeneration : People with this condition experience stiffness in the extremities, sudden muscle jerking, and problems carrying out purposeful movements, such as reaching or grasping an object .
- Dementia with Lewy bodies : Men older than age 50 with a family history of Parkinsons are most likely to have DLB. This condition causes early dementia as well as visual hallucinations.
- Progressive supranuclear palsy : PSP is the most common form of atypical Parkinsonism. The disease can affect a persons ability to look up and down and can cause postural instability that leads to frequent falls. This condition is associated more with women and people older than 60.
- Multiple system atrophy : MSA is the second most common form of atypical Parkinsonism. The condition causes unstable blood pressure and reddish skin discoloration, as well as bladder, bowel, and sexual dysfunction.
- Normal pressure hydrocephalus : This condition results in an excess of cerebrospinal fluid that causes a person to experience symptoms such as difficulty walking, incontinence, and dementia.
- Vascular Parkinsonism: This condition causes a person to have many lower body symptoms, such as problems with walking and balance. A person will also have problems with blood flow, which can lead to stroke and mini-strokes.
Read Also: Mucuna Plants For Parkinson’s Disease
Whats The Difference Between Corticobasal Degeneration And Parkinsons
The main difference between CBD and Parkinsons is that it usually starts on one side with the gradual loss of use of one hand or leg , and there may be little flicks of involuntary muscle jerks. Walking and balance difficulties usually occur later in CBD than in Parkinsons. Also, in CBD, a person may have trouble with purposeful movements, such as buttoning a shirt or cutting food.
For more information on corticobasal degeneration, read this information page.
Treatment Of Atypical Parkinsonism
While no current therapy can slow or stop progression, treatment can ease symptoms of atypical parkinsonisms. Because symptoms overlap across these conditions, treatments overlap, too.
For movement symptoms, such as stiffness and slowness, doctors may prescribe levodopa. Unfortunately, if this medication does ease symptoms, its benefit may not be significant or long-lasting. In people who have dementia with Lewy bodies, levodopa may worsen hallucinations, so doctors prescribe it cautiously. For dystonia in CBD, botulinum toxin injections such as Botox or Myobloc into the muscles may be an option. For walking and balance problems, as well as falls, occupational and physical therapy are helpful. Canes and walkers may provide extra stability, though in some cases wheelchairs may be necessary.
Memory and thinking problems may be treated with medications such as Exelon , Aricept , Razadyne or Namenda . In DLB, these drugs also may help with behavioral changes and hallucinations.
Speech therapy treats speech and swallowing problems. Therapists may recommend exercises to strengthen speech and swallowing muscles, as well as diet adjustments and behavioral strategies to improve swallowing. If swallowing problems lead to weight loss or recurrent pneumonia , doctors may consider a feeding tube.
Doctors can use a variety of medications to ease mood, behavioral and sleep problems.
Also Check: Actor With Parkinson’s Disease