How Is Parkinsons Disease Diagnosed
A person doesnt need to have all the signs and symptoms of Parkinsons disease to be diagnosed with it.
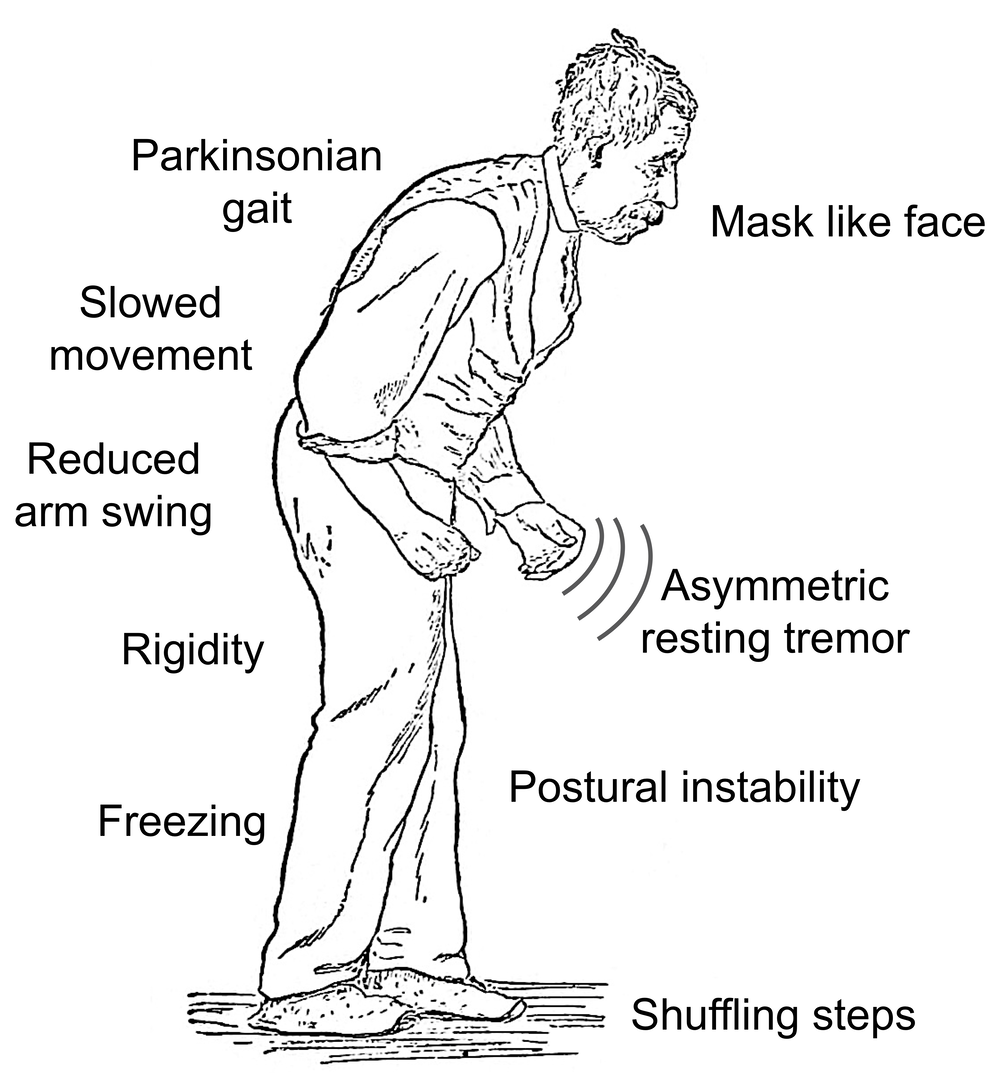
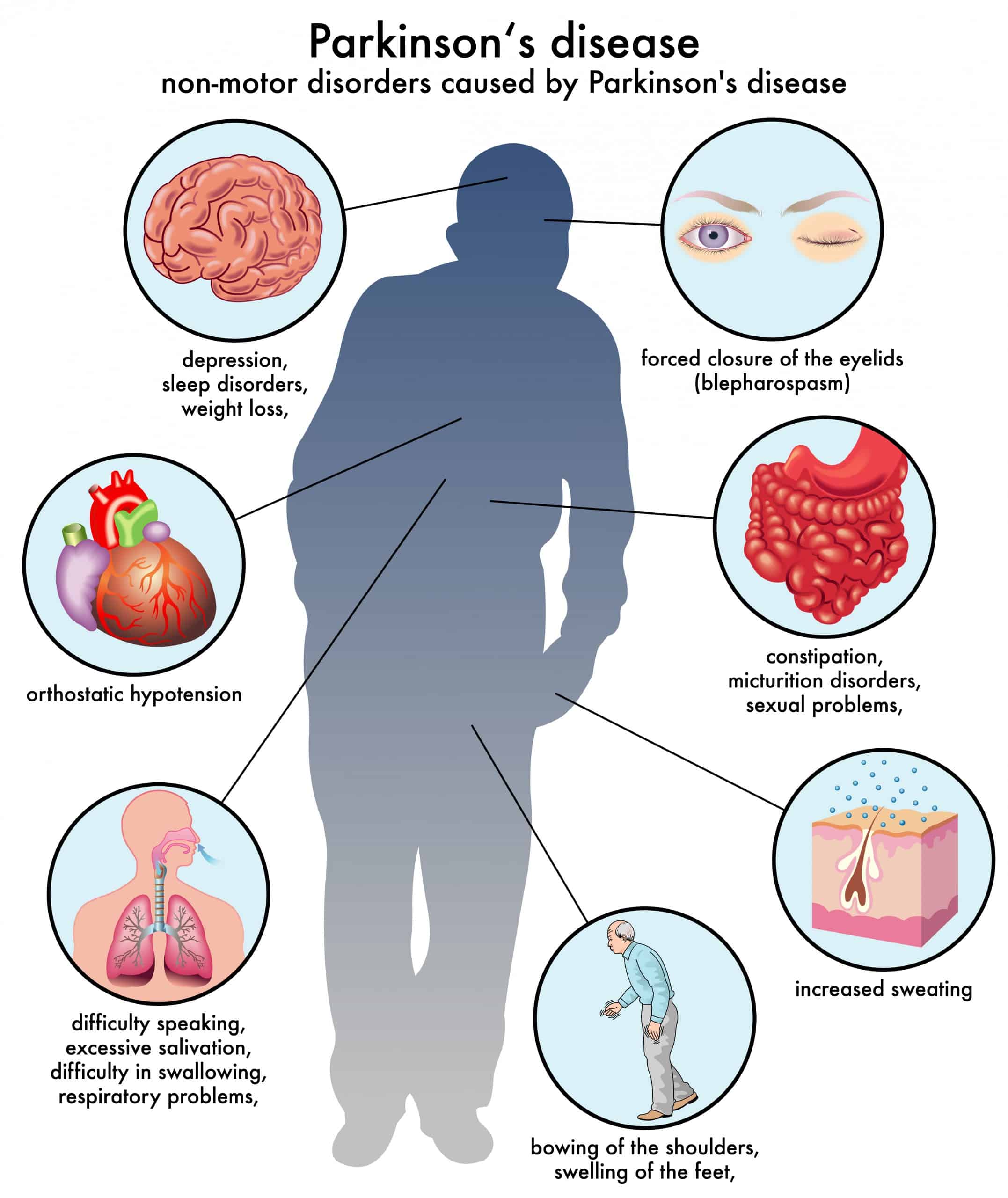
In general, people have a combination of the motor symptoms and the non-motor symptoms, says Dr. Nwabuobi. Some people have more non-motor symptoms than motor and vice versa, but in order to have a diagnosis of Parkinsons, you definitely need the motor symptoms. Were looking for specific things , including a rest tremor, bradykinesia, rigidity, and poor balance.
According to the Parkinsons Foundation, a person needs to have two of the four main motor symptoms of Parkinsons over a period of time to be diagnosed with the disease.
Further Testing In Parkinsons
In other situations, where perhaps the diagnosis is not as clear, younger individuals are affected, or there are atypical symptoms such as tremor affecting both hands or perhaps no tremor at all, further testing may help. For example, imaging can play a role in differentiating between essential tremor and Parkinsons. It can also be important to confirm what is initially a clinical diagnosis of Parkinsons prior to an invasive treatment procedure such as surgical DBS
Walking Freezing And Falling
The dopamine in your brain is heavily involved in controlling the movement of your body. In Parkinsons, there are reduced levels of dopamine. For this reason the most obvious changes related to Parkinsons are normally those that affect your movement, including walking, falling, and freezing.
In particular, slowed movement, stiff muscles and changes to posture affect all people living with Parkinsons. These issues and others can lead to challenges with walking, freezing and falling.
Recommended Reading: Latest Research On Parkinson Disease
Critical Appraisal Of Primary Studies
As presented in Additional file , a variety of different critical appraisal instruments were used to assess the methodological quality of included primary studies. The methodological quality of primary studies was varied and was noted as a limitation in the majority of included systematic reviews. A detailed summary of the critical appraisal of the primary studies is outlined in Additional file .
Support For People Living With Parkinsons Disease
While the progression of Parkinsons is usually slow, eventually a persons daily routines may be affected. Activities such as working, taking care of a home, and participating in social activities with friends may become challenging. Experiencing these changes can be difficult, but support groups can help people cope. These groups can provide information, advice, and connections to resources for those living with Parkinsons disease, their families, and caregivers. The organizations listed below can help people find local support groups and other resources in their communities.
Also Check: Toxic Causes Of Parkinson Disease
Parkinsons Disease And Sleep
Parkinsons disease is a progressive neurodegenerative disorder characterized by the loss of dopamine-producing nerve cells in the brain. Dopamine is a cell-signaling molecule that relays information between nerve cells and between the brain and the muscles. The loss of dopamine leads to symptoms of the motor system such as tremor, bradykinesia , impaired balance, and rigidity. It can also cause non-motor symptoms, including speech, cognitive, mood, and sleep problems.
Most sleep problems in Parkinsons patients can be broken down into one of three categories: trouble falling asleep, trouble staying asleep or getting restful sleep, or falling asleep at the wrong times.
What Are Some Strategies To Prevent Falls In Pd Patients
In this 4-minute video Dr. Bastiaan Bloem recommends preventing falls in those with Parkinsons disease with a multi-disciplinary approach. He outlines specific tasks for a neurologist, physical therapist, occupational therapist and rehabilitation specialist. When prevention of falls is not possible protective measures should be installed around the home, learn to use a walking aid properly or even wear a helmet.
You May Like: Parkinson’s And Alcohol Use
Older Adult Fall Prevention
This short webpage shares facts about falls, why falls are serious and costly, what can happen after a fall, what conditions make it more likely you will fall, and what you can do to prevent falls. The bottom of the page has additional resources and related pages about fall prevention for families and professionals.
Recurrent Falls In Parkinsons Disease: A Systematic Review
Natalie E. Allen
1Clinical and Rehabilitation Sciences Research Group, Faculty of Health Sciences, The University of Sydney, P.O. Box 170, Lidcombe, NSW 1825, Australia
Abstract
Most people with Parkinsons disease fall and many experience recurrent falls. The aim of this review was to examine the scope of recurrent falls and to identify factors associated with recurrent fallers. A database search for journal articles which reported prospectively collected information concerning recurrent falls in people with PD identified 22 studies. In these studies, 60.5% of participants reported at least one fall, with 39% reporting recurrent falls. Recurrent fallers reported an average of 4.7 to 67.6 falls per person per year . Factors associated with recurrent falls include: a positive fall history, increased disease severity and duration, increased motor impairment, treatment with dopamine agonists, increased levodopa dosage, cognitive impairment, fear of falling, freezing of gait, impaired mobility and reduced physical activity. The wide range in the frequency of recurrent falls experienced by people with PD suggests that it would be beneficial to classify recurrent fallers into sub-groups based on fall frequency. Given that there are several factors particularly associated with recurrent falls, fall management and prevention strategies specifically targeting recurrent fallers require urgent evaluation in order to inform clinical practice.
1. Introduction
3. Results
You May Like: What Does Parkinson’s Disease Mean
A Search For Sharpness
But it is the angles and sharpness of brain waves that could hold the key to detecting Parkinsons, according to the new studys findings, which appear in the journal eNeuro.
While working on his doctorate at the University of California, San Diego, fellow study author Scott Cole, Ph.D., realized a potential link between the disease and sharp brain waves.
Using EEG readings taken from 15 Parkinsons patients and 16 healthy individuals, the team honed in on the unfiltered waves.
The raw signals go up and down like sine waves but with more asymmetry, explains Swann, adding, The steepness the slant turns out to be important in Parkinsons patients.
Indeed, the team noticed that Parkinsons patients who were not taking medication had a sharper peak at the top of their brain wave, compared with the bottom.
Finding that a noninvasive method such as an EEG could be a promising diagnostic tool may have important consequences for the future of the disease. The team is hoping that doctors and researchers can use the test to track changes related to Parkinsons in the brain over the years.
We dont know yet whether this approach will be better, but it could provide easily obtained brain measurements that would be helpful and possibly used in tandem with clinical observations and other EEG measurements, notes Swann.
Read Also: Parkinsons Loss Of Taste
Problems With Blood Pressure
Problems with blood pressure can affect people generally as they get older, but some Parkinsons medication can cause side effects, including problems with blood pressure. This can lead to dizziness and falls. If youve felt dizzy, or fallen because of dizziness, ask your GP or practice nurse to check your blood pressure both when youre sitting and standing, to see if its too low.
Drugs used to treat other medical conditions, such as high blood pressure, can potentially make dizziness worse, especially if you are losing weight or not eating and drinking as well as you used to.
Postural hypotension is a sudden drop in blood pressure when changing position, for example getting up out of a chair. It can make you feel very light-headed, which will affect your balance. You may experience postural hypotension as a symptom of Parkinsons. But it can also be caused by the drugs used to treat Parkinsons.
You can avoid some dizzy spells by taking your time. For example, before you get out of bed, sit with your feet touching the floor for a few minutes to get your blood flowing. Then stand up slowly, but try not to walk away immediately stand for a while until you feel steady.
Also Check: Alan Alda Parkinson’s Diagnosis
Dealing With Overlap Of Primary Studies
Overlap of primary studies within included systematic reviews is a challenge exclusive to umbrella reviews. Currently, there is a lack of guidance on how best to manage this occurrence . To maximise comprehensiveness of this umbrella review, we employed a full inclusion scenario where all Cochrane reviews and non-Cochrane reviews were included . A list of the primary studies included in each systematic review was assembled and a matrix of evidence table was created to determine the amount of overlap between systematic reviews. To avoid double-counting outcome data the following were decided:
-
Any systematic review that contained a relevant primary study that was not in any other systematic review was included so that data were not lost.
-
Any systematic review that did not contain any unique primary study was excluded to minimise duplication of data.
-
In the presence of complete overlap between reviews, the highest quality review, as determined by the A MeaSurement Tool to Assess Systematic Reviews 2 was included in data synthesis and analysis.
-
In cases where there was a complete overlap between reviews and they received the same AMSTAR 2 rating, then the most recently published review was included.
-
In the presence of partial overlap, all reviews were included but the degree of overlap was noted and its implications on the findings of this umbrella review were discussed.
Factors Associated With Falling In Pd
Unsurprisingly a history of prior falls was associated with a higher risk of future falls. These results are similar to those found by Bloem et al and are mirrored in a study looking at falls in the general population. Patients with PD who describe prior falls should be thought of as being at risk of future falls.
The association between duration and severity of disease and falling is also important. In this study the risk of falling increased with greater disease severity, but it is important to note that only one subject was in stage IV and none were in stage V. It has been postulated that at more advanced stages the risk of falling may decrease owing to limitations on mobility. Dyskinesia, bradykinesia, and wearing off phenomena may be particularly important for falls risk.
Cognitive impairment was an independent predictor of falling. This is very important because dementia is a common problem in PD and has been minimally studied. Falls prevention in patients with dementia is difficult but recent work suggests that tailored interventions are of benefit in dementia sufferers and this may be extrapolated to dementia in PD. Further studies should address this area.
The association between falls and depression and quality of life is an important finding but many potential confounding variables may affect the scales used. Common sense would dictate that falls are going to impinge upon both mood and quality of life.
Also Check: How To Prevent Parkinson’s Disease
Thanks For Signing Up
We are proud to have you as a part of our community. To ensure you receive the latest Parkinsons news, research updates and more, please check your email for a message from us. If you do not see our email, it may be in your spam folder. Just mark as not spam and you should receive our emails as expected.
You May Like: Best Supplements For Parkinsons
Changes In Cognition And Parkinsons Disease
Some people with Parkinsons may experience changes in their cognitive function, including problems with memory, attention, and the ability to plan and accomplish tasks. Stress, depression, and some medications may also contribute to these changes in cognition.
Over time, as the disease progresses, some people may develop dementia and be diagnosed with Parkinsons dementia, a type of Lewy body dementia. People with Parkinsons dementia may have severe memory and thinking problems that affect daily living.
Talk with your doctor if you or a loved one is diagnosed with Parkinsons disease and is experiencing problems with thinking or memory.
Recommended Reading: Ketogenic Diet And Parkinson’s
Get Daily Living Aids That Can Help You Stay Independent And Safe
Among the tools that an occupational therapist might recommend are railings around your toilet and bathtub, a seat to use in the tub or shower, a pump soap dispenser instead of bar soap, an electric toothbrush and razor, a cordless phone that you can carry around with you, nonskid socks and Velcro-closure shoes, and an appropriate cane, walker, rollator or wheelchair to help you move around effectively.
Recommended Reading: Sam Waterston Tremor
Inclusion And Exclusion Criteria
Quantitative systematic reviews , mixed-methods systematic reviews , or pooled analyses and research syntheses investigating the effectiveness of non-pharmacological falls prevention interventions for people with MS, PD and stroke were considered for inclusion in this umbrella review. Reviews published in the English language were included and authors of potentially relevant reviews published in a different language were contacted to ascertain if a copy of the review was available in English. No restriction was placed on year of publication of the review. In instances where a systematic review was an update of a previous review, the most recent version was included and the older version excluded. For the purposes of this umbrella review, a review was classified as an update of a previous version if there were changes pertaining to new data, new methods, or new analyses, but the research question, objectives and inclusion criteria remained similar . In the case of new authors or a different research team updating an existing review, they had to clearly state that their review was an update and acknowledge the work of the authors on the previous edition .
The eligibility criteria based on population, intervention, comparator, outcome and study design are outlined below.
Population
Intervention
Comparator
Outcomes
Study design
Systematic reviews of all study designs investigating falls prevention interventions were considered for inclusion.
Don’t Miss: Who Has Parkinson’s Disease
What Are The Causes And Symptoms Of Parkinsons Disease
As a neurodegenerative disorder, Parkinsons Disease leads to the progressive deterioration of motor function due to loss of dopamine-producing brain cells. While the cause of Parkinsons Disease is unknown, researchers speculate that both genetic and environmental factors are involved. Studies also show that men are 50% more likely to develop the disorder than women.
Primary symptoms of Parkinsons Disease:
Dont Miss: Prayers For Parkinsons Disease
Stages And Symptoms Of Parkinsons Disease
Parkinsons disease progresses over time and affects individuals at differing rates. The earliest Parkinsons symptoms are often subtle and sporadic. Every now and then, a person may notice a tremor, slight staggering gait, or have trouble getting up from a chair and pass it off as a symptom of aging. Other Parkinsons symptoms like occasional depression, insomnia, constipation, and loss of smell may be so amorphous and general that they are brushed off as a temporary nuisance.
In many cases, it takes a family member or friend pointing out that the individual is speaking softer than usual or moving their arms in a stiff manner to make the patient aware of changes that are taking place in their body. At this early stage, a patient might want to consult their physician and start treatment before the disease progresses to its later stages with more crippling symptoms.
Also Check: Robert Wood Johnson Parkinson’s Disease Center
Drugs And Medication Used To Treat Parkinsons Disease
A number of different drugs can be used to treat Parkinsons.
Levodopa
Levodopa is the most common treatment for Parkinsons. It helps to replenish dopamine.
About 75 percent of cases respond to levodopa, but not all symptoms are improved. Levodopa is generally given with carbidopa.
Carbidopa delays the breakdown of levodopa which in turn increases the availability of levodopa at the blood-brain barrier.
Dopamine agonists
Dopamine agonists can imitate the action of dopamine in the brain. Theyre less effective than levodopa, but they can be useful as bridge medications when levodopa is less effective.
Drugs in this class include bromocriptine, pramipexole, and ropinirole.
Anticholinergics
Anticholinergics are used to block the parasympathetic nervous system. They can help with rigidity.
Benztropine and trihexyphenidyl are anticholinergics used to treat Parkinsons.
Amantadine
Amantadine can be used along with carbidopa-levodopa. Its a glutamate-blocking drug . It offers short-term relief for the involuntary movements that can be a side effect of levodopa.
COMT inhibitors
Catechol O-methyltransferase inhibitors prolong the effect of levodopa. Entacapone and tolcapone are examples of COMT inhibitors.
Tolcapone can cause liver damage. Its usually saved for people who do not respond to other therapies.
Ectacapone does not cause liver damage.
Stalevo is a drug that combines ectacapone and carbidopa-levodopa in one pill.
MAO-B inhibitors
Ways To Reduce The Risk Of Falling
There are several steps people living with PD can take to reduce their risk of falling, including:
- Talk to your doctor about your risks. Your doctor can assess your personal risk and can help you manage your medications and any side effects. Medications may need to be adjusted or switched up.
- Exercising regularly helps maintain strength, improve stamina, improve balance, and reduce the risk of falls. Exercises that challenge your balance are especially beneficial, and research has shown that exercise that requires your attention, concentration and focus on activity and movement may also be neuroprotective protecting the nerve cells from damage and possibly slowing the progression of PD.
- Make modifications to your home. There are several adaptations that can be made in your home to make falls less likely, such as removing throw rugs, ensuring wide pathways through furniture, and adding non-skid mats and grab bars to showers and bathtubs.
- Use a walking aid.Canes or four-wheeled walkers offer stability for people with PD.
- Learn ways to overcome freezing episodes, such as walking in beat to music or a metronome. Some people also find it helpful to move from side to side before stepping forward.
- Work with a physical therapist or occupational therapist.Physical and occupational therapists can provide exercises to help keep you mobile. Occupational therapists also can suggest adaptations and modifications to the persons environment.1,3-5
Don’t Miss: Parkinson’s Phase 3 Trials