Current Update On Clinically Relevant Sleep Issues In Parkinsons Disease: A Narrative Review
Article type: Review Article
Authors: Suzuki, Keisuke *
Affiliations: Department of Neurology, Dokkyo Medical University, Shimotsuga, Tochigi, Japan
Correspondence: Correspondence to: Keisuke Suzuki, MD, PhD, Department of Neurology, Dokkyo Medical University, 880 Kitakobayashi, Mibu, Shimotsuga, Tochigi 321-0293, Japan. Tel.: +81 282 86 1111 Fax: +81 282 86 5884 E-mail: .
Keywords: Parkinsons disease, sleep disturbances, excessive daytime sleepiness, REM sleep behavior disorder, restless legs syndrome, sleep apnea syndrome
DOI: 10.3233/JPD-202425
Journal: Journal of Parkinson’s Disease, vol. 11, no. 3, pp. 971-992, 2021
Abstract
Sleep: A Mind Guide To Parkinsons Disease
This 36-page booklet explains normal sleep patterns, the body clock, how much sleep we should get, challenges to sleeping well, tips for good sleep hygiene, and sleep in normal aging before discussing symptoms, diagnosis and treatment of sleep disorders, including insomnia, REM sleep behavior disorder, sleep apnea, restless leg syndrome, and daytime sleepiness.
Figuring Out Causes Of Fatigue
The first step in easing the fatigue associated with Parkinsons disease is to rule out other causes of tiredness, says Liana Rosenthal, M.D., assistant professor of neurology at the Johns Hopkins University School of Medicine and director of clinical core at the Morris K. Udall Center Parkinsons Disease Research Center of Excellence. We evaluate patients to see if there are other things contributing to the fatigue besides their disease, she says.
Sometimes patients may be referred to a sleep specialist for an evaluation. That can help identify causes of tiredness, like sleep apnea. Rosenthal says: Our aim is to first treat any sleep issues, like insomnia, sleep apnea or other causes of poor sleep. Once we treat and address those issues, we can see if fatigue still persists.
You May Like: Cleveland Clinic Parkinson’s Bicycle Study 2017
Frequency Of Sleep Disorders And Other Nocturnal Features
Table 11 presents the prevalence of sleep disorders and other nocturnal features in patients with PD in 1993, 1997 and 2001. More than 50% of the patients reported insomnia at each study visit. The frequency of problems with sleep initiation and frequent awakenings varied from 23% to 30% and from 23% to 44%, respectively. In all, 1924% of the patients reported early morning awakening during the study period. Problems turning in bed, vivid dreaming or nightmares, and EDS were also common complaints, and their frequency increased significantly over time, whereas rapid eye movement sleep behaviour disorder suspect features varied in prevalence. The proportion of patients who had discussed the sleeping problem with their general practitioner increased over the years. The use of sleeping pills varied little. Other problems like pain or cramps, dystonia and myoclonic jerks during the night occurred in < 20% of patients, and their frequencies were rather stable during the study period. Among patients with insomnia, it was only in 1993 that the occurrence of problems turning in bed was more common than that related to insomnia .
Table 1Prevalence of diurnal and nocturnal symptoms in patients with Parkinson’s disease over an 8year study period
| Patients with PD |
|---|
MADRS, Montgomery and Aasberg Depression Rating Scale MMSE, MiniMental State Examination PD, Parkinson’s disease UPDRS, Unified Parkinson’s Disease Rating Scale.
*p0.05.
**p0.005.
Changes In Sleeping Patterns

As Parkinsons progresses, you can also develop problems with sleep patterns. These may not happen in the early stages, but can be noticeable later. You might wake up often in the middle of the night or sleep more during the day than you do at night.
Another common sleep disturbance for people with Parkinsons is rapid eye movement sleep behavior disorder. This is when you start acting out your dreams in your sleep, such as verbally and physically, which can get uncomfortable if someone is sharing your bed. Dr. Rundle-Gonzalez says many times a bed partner will be the one to notice sleep problems.
REM sleep behavior disorder can also happen in people who dont have Parkinsons. However, if this isnt something youve dealt with before, its likely related to your disease. There are medications your doctor can prescribe to help you sleep comfortably through the night.
You May Like: Parkinson Silverware
Diagnostic Assessment Of Sleep Disorders In Pd
The history taken from the patient and its neighbors is very important in assessing sleep disorders in PD. The type of sleep disorder should be identified in the history, and information about possible related factors should be obtained from the history. In PD, general and specific scales can be used to investigate the subtype of sleep disorder and to determine its severity. Objective methods can be used to further investigate the diagnosis of these disorders. Further investigative techniques include sleep recording methods such as actigraphy or PSG. Polysomnographic findings of each sleep disorder have been explained in the relevant section. In addition, information about screening scales used in each sleep disorder has been described in the relevant section.
Actigraphy is an electrophysiological device that measures the movements of the patient during sleep by recording from wrist or ankle for many days. Actigraphy evaluates indirectly the circadian sleepwake patterns . It is especially used in circadian rhythm disorders or insomnia and prolonged daytime sleepiness .
What Else Can I Do To Sleep Better With Parkinsons Disease
Practicing healthy sleep hygiene habits may also promote more restful sleep.
- Get outside during the day. Bright light tells your body its time to be awake.
- Keep your body moving during the day. Even if all you feel up to is a short walk or two, all physical activity offers benefits.
- Try at-home remedies, such as massage or a warm bath. Relaxing your mind may help your body fall asleep.
Dont:
- Take long naps during the day.
- Use stimulants, such as caffeine, within six hours of bedtime.
- Use your bedroom for activities other than sleeping. Go to another room to read, watch TV or work.
Don’t Miss: Judy Woodruff Parkinson’s
What Types Of Sleep Problems Do People With Parkinsons Disease Have
Parkinsons disease affects every person differently. It also impacts sleep in different ways. People with Parkinsons may have:
- Insomnia, finding it hard to fall asleep.
- Fragmented sleep, waking up many times over the night.
- Excessive daytime sleepiness, finding it hard to stay awake during the day.
- Very vivid dreams, which may cause hallucinations or confusion after waking up.
- Emotional dreams or nightmares, which may make you feel emotionally drained after waking up.
Genetic Similarities Between Rbd And Pd
GBA mutations, which cause Gaucher disease, were more common in PD patients than in controls , and GBA mutations were associated with a 5.43-fold higher risk of PD . In addition, GBA mutations were more commonly found in idiopathic RBD patients than in healthy subjects , suggesting an association between RBD and GBA mutations. In other studies, PD patients with GBA mutations had more severe motor symptoms and higher rates of RBD, hallucinations and other nonmotor symptoms, such as depression and olfactory impairments, than PD patients without GBA mutations . Thus, GBA mutations may affect the clinical features of PD.
A study showed a significant association between Lewy-type alpha-synucleinopathy pathology and the prevalence of probable premortem RBD in various neurodegenerative diseases, including progressive supranuclear palsy . The association of RBD with MAPT is unclear . Interestingly, carriers of different haplotypes of LRRK2 mutations may have different risks of RBD: the p.N551K-p.R1398H-p.K1423K haplotype was associated with a lower risk of RBD, and the common variant p. S1647T was associated with an increased risk of RBD . Full sequencing and genotyping of SNCA in patients with iRBD, PD, and DLB and controls showed that a 5-region SNCA variant was associated with an increased risk of iRBD and probable RBD with PD . Zhao et al. recently found SNCA hypomethylation in leukocytes in patients with iRBD and PD.
You May Like: Zhichan Capsule
Sleep Disorders In Parkinson’s Disease By Amer G Aboukasm
Although the daytime clinical manifestation of Parkinson’s disease have been well recognized for almost two centuries, the nocturnal symptoms, which occur in as many as 75% of patients and the associated sleep disorders were not studied until the 1960s. A variety of psychological and physiological processes can lead to disruption of the normal rhythm of the sleep-wake cycle in patients with Parkinsonism. First, the degenerative process in Parkinson’s disease affects the neurophysiological and neurochemical systems responsible for sleep organization, thus results in disruption of sleep. Second, the motor, respiratory and behavioral phenomena accompanying the disease may produce nocturnal symptoms. Third, the medication used in its treatment may induce new symptoms, such as nightmares or nocturnal movements. All these effects on sleep have implications for treatment planning.
Parkinsons Disease Linked To Sleep Disorders Sleep Disturbances
Written byDevon AndrePublished onFebruary 9, 2016
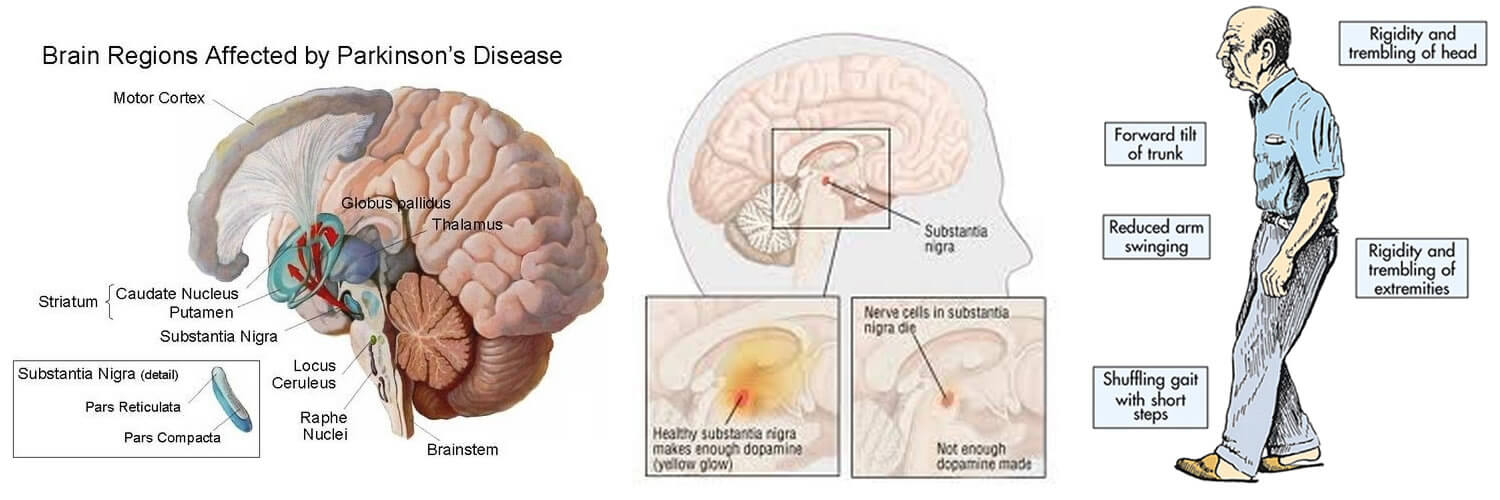
Parkinsons disease has been linked to sleep disorders and sleep disturbances. Parkinsons disease is characterized by the loss of brain cells that control movement. Symptoms of Parkinsons disease can include tremors, stiffness, slowness of movements, as well as balance and coordination problems. Memory problems, depression, and sleep problems can all occur in Parkinsons disease, too.
Sleep problems and sleep disorders may occur as an early sign of Parkinsons disease, even before motor symptoms have started. Common sleep disorders experienced in Parkinsons disease include insomnia, excessive daytime sleepiness, nightmares, sleep attacks, REM sleep behavior disorder , periodic leg movement disorder, restless leg syndrome, sleep apnea, and nocturia, which is frequent nighttime urination.
Don’t Miss: On Off Phenomenon
The Effect Of Exercise
Exercise has been shown to have a variety of beneficial impacts, and sleep is no exception. In fact, a study found that after four months of physical activity, adult insomniacs got an average of one extra hour of sleep per night. Exercise improves sleep quality, quantity, number of nighttime waking incidents and the time it takes to fall asleep. Sleep also gives you more energy and therefore contributes to a positive feedback loop of more exercise and more sleep.
From preventing against cancer to improving your learning capabilities to making cool-headed decisions, consistent and proper sleep habits can offer a wide range of positive effects. But even if you know how important sleep is, when youre having trouble sleeping, what can you do to fix it?
The number of reported cases of sleep issues has increased dramatically in recent years. There are a variety of underlying causes, as Walker describes:
To date, we have discovered numerous triggers that cause sleep difficulties, including psychological, physical, medical, and environmental factors . External factors that cause poor sleep, such as too much bright light at night, the wrong ambient room temperature, caffeine, tobacco, and alcohol consumption can masquerade as insomnia. -Matthew Walker, 243
The Relationship Between Parkinsons Disease And Sleep

Its unclear whether poor sleep causes parkinsonian symptoms to worsen or whether worsening parkinsonian symptoms cause poor sleep. In many cases its likely a case of bidirectionality, with each one exacerbating the other.
Fragmented sleep and sleep deprivation appear to leave the brain more vulnerable to oxidative stress, which has been tied to the development of Parkinsons disease. Parkinsons disease is not usually diagnosed until individuals have developed sufficient motor symptoms, by which time a significant portion of brain cells have already been damaged. If poor sleep quality or having sleep disorders foreshadows the development of parkinsonian symptoms, these could be useful in early diagnosis of the disease.
More research is needed to clarify the multifaceted relationship between Parkinsons disease and sleep. A better understanding of this connection may offer medical experts the unique opportunity to screen at-risk individuals and perhaps delay the onset of the disease.
Recommended Reading: Sam Waterston Parkinson’s
Restless Legs Syndrome And Periodic Limb Movements Of Sleep
Restless legs syndrome usually occurs as one is trying to fall asleep and is characterized by an unpleasant, restless feeling that is only relieved by moving the legs. Periodic limb movements of sleep are rhythmic moving or jerking of the limbs during sleep.
Both RLS and PLMS affect the quality and quantity of sleep. Medications are available that can help these syndromes. Some people also experience relief with an increase in dopaminergic treatment.1
Treatment Of Circadian Abnormalities
Exposure to one hour of bright light once a day during the evening hours for 3 months improved sleep problems assessed by PDSS-2 scores, with restoration of circadian phases based on the assessment of the expression levels of three clock genes in 16 patients with PD . In a randomized trial including 31 treated PD patients with EDS who received 1 hour of bright light therapy or dim-red LT in the morning and in the afternoon for 2 weeks, bright LT improved EDS, sleep quality, and sleep fragmentation and increased daily physical activity in patients with PD .
Read Also: Parkinson’s Hallucinations Commercial
Longitudinal Analyses Of Insomnia Complaints In Pd
A total of 3 longitudinal studies have documented the fluctuating nature of insomnia symptoms in PD. In a population-based study, Tholfsen and colleagues compared insomnia complaints between a newly diagnosed, drug-naïve PD cohort and controls at 3 time points for 5âyears. Insomnia was identified by nocturnal complaints or use of sleeping medications. During the study period, the overall prevalence of insomnia complaints was similar between individuals with PD and controls. Although the prevalence of DMS was equivalent at baseline , follow-up during 5âyears showed an increasing prevalence of DMS for individuals with PD , but not for controls . In another study examining insomnia complaints for 8âyears in moderate PD, Gjerstad and colleagues observed that insomnia was present in 54% to 60% of individuals at each of 3 time points. The prevalence of DIS, DMS, and EMA ranged from 23% to 30%, 23% to 44%, and 19% to 24%, respectively. Of the study participants, 20% developed insomnia. Similarly, in a hospital-based study following individuals with moderate PD for 5âyears, Zhu and colleagues tracked insomnia complaints at annual assessments. Of the study participants, 27% reported insomnia at baseline, and 51% reported insomnia during at least one time point. These data highlight that insomnia rates in PD change over time and require periodic assessments.
Falling Asleep During The Day
Not getting enough restful sleep at night, some medications, and possibly the disease itself leading to neurodegeneration can lead to daytime sleepiness and even sleep attacks in people with Parkinsons disease.
Excessive daytime sleepiness is one of the most frequent sleep disorder symptoms in Parkinsons disease and can affect a patients quality of life.
Trying to get more restful sleep at night and adjusting medications can help with excessive daytime sleepiness.
A new therapy from Theranexus is also currently being investigated in a Phase 2 clinical trial to help with excessive daytime sleepiness.
Parkinsons News Today is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or another qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Recommended Reading: Similar To Parkinsons
Parasomnias In Parkinsons Disease
In PD, parasomnias are quite common, and REM parasomnias are more common than those in NREM . As REM parasomnia in PD, RBD can be seen in near two-thirds of patients . In PD, non-NREM parasomnias can include sleepwalking, confusional arousals, and sleep terrors. However, NREM parasomnias are not a frequent cause of sleep disorders in PD .
Natural Course Of And Risk Factors For Eds In Pd
In a multicenter study, EDS was found in 165 of 436 PD patients, and logistic regression analysis revealed that male sex, Movement Disorder Society -sponsored revision of the Unified Parkinsons Disease Rating Scale III scores , hallucinations, and MDS-UPDRS II scores were associated with EDS . In the analysis by clinical subtype, ESS scores were significantly higher in the patients with the postural instability and gait disturbance type than in those with the tremor-dominant type. The prevalence of EDS increases after the onset of PD motor symptoms. In an 8-year follow-up study of 232 PD patients, the proportion of patients with EDS increased from 5.6%at the beginning of the study to 22.5%at 4 years and 40.8%at 8 years . Logistic regression analysis showed that factors contributing to EDS were older age, male sex, and dopamine agonist use, but in a subanalysis of the patients who were never treated with dopamine agonists, the predictor of EDS was Hoehn-Yahr stage alone. This result indicates that EDS is related to disease severity, independent of the effects of dopamine agonists.
Also Check: Prayers For Parkinson’s Disease
Mechanism Of Arousal In Parkinson’s Disease And Dementia With Lewy Bodies
Lewy body disease affects the brainstem and hypothalamic sleep-wake centers, and the pathology affects multiple neurotransmitter systems . Saper et al. have provided data and a theoretical framework for a neuroanatomic flip-flop switch that regulates the transition from sleep to wakefulness. It includes mutually inhibitory elements responsible for sleep initiation, and brainstem nuclei that promote arousal. One hypothesis for the daytime somnolence in PD and DLB may be associated with the disruption of the wakefulness centers, but perhaps also to damage to the mechanism that switches and maintains wakefulness, presumed to reside in the hypothalamic hypocretin neurons. Involvement of the latter may lead to difficulty keeping the arousal switch in place, which may result in trouble maintaining wakefulness and/or frequent brief transitions of sleep into wakefulness, or microsleeps.
Why Do Parkinsons Patients Sleep So Much
Parkinson’s patients experience difficulties with their sleep due to the disease itself and the medications that treat it. This can lead to increased sleepiness during the day.
Parkinsons disease can cause problems with sleep, and the medications used to treat it can cause even more. Difficulties sleeping during the night can cause daytime sleepiness, and the medications can also cause drowsiness. This disruption to the circadian rhythms can lead to more frequent, lower quality sleep.
Read Also: Diseases Similar To Parkinsons