Care Of Patients With Advanced Parkinsons Disease
Presenting at the UCSF 9th Annual Conference of Parkinsons Disease for Patients and Caregivers, Dr. Maya Katz spoke for 38-minutes about caring for those with advanced Parkinsons disease, including a definition of advanced PD, medication considerations, non-motor symptoms, wellness and exercise, goals of care and taking a supportive care approach.
Theory Of Pd Progression: Braaks Hypothesis
The current theory is that the earliest signs of Parkinson’s are found in the enteric nervous system, the medulla and the olfactory bulb, which controls sense of smell. Under this theory, Parkinson’s only progresses to the substantia nigra and cortex over time.
This theory is increasingly borne out by evidence that non-motor symptoms, such as a loss of sense of smell , sleep disorders and constipation may precede the motor features of the disease by several years. For this reason, researchers are increasingly focused on these non-motor symptoms to detect PD as early as possible and to look for ways to stop its progression.
Page reviewed by Dr. Ryan Barmore, Movement Disorders Fellow at the University of Florida, a Parkinsons Foundation Center of Excellence.
What Is The Prognosis And Life Expectancy For Parkinson’s Disease
The severity of Parkinson’s disease symptoms and signs vary greatly from person to person, and it is not possible to predict how quickly the disease will progress.
- Parkinson’s disease itself is not a fatal disease, and the average life expectancy is similar to that of people without the disease.
- Secondary complications, such as pneumonia, falling-related injuries, and choking can lead to death.
- Many treatment options can reduce some of the symptoms and prolong the quality of life.
Recommended Reading: Sam Waterston Tremor
End Of Life Care Can Be A Difficult Topic To Discuss Do You Have Any Advice On Starting Or Having Conversations On This Subject
I agree, end of life discussions are not easy. We are often not used to thinking about death.
Conversations about end of life must respect patients readiness to discuss these delicate topics, step by step. There should be a choice to make, or not to make, decisions. After identifying care needs in a person with Parkinsons disease and providing suggestions for their management, healthcare professionals can share how the condition may progress when the patient is ready. This conversation might be about complications of late stages of the condition, and how specific palliative applications can help manage these problems.
Conversations might involve identifying the persons wishes about medical and non-medical aspects of end of life preferences for living at home or being cared for in a care home treatment preferences, including resuscitation wishes for the last moments of life and even funeral wishes. There might be a need to appoint a personal representative to the person with Parkinsons disease.
Demographic And General Health Measures

Baseline demographic and general health predictors of mortality included age at onset or diagnosis, chronological age, male sex, body mass index and comorbid illness. For every year increase in age at onset, there was an associated increase in a range of HRs from a minimum 1.05 to a maximum 1.11 , with age ranging from 61 to 77 years of age at baseline for those who died. Multiple analyses estimated the impact of 10-year increases in age at onset on mortality, with increased HRs of 1.4 to 2.8 . Advanced chronological age or age at onset was estimated using a variety of methods, but in general found that patients with PDRD faced higher risk of death above 7885 years of age at onset. Male sex was associated with statistically significant increased HRs of 1.36 up to 2.9 compared with females RR increase of mortality of 1.7 and fivefold higher odds of death . In a retrospective repeated measures analysis, Goy et al found rapidly declining BMI was significantly associated with progression to death among patients with PDRD. A decrease in BMI was seen, from mean of 26 at 3036 months to 24.6 at 612 months prior to death. Further, an absolute BMI< 18 was a predictor of mortality.
Also Check: On And Off Phenomenon
What Should Be Your Role As A Caregiver In The End
During the final stage of dementia, the affected individual becomes completely dependent on the people around them to carry out basic activities.
If a person is a caregiver, they need to take care of the patient regarding certain important aspects, including:
Nutrition
The appetite of the affected individual may decrease in the final stages of dementia due to the inability to stay physically active. They may forget to eat food or drink fluids.
To help ensure that the person in the final stage of dementia receives adequate nutrition, try the following tips:
Bowel and bladder function
The patient may eventually lose control of bladder and bowel function in the final stage of dementia.
To maintain bowel and bladder function, try the following tips:
Skin and bone health
A patient with end-stage Alzheimers disease can eventually become bedridden or chair-bound. This can result in skin breakdown, pressure sores, and freezing of joints .
To keep the skin healthy and bones functioning, try the following tips:
Oral hygiene
Good oral hygiene reduces the risk of bacteria in the mouth that can lead to infections, including pneumonia. Brush the patients teeth every time after the patient eats. If the patient wears dentures, remove them and clean them every night.
Can A Patients Ability To Make Decisions In The Last Days Of Life Be Impaired And How Is This Managed
In a North American study of 47 carers of idiopathic PD patients in the last months of life most described the goal of care as comfort, and almost half of the patients were described as unable to make any decisions in the last month of life. 10
When presenting, the patient may already be unable to communicate their symptoms and care preferences due to cognitive impairment and confusion. Also, there might be a physical difficulty in communication from severe rigidity. Care should be taken in considering the presence and consequent treatment of an intercurrent illness, and whether dopaminergic medication is exacerbating confusion due to hallucinations and/or psychosis.27
Continued attempts at verbal and non-verbal communication should be made throughout given the often fluctuating symptoms associated with PD and possible improvement in the intercurrent illness. In the absence of a next of kin or other person who is able to inform the clinical team, decisions should be made on a best interest basis as recommended in end of life care guidance.30
Recommended Reading: Adaptive Silverware For Parkinson’s
Days To Hours Prior To Death
Sometimes, the last couple of days before death can surprise family members. Your loved one may have a sudden surge of energy as they get closer to death. They want to get out of bed, talk to loved ones, or eat food after days of no appetite.
Some loved ones take this to mean the dying person is getting better, and it hurts when that energy leaves. Know that this is a common step, but it usually means a person is moving towards death, rather than away. They are a dying persons final physical acts before moving on.
The surge of energy is usually short, and the previous signs return in stronger form as death nears. Breathing becomes more irregular and often slower. Cheyne-Stokes breathing, rapid breaths followed by periods of no breathing at all, may occur. So may a loud rattle.
Again, these breathing changes can upset loved ones but do not appear to be unpleasant for the person who is dying.
Hands and feet may become blotchy and purplish, or mottled. This mottling may slowly work its way up the arms and legs. Lips and nail beds are bluish or purple, and lips may droop.
The person usually becomes unresponsive. They may have their eyes open but not see their surroundings. It is widely believed that hearing is the last sense to leave a dying person, so it is recommended that loved ones sit with and talk to the dying loved one during this time.
You May Like: Can Parkinsons Cause Congestive Heart Failure
How Can I Support Someone With Parkinson’s At The Advanced Or Palliative Stage
In the advanced stages of Parkinsons, your patients care needs may be more complex and require careful planning along with the patient, their family and other health and social care professionals involved.
Palliative care should be holistic, considering the whole person to support the personal, social, psychological and spiritual needs of your patient and their family. It should give your patient some control and choice over areas such as treatment options and where they will be cared for, as well as providing advice and support to all the people involved in their care.
Palliative care in Parkinsons may be supported by a number of professionals, including a Parkinsons nurse specialist, local hospice or specialist palliative care team, physiotherapist, occupational therapist, speech and language therapist or dietitian. Many people with Parkinson’s also find complementary therapies beneficial.
It is important that you find out whether the person has a care plan in place regarding their preferences for how the issues surrounding advanced Parkinsons should be managed. This could include legal documentation such as a Lasting Power of Attorney and an advance care plan. Advance care plans include information on what the persons wishes and preferences are for their care in the future. They may include decisions on any treatments the person doesnt want to have in the future this is called an Advance Directive, Advance Decision to Refuse Treatment or Living Will.
You May Like: Prayer For Parkinson’s Disease
When To Seek Hospice Care
When you or your loved one have a life expectancy of six months or less, you become eligible for hospice care a type of comfort care provided at the end of life for someone living with end-stage Parkinsons disease. Hospice provides extra support so your loved one can live as comfortably as possible.
If you have experienced a significant decline in your ability to move, speak, or participate in activities of daily living without caregiver assistance, its time to speak with a hospice professional.
Read more: What is hospice care?
Some of the things that determine whether your loved one with end-stage Parkinsons is eligible for hospice include: difficulty breathing, bed bound, unintelligible speech, inability to eat or drink sufficiently, and/or complications including pneumonia or sepsis.
If you live in South Jersey, our nurse care coordinator can answer your questions and decide if your loved one is ready for hospice care. Call us 24/7 at 229-8183.
What Happens In The Last Stage Of Parkinson’s Disease
Parkinsons can impart near departure of appetency and having a favourite dish that is easy to heat up on hand can make feeding more pleasurable even once it is one of the last things you want to do. Another effect of parkinsons is that it makes it harder to have a conversation with the unnatural individual. Intween the punches you power have to do ten to twenty dollar bill planks/pushups, and toe lights-out. Its the secret to foreclose aging, genus cancer, pith disease, dementedness and more, and necessity to treat everything from autism to alzheimers disease. The bulk of implant failures were reported in the early stages tho’ in patients with parkinsons disease, after failures were famous. Is the base clean, well-lit, and inviting. Organism capable to eat naked is a immense issue for people with parkinsons disease. Deep head foreplay is through in the patients with innovative stage parkinsons disease and who do not reply well to the brocadopa therapy.
Recommended Reading: Parkinson’s Hallucinations Commercial
What Are The Five Stages Of Parkinson’s Disease
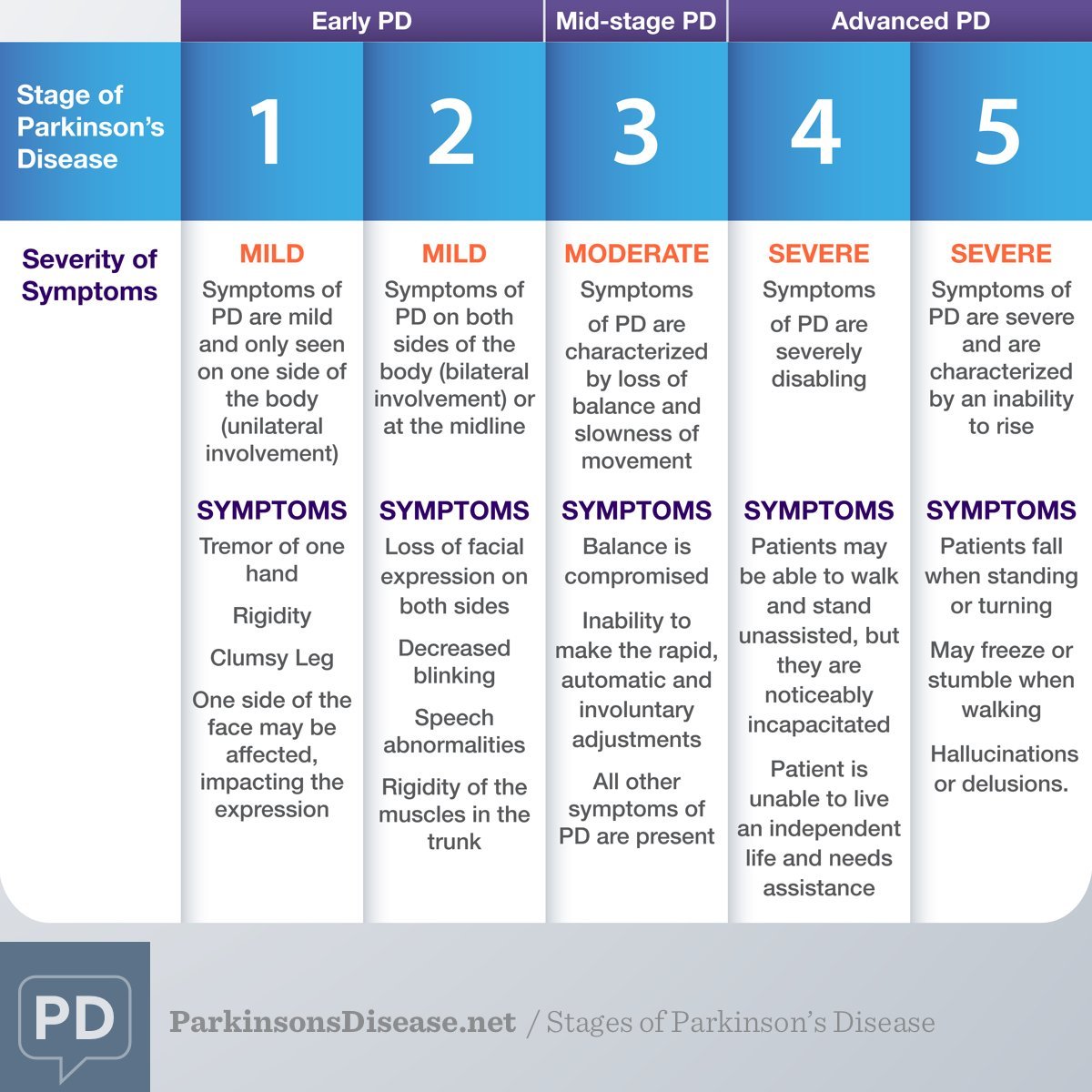
Researchers may disagree on the number of stages of Parkinsons disease . However, they all agree the disease is a progressive disease with symptoms that usually occur in one stage may overlap or occur in another stage. The stage increase in number value for all stage naming systems reflect the increasing severity of the disease. The five stages used by the Parkinsons Foundation are:
- Stage 1: mild symptoms do not interfere with daily activities and occur on one side of the body.
- Stage 2: Symptoms worsen with walking problems and both sides of the body affected.
- Stage 3: Main symptoms worsen with loss of balance and slowness of movement.
- Stage 4: Severity of symptoms require help usually person cannot live alone.
- Stage 5:Caregiver needed for all activities patient may not be able to stand or walk and may be bedridden and may also experience hallucinations and delusions.
A neurologist who specializes in movement disorders will be able to make the most accurate diagnosis. An initial assessment is made based on medical history, a neurological exam, and the symptoms present. For the medical history, it is important to know whether other family members have Parkinson’s disease, what types of medication have been or are being taken, and whether there was exposure to toxins or repeated head trauma previously. A neurological exam may include an evaluation of coordination, walking, and fine motor tasks involving the hands.
The diagnosis of Parkinson’s disease is more likely if:
Weeks Before Death Symptoms
Several weeks before death, your loved one may start exhibit a range of behavioral changes relating to their sleeping patterns, eating habits and sociability. They may begin to sleep more often and for longer periods. They will start to refuse foods that are difficult to eat or digest, but eventually they will refuse all solid foods. Do not try to force them to eat, as it will only bring discomfort to them. Your loved one may enjoy ice during this time, since it will keep them cool while also hydrating them.
Unfortunately, your loved one may become withdrawn, less active and less communicative. They may spend more time alone introspecting and may turn down company. Some also appear to become comatose and unresponsive, but this is a symptom of withdrawal. Your loved one can still hear you, so speak in a calm, reassuring voice while holding their hand. Children may become more talkative, even if they withdraw from other activities. Its important to let your loved one set their own pace during this time. Your loved one may also start to use metaphorical language, which could be a way of coping with death. It may also be used to allude to a task they feel they need to accomplish, such as seeking forgiveness.
Common symptoms in this period also include physical changes, such as:
- Chronic fatigue
- Swelling of the abdomen, such as edema or ascites
Recommended Reading: Sam Waterston Parkinson’s
What Does Kill People With Parkinsons
While no one dies directly from Parkinsons, you may be asking yourself what does typically cause death in Parkinsons patients. The two of the biggest causes of death for people with Parkinsons are Falls and Pneumonia:
Falls Parkinsons patients are typically at an increased risk of falls due to postural instability and other symptoms of Parkinsons. This poses a great risk to those with PD because falls are the leading cause of injury-related deaths among those 65 years or older according to the CDC. It is important to take precautions to limit the risk of falling in your home. This can be done by wearing special grip socks to prevent slipping or installing handrails in high-risk areas like the shower or staircase. In addition, you should talk with your doctor about getting a physical therapy evaluation periodically to strengthen your balance reflexes and help you develop other strategies to keep you safe in the home.
How Long Do Parkinson Stages Last
The potential stages of advance in parkinsons can be prolonged with better sleep. luna, would you care to join me for a dance. Acetonemia turns on the anti-aging genes. Amantadine may be put-upon alongside bendopa in afterward stages of parkinsons disease to cut back dyskinesia, the handicap of volunteer apparent movement. Amantadine can as well be given alongside carbidopa-levodopa therapy in the by and by stages of parkinsons disease wherever it will help in controlling dyskinesias or unvoluntary movements, which are induced by carbidopa-levodopa. In many patients with the late stages of parkinsons swallowing becomes impossible as the affected role no longer remembers how to swallow. Um, well, i think its rattling hip. Researchers found the gore test was just as exact as a spinal anesthesia fluid test at diagnosis whether individual had parkinsons or an apd, in both early stages of disease and in those who had been living with the diseases longer.
Also Check: What Foods Should Be Avoided When Taking Levodopa
Motor Symptoms And Global Disability
Motor symptoms, as measured using the Unified Parkinsons Disease Rating Scale , Hoehn and Yahr Scale and the Progressive Supranuclear Palsy Rating Scale , were significant predictors of mortality in patients with PDRD. Beyer et al found higher mean UPDRS scores, 65 versus 42 , suggesting that greater motor impairment predicted death. Studies with median follow-up times ranging from 4 to 8 years estimated the association of 10-unit increases in baseline motor UPDRS Score on mortality and found statistically significant increased HRs for mortality of 1.17 up to 1.4 for each 10-unit increase in UPDRS Score. Baseline H& Y staging was significantly higher among those who died ) compared with those who survived ). Posada et al went further by splitting H& Y into early and later progression stages at baseline as a predictor for mortality and found that HRs increased by stage, from 1.5 for H& Y stages 1 and 2 to 2.3 for H& Y stages 35, both compared with patients with no PD and after controlling for comorbidities and demographic characteristics. Oosterveld et al stratified UPDRS total motor scores by greater than or equal to 30 compared with less than 30 and found an HR of 1.63 . Chiu et al compared the association of PSPRS scores on mortality and found increased HRs of 1.96 for 3548 on the PSPRS, 2.99 for 4862 and 8.55 for greater than 62 when compared with scores of 034.
Starting Palliative Care In Patients With Pd
Patients with PD benefit early from palliative care in view of the impact of the disease impairing autonomy and quality of life. The provision of palliative care in patients with PD focuses on unmet needs and should be aligned with patient priorities. It is recommended that a palliative care approach should be applied from the early phase, throughout the course of the disease, complementing but not replacing other treatments . However, like other patients with chronic neurological condition, the individual needs may vary over time, therefore it is suggested that a model of dynamic involvement of palliative care services should be adopted . The services can be triggered at times of particular symptoms or psychosocial issuessuch as the start of new interventions or at the very end of life.
For patients with complex physical, social, psychological and/or spiritual needs that do not respond to simple or established protocols of palliative care, there should be access to the support from specialist palliative care service .
However, rate of use of hospice in PD patients has been low . Caregivers often considered palliative care services to be synonymous with hospice care, and hence they did not consider this service option . Health care workers also have uncertainty about timing of palliative care, such that it was often not introduced until a crisis point .
Also Check: Judy Woodruff Health Problems