Determination Of Neurogenic Orthostatic Hypotension Status
Presence of neurogenic vs. non-neurogenic orthostatic hypotension was determined from a metric validated in similar population of PD patients, and using corroborating physiologic measures,,. Neurogenic orthostatic hypotension was determined from the ratio of heart rate change to systolic blood pressure change from supine-to-standing transition / = HR/SBP, with HR/SBP=< 0.5 most consistently corresponding to neurogenic forms of OH within the physiogically validated cohort. The ratio was calculated only for subjects with orthostatic hypotension, as defined by SBP20 or DBP10 mmHg.
Symptoms And Diagnostic Considerations
Rapid Eye Movement Sleep Behavior Disorder is a non-familial sleep disorder, characterized by the loss of the inherent muscle atonia observed during normal REM sleep. This phenomenon is often referred to as REM Sleep without Atonia . Whilst isolated RSWA is frequently an incidental finding in sleep studies, it forms the substrate of the dream enactment behavior which defines RBD. Here, individuals experience vivid dreams which they act out during sleep.
It is important to remember that dream enactment and limb movements during sleep can occur in the healthy population, often in the context of heightened emotional states . The same symptoms may also be experienced during withdrawal from sedatives or alcohol. In non-pathological dream enactment, individuals typically respond to dream content during the transition from REM sleep to the awake state and while maintaining REM atonia during much of the REM period. In contrast, RBD individuals will maintain REM sleep during and immediately after most of their dream enactments. As acute dream enactment is generally self-limiting, the chronicity of symptoms is a key distinguishing factor, and forms part of the diagnostic criteria for RBD .
A Cheaper Quicker Form Of Assessment
Unlike the usual method of assessing the risk of Parkinsons disease, which is called dopamine transporter imaging, the current assessment is inexpensive and easy to apply.
Dopamine transporter imaging, explain Dr. Postuma and colleagues, assesses the integrity of the dopaminergic system, which typically becomes compromised in parkinsonism and Parkinsons disease. However, this test is complex and costly. In contrast, assessing for the risk factors that the current study considers is both quick and cost efficient.
We confirmed a very high risk of in people with REM sleep disorder and found several strong predictors of this progression, notes Dr. Postuma.
As new disease-modifying treatments are being developed for and related diseases, these patients are ideal candidates for neuroprotective trials.
Dr. Ron Postuma
Don’t Miss: Does Parkinson’s Cause Sleepiness
Rapid Eye Movement Sleep Behavior Disorder In Parkinsons Disease
Table 2Table 3
Based on the PD model proposed by Braak et al.4141. Braak H, Del Tredici K, Rüb U, de Vos RA, Jansen Steur EN, Braak E. Staging of brain pathology related to sporadic Parkinson’s disease. Neurobiol Aging. Mar-Apr 2003 24:197-211. https://doi.org/10.1016/s0197-458000065-9, pre-symptomatic PD stages are characterized by the deposition of Lewy bodies in the dorsal pons, bulb, and olfactory nucleus. This explains why RBD precedes PD motor symptoms in some cases nevertheless, it does not explain why many PD patients do not present RBD. Histopathological changes have been reported in patients with iRBD who did not clinically present neurological disorders. These changes included the presence of Lewy bodies in the brainstem in one patient and decreased monoaminergic neurons in the locus coeruleus and substantia nigra in another2020. Schenck CH, Boeve BF, Mahowald MW. Delayed emergence of a parkinsonian disorder or dementia in 81% of older men initially diagnosed with idiopathic rapid eye movement sleep behavior disorder: a 16-year update on a previously reported series. Sleep Med. 2013 Aug 14:744-8. https://doi.org/10.1016/j.sleep.2012.10.009.
What Are The Risk Factors For Rem Sleep Behavior Disorder
REM sleep behavior disorder primarily affects men over 60 years of age, with about 80% of cases being diagnosed with Parkinsons disease however, the following factors may also increase the risk of developing the disorder.
- Gender: Males are more likely to develop RBD than females at a risk ratio of 9 to 1.
- Age: REM Sleep Behavior Disorder is most often diagnosed after the age of 50.
- Family History: Having a family history of narcolepsy, Parkinsons disease or other neurological disorders may indicate an increased risk for RBD.
Recommended Reading: How Many People In Us Have Parkinsons
Diagnosis And Treatment Of Parkinsons Sleep Problems
Parkinsons disease is chronic and progressive, meaning it tends to get worse over time. However, there are treatment options that can help manage symptoms and allow patients to get more restful sleep.
The simplest way to start sleeping better with Parkinsons disease is by adopting healthy sleep habits. Sleep hygiene tips for Parkinsons disease sufferers include:
- Sticking to regular bedtimes
- Following a consistent bedtime routine with soothing activities such as listening to music or reading a calming book
- Getting regular exercise, preferably early in the day
- Getting adequate exposure to light, whether outdoors or through light therapy
- Avoiding long naps and naps late in the day
- Creating a cool, dark, and comfortable sleeping environment
- Restricting bedtime activities to sex and sleep only
- Turning off screens an hour before bedtime
- Reducing liquid intake before bedtime
- Avoiding caffeine, alcohol, and tobacco
- Eating a healthy diet and avoiding large meals at night
Light therapy, exercise, and deep brain stimulation have been successfully used to improve overall sleep quality and to treat specific conditions, such as REM sleep behavior disorder, in patients with Parkinsons disease. Cognitive behavioral therapy for insomnia has proven effective at reducing insomnia in healthy adults, although further research is needed on the effects of CBT in patients with Parkinsons disease.
- Was this article helpful?
Somnolence And Excessive Daytime Sleepiness
Somnolence and EDS occur commonly in PD. Etiologies of somnolence in PD include reversal of the sleepwake cycle, the disease process itself, disrupted sleep due to a variety of motor and nonmotor causes, and the use of dopamine agonists and other antiparkinsonian medications. Several studies have found that dopamine agonists are more likely to cause somnolence than levodopa. The soporific effects of the commonly used dopamine agonists appear to be similar as assessed by Epworth Sleepiness Scale scores.36
EDS occurs in PD patients, and is usually associated with dopamine agonist use. EDS may occur with use of other PD medications, including levodopa/carbidopa. However, EDS as measured by the ESS does not always correspond to shortened sleep latency as quantified by the Multiple Sleep Latency Test .10 In addition, nocturnal sleep disturbance as measured by polysomnogram may not account for the severity of daytime sleepiness in PD patients with EDS.10
Recommended Reading: How Does Parkinsons Disease Develop
Recommended Reading: Reishi Mushroom Parkinson’s Disease
How To Take Action And Improve Your Sleep
Limit Lights In Your Room
Minimize your exposure to artificial lights when preparing for bed. Sleep in a cool, dark place. Avoid bright lights when sleeping. You could keep dim night lights if sleeping in complete darkness is uncomfortable.
Avoid watching television and using mobile devices before bed or lying in bed. These devices emit blue lights that could affect your sleeping habits.
Don’t Miss: Social Security Disability Parkinson’s
How Are Sleep Problems Diagnosed In People With Parkinsons Disease
If youre having problems sleeping, sit down with your healthcare provider to discuss the issue in detail. Your provider will ask you questions to better understand your symptoms.
Be prepared to explain when sleep disruptions happen and how they affect your life. Keeping a sleep journal for a few weeks can help you remember the details.
If your provider suspects you may have a sleep disorder, they may recommend you have a sleep study. This overnight test uses electrodes attached to your skin to track how your body functions when youre sleeping.
How Is Daytime Sleepiness Treated
Consider making certain lifestyle modifications, such as:
- Establish good sleep hygiene, including a set bedtime and wake-up time.
- Get exposure to adequate light during the day and darkness at night.
- Remember indoor lighting may not be sufficient to promote a normal circadian rhythm.
- Avoid sedentary activities during the day.
- Participate in activities outside the home. They may help provide stimulation to prevent daytime dozing.
- Get physical exercise appropriate to your level of functioning, which may also promote daytime wakefulness. Strenuous exercise, however, should be avoided six hours before sleep.
- Do NOT drive while sleepy if you experience excessive daytime sleepiness. Motor vehicle accidents increase during periods of drowsiness and may be associated with sudden onset of sleep .
- Talk to your doctor about possibly decreasing the dosage of dopamine agonists if you experience daytime sleepiness or sleep attacks.
- Talk to your doctor about decreasing stimulants like caffeine, modafinil and methylphenidate .
You May Like: Voice Amplifiers For Parkinson’s Patients
Idiopathic Rapid Eye Movement Sleep Behavior Disorder
iRBD, which occurs without neurodegenerative disease, was first described in 1986, with similar phenomenological reports being presented in the 1970s. It is characterized by central nervous system dysfunction during sleep and wakefulness with cortical activity impairment, neuropsychological changes, and autonomic dysfunction1313. Fantini ML, Ferini-Strambi L, Montplaisir J. Idiopathic REM sleep behavior disorder: Toward a better nosologic definition. Neurology. 2005 Mar 64:780-6. https://doi.org/10.1212/01.WNL.0000152878.79429.00.
How Does Parkinsons Disease Cause Sleep Problems
Researchers have yet to uncover every nuance of the Parkinsons and sleep connection. So far, medical experts believe several causes may contribute:
- Chemical changes in the brain: Ongoing research shows that Parkinsons disease may disrupt sleep-wake cycles. Changes to certain brain chemicals may cause people with Parkinsons to get less sleep.
- Medication: Some drugs that treat Parkinsons disease may make it harder to fall or stay asleep. A medication may also disrupt your sleep patterns by making you drowsy during the day .
- Mental health challenges: People with Parkinsons commonly deal with mood disorders, such as anxiety or depression. Any mood disorder may keep you up at night or make you sleep less soundly.
- Parkinsons symptoms: Pain, waking up at night to pee or other Parkinsons symptoms can make restful sleep harder to come by. Sleep apnea can also disrupt sleep.
Don’t Miss: Clinical Manifestations Of Parkinson’s Disease
What Are The Complications Of Rem Sleep Behavior Disorder
Complications of RBD include accidental injury to oneself or their sleeping partner, later development of a neurological disorder such as Parkinsons disease or Dementia with Lewy Bodies, and Excessive Daytime Sleepiness .
- Accidental Injury Accidental injury to self or bed partner occurs because the sleeper is acting out their dreams and cannot distinguish between reality and dream. Someone sleepwalking will be somewhat limited in their ability to act out physically however, this may not be the case with someone experiencing REM Sleep Behavior Disorder. The lack of muscle inhibition allows the sleeper to hit as hard as they may while awake or jump just as far as they might normally.
- Development of Neurological Disorder Because RBD is associated with the development of other neurological disorders such as Parkinsons disease or Dementia with Lewy Bodies, many people experience some form of memory loss while awake. They may find themselves more confused, tired, or otherwise more forgetful than they would like to admit. However, this progression is more likely to occur in later stages of co-morbid diseases such as Parkinsons disease.
- Excessive Daytime Sleepiness Excessive Daytime Sleepiness is one of the top complaints among people with RBD. This is because of the lack of quality sleep experienced while dreaming during REM sleep and common co-morbid sleep conditions like narcolepsy.
Getting Your Best Sleep With Parkinsons
This 1-hour webinar includes an interview of a person with Parkinsons disease, a movement disorders specialist, and a sleep sciences specialist. They discuss sleep disorders associated with Parkinsons disease, the difference between those that are a symptom the disease or a side-effect of medication, and how to treat them and live your best life with a sleep disorder.
Read Also: Parkinsonism Is Characterized By The Loss Of
Preclinical Biomarkers Of Parkinsons Disease In Patients With Rem Sleep Behaviour Disorder
Rapid eye movement sleep behaviour disorder is a condition in which patients thrash about while acting out dreams. Within the first 10 years of being diagnosed with the disorder, people are at high risk of developing Parkinsons disease.
At Western University, neuroscience graduate student Erind Alushaj is using Magnetic Resonance Imaging to scan the brains of people with the sleep disorder, known as RBD. Hes comparing scans of patients with RBD to scans of people with Parkinsons disease.
The MRI scans will focus on changes to iron levels and structural connections in the areas of the brain, such as the substantia nigra, that Parkinsons disease most affects.
Researchers believe higher-than-normal levels of iron and damage to the structural connections in the substantia nigra are both connected to Parkinsons disease.
If the changes Alushaj finds are similar in the brains of both people with RBD and Parkinsons, his work will solidify the link between the two diseases.
At around the 10-year-mark of their diagnosis, the majority of REM sleep behaviour disorder patients will have converted, or gotten, Parkinsons disease.
The research findings may help with earlier diagnosis of people at risk of Parkinsons.
Another way this research could help is by ensuring individuals who are at high risk of developing Parkinsons are included in clinical trials developing neuro-protective or preventative treatment, says Alushaj.
What To Do If Rbd Is Suspected
While REM sleep behavior disorder may occur in conjunction with, or as a predecessor to, certain neurological disorders such as Parkinsons disease, it can also result from medication usage.
If you or a loved one is concerned about RBD, contact a movement disorder neurologist or sleep disorders specialist, such as the experts available at Michigan Medicine, for an evaluation.
Don’t Miss: Celebrities With Parkinson’s Disease
Stratifying Risk For Clinical Trials
We then tested potential selection strategies to increase likelihood of conversion to clinical neurodegenerative disease . Using single markers, stratification could increase likelihood of conversion to disease, sometimes with only minimal loss in screening. Simple measures such as removing possible antidepressant-caused RBD or patients younger than 55 years increased conversion rates modestly. Other clinical signs were more powerful stratifiers, albeit with more recruitment cost. Selecting patients with olfactory loss would allow 52% cohort eligibility and increased 3-year conversion from 30% to 40% and 5-year conversion from 47% to 63%. Selecting those with motor impairment increased conversion more dramatically, to 56% at 3 years and 74% at 5 years .
We then explored whether combining markers could further stratify disease risk . We found numerous potential strategies for increasing conversion rates. For example, removing age younger than 55 years and possible antidepressant-caused RBD, combined with any one of abnormal olfaction, color vision, or motor impairment, increased disease risk to 44% at 3 years and 61% at 5 years, while retaining 66% eligibility. Stricter eligibility requirements could dramatically increase conversion motor impairment and age/antidepressant exclusion obtained a 65% 3-year rate . Requiring 2/3 abnormalities increased 3-year conversion to 60% and 5-year conversion to 80% , and 3/3 abnormalities identified near-certain conversion .
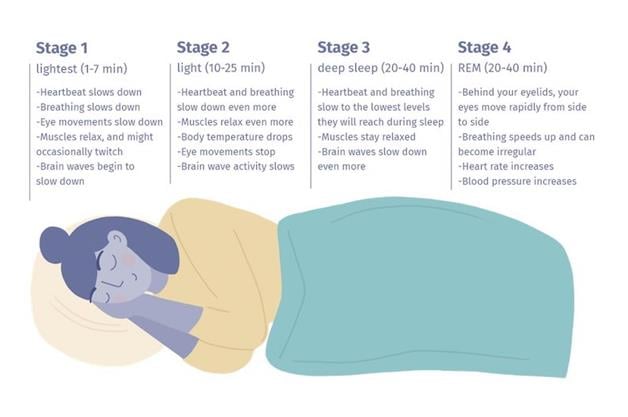
Sleep Architecture In Healthy Adults
Sleep is divided into non-rapid eye movement sleep , and rapid eye movement sleep which alternate intermittently throughout the night . NREMS is further divided into 4 stages , where stages 3 and 4 are collectively known as Slow Wave Sleep .
A healthy adult falls asleep within 10 min and undergo a cyclic sequence of the five sleep stages, beginning with NREMS stage 1 advancing onto stage 2, followed by SWS and finally REMS. The individual then resumes back to NREMS , and the cycle recommences.
REMS and NREMS substitute throughout the night in an ultradian pattern every 85â100 min consisting of 3â5 cycles each night , where NREMS dictates the first half of the night mostly with SWS, whereas REMS and stage 2 NREMS abound in the latter half of the night .
Also Check: Signs Of Early Onset Parkinsons
Also Check: Naturopathic Medicine For Parkinson’s Disease
Sleep Disorders In Parkinsons Disease
In this 17-minute lecture Dr Gary Leo discuses sleep challenges caused by the neurochemical changes, medications and mood disturbances of Parkinsons disease, and normal changes of aging. He discusses possible causes and treatment options of sleep maintenance insomnia, REM Sleep Behavior Disorder, daytime sleepiness, sleep apnea, and restless leg syndrome, ending with some tips for good sleep.
Sleep Matters: A Review Of Sleep Issues In Parkinson’s
Sleep disorders are present in 66-99% of people with Parkinson’s disease . In this 1-hour webinar Okeanis Vaou, MD, describes common sleep disorders in PD and how to treat them. Disorders described include REM sleep behavior disorder, daytime sleepiness, insomnia, nocturnal motor fluctuations, and restless leg syndrome. Dr. Vaou ends the webinar with tips on how to maintain good sleep hygiene.
You May Like: Power For Parkinson’s Exercise Videos