Us Food And Drug Administrationapproved Agents For Pdp: Pimavanserin
Pimavanserin is a 5-HT2A inverse agonist indicated for the treatment of hallucinations and delusions associated with PDP.25 Pimavanserin binds preferentially to the 5-HT2A receptor and, to a lesser extent, to the 5-HT2C receptors, and has low binding affinity to alpha, dopamine D2, histamine, muscarinic, and other serotonin receptors.26 The pharmacologic rationale for the efficacy of pimavanserin in PDP is based on investigations demonstrating that overstimulation of postsynaptic 5-HT neurons contributes to psychotic symptoms in PD. Serotonin 5-HT2A receptors exhibit baseline activity.27,28 In other words, 5-HT2A receptors spontaneously signal to produce and regulate cellular postsynaptic activity. Pimavanserin binds to 5-HT2A receptors and blocks the receptor and reduces the spontaneous baseline activity.28 This property of binding to the receptor and reducing spontaneous baseline activity is referred to as inverse agonism.
The US Food and Drug Administrationapproved labels for pimavanserin and all antipsychotics contain a boxed warning stating elderly patients with dementia-related psychosis treated with antipsychotic drugs are at an increased risk of death.31 However, it is important to note that if the psychotic symptoms are related to the underlying PD, pimavanserin can be used in patients with concurrent dementia.
How Common Is Parkinson’s Disease Psychosis
Between 20-40% of people with Parkinsons report the experience of hallucinations or delusions. When followed as the disease progresses over the years, this number increases. The increase does not mean that the hallucinations are persistent across the majority of patients. However, it is important to note that these statistics sometimes include delirium, in which the symptoms are temporary due to medication that needs to be adjusted or infection that needs to be treated, and isolated minor symptoms or minor hallucinations, including illusions, where instead of seeing things that are not there , people misinterpret things that are really there. These are the most common types of psychosis in people with PD, with different studies placing the occurrence between 25-70% of people with Parkinsons. Typically, if the person with PD only has these minor hallucinations, their doctor will not prescribe an antipsychotic medication, though more significant psychosis that requires medication may develop over time. In one study, 10% of those with minor hallucinations had their symptoms resolved within a few years, while 52% saw their symptoms remain the same and 38% saw their psychosis symptoms get worse.
We recommend that people with Parkinsons not use a single percentage to represent the prevalence of hallucinations and PDP. Parkinsons is a complex disease and as it progresses the percentages and risk of symptoms will change.
Features Of Parkinson’s Disease Psychosis
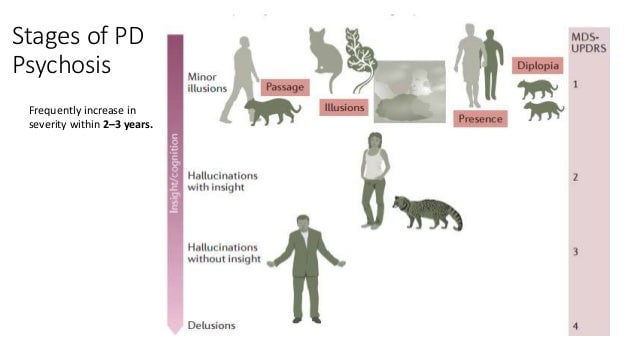
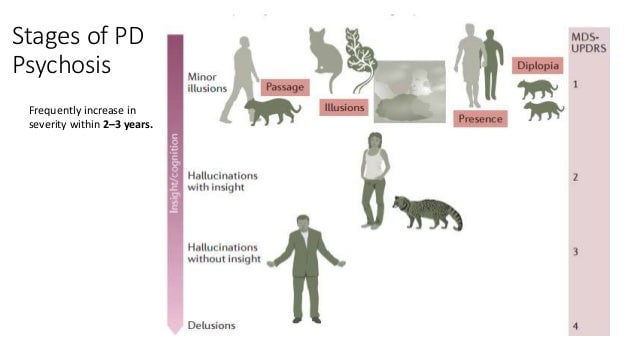
PDP typically arises later in the course of the disease, approximately 10 years after initial diagnosis of PD. Symptoms typically arise in the context of retained insight and clear sensorium . Over time, symptoms such as visual hallucinations or delusions tend to recur and progress and insight is lost. Prominent hallucinations early in the course of the disease may suggest Lewy body dementia, Alzheimer’s disease, or a preexisting psychiatric disorder .
Don’t Miss: Reciprocal Exercises For Parkinson’s
Treatment Options For Pd Psychosis
Treating psychosis is truly a challenge. Unfortunately, only 10 to 20 percent of people with PD psychosis actually inform their doctor of their symptoms. Dr. Dewey speculates that stigma and fear of embarrassment prevent many patients from seeking help.
When new symptoms of any kind arise, it is crucial to make a doctors appointment to discuss the issue. A physician will first try to determine whether there is an underlying illness that could be causing psychotic behaviors. Treating the underlying cause is one of the simplest ways of minimizing these episodes.
When there is no other identifiable source, doctors often turn their attention to the medications that the patient is taking. Gradually decreasing the dosage of dopamine-enhancing medication may reduce psychotic symptoms, but the obvious trade-off is that the persons motor function is likely to deteriorate more rapidly. Balancing risks and benefits is a delicate and complicated process that often involves a three-step approach, including assessment and planning, adjusting or reducing any medications, and initiating antipsychotic therapy.
Medical research produces discoveries continually, so keeping an ongoing dialogue open with your loved ones doctor should be a priority. Finding the best balance of treatment is crucial for optimum care and quality of life.
Families Often See The Signs First
Often, loved ones or close family members may notice the signs of psychosis in Parkinsons disease first. Diagnosis is based on history, often with patients families reporting that symptoms are occurring, says Dr. Hui. To confirm the diagnosis, your doctor will consider a variety of diagnostic criteria, such as which specific symptoms are present and when they began, as well as ruling out other potential causes, according to a study in Parkinsons Disease.
Don’t Miss: Can A Blood Test Detect Parkinson’s
Risk Factors For Psychosis
Not everyone with Parkinsons will develop hallucinations or delusions, but there are several things can increase your risk:
- Dementia or impaired memory
- Depression: Individuals suffering from depression and PD are at a greater risk. In addition, severe depression alone can cause psychosis.
- Sleep disorders, such as vivid dreaming. Individuals commonly report vivid dreaming prior to the onset of psychosis. Other associated sleep disturbances include REM sleep disorder and general insomnia.
- Impaired vision
- Use of PD medications
Hallucinations And Delusions In Pd
Hallucinations and delusions are collectively referred to as psychosis.
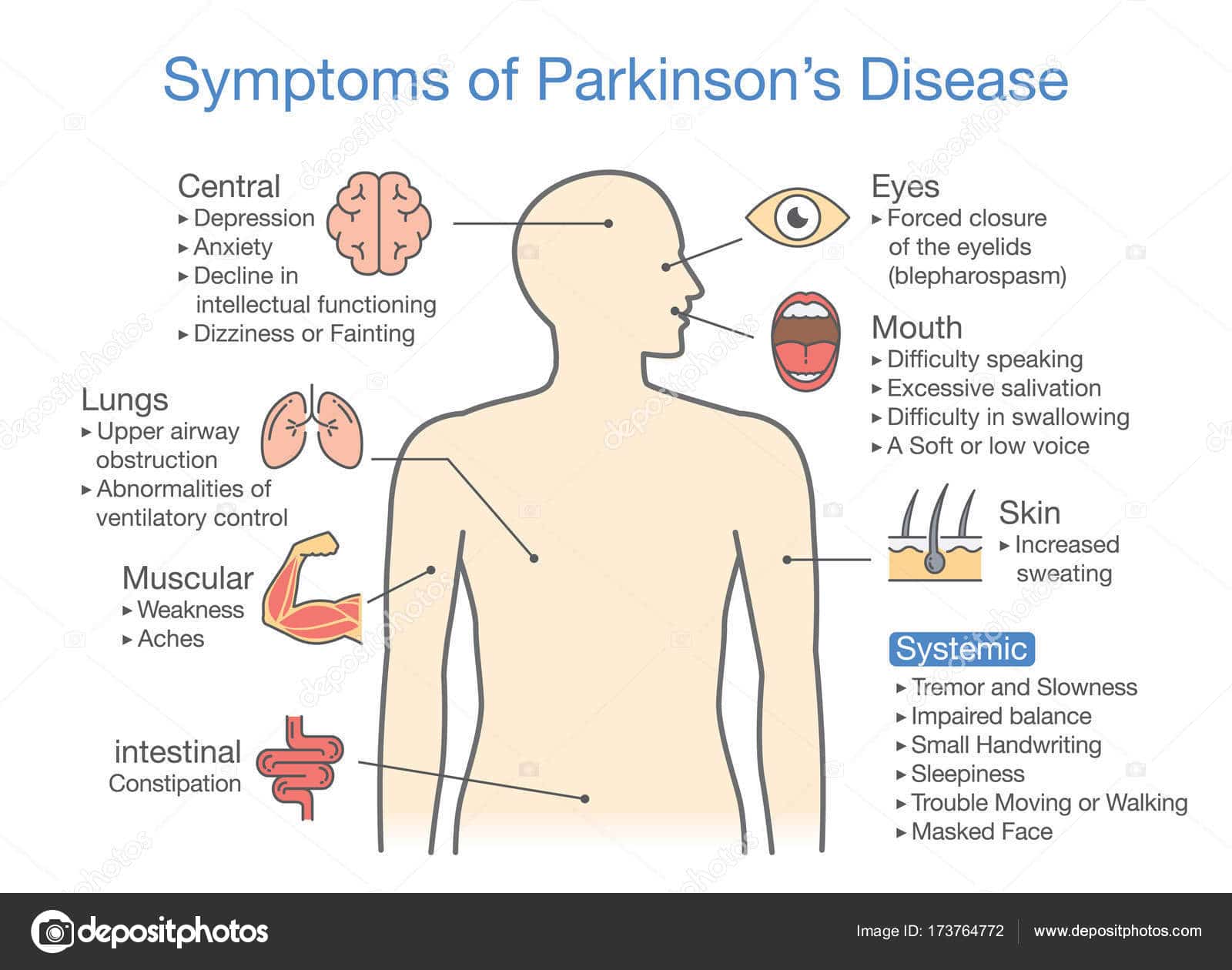
Visual hallucinations are the most common type of hallucination. In a visual hallucination, someone sees things that are not actually there. There can also be auditory and olfactory hallucinations. Often hallucinations are not alarming to the person experiencing them.
Delusions are when there is an alternative view of reality: an entire irrational story is created. Paranoia is a common type of delusion. Capgras delusions are a specific type of delusion where the person believes that a spouse, adult child, or other family member has been replaced by an imposter.
Don’t Miss: Is Parkinsonism The Same As Parkinson’s Disease
Psychosis And Dopamine Agonists
The majority of PDP symptoms are felt to be secondary to treatment with dopamine agonists, as the prevalence of psychotic symptoms dramatically rises with the addition of dopamine agonists. This is parsimonious and consistent with the general idea that psychosis is a consequence of increased dopaminergic transmission in the mesolimbic dopaminergic pathway. In a cross-sectional retrospective study of PD patients with psychosis vs. age-matched controls without psychosis, there was a positive correlation found between psychosis and dementia, number of medications, and pergolide intake . In terms of medications, the adjusted odds ratio was calculated to be the highest with pergolide and the lowest with levodopa . This lack of association with levodopa is further supported by data showing that the relationship of PDP symptoms with mean levodopa and levodopa-equivalent may not be always established .
Another study using the administrative health care databases of Ontario, Canada, examined 10,347 individuals 66 years of age or older following recent initiation with dopaminergic therapy. The estimate for the cumulative probability of requiring an antipsychotic at 7 years was 35% 499 individuals were prescribed an antipsychotic within 1 year of starting dopaminergic therapy. This also suggests a role for dopaminergic treatment in the development of psychosis .
Keep Your Home Well Lit
A dark environment may be associated with increased hallucinations, says Dr. Barrett. For some people, increased lighting may help, he says. However, this could also have a negative effect on sleep, so it should be approached with that in mind. After all, adequate sleep can help you feel better, he says. Talk with your doctor about adjustments that might work for you.
Also Check: American Parkinson Disease Association Northwest Chapter
Parkinsons Disease: Symptoms Of Psychosis
Common symptoms of psychosis in Parkinsons disease include:
- Visual hallucinations: Seeing things or people that aren’t there
- Auditory hallucinations: Hearing voices and other noises that no one else can hear. Parkinsons disease and auditory hallucinations are more common in people over the age of 65
- Tactile hallucinations: Touching or feeling something that isnt really there
- Olfactory hallucinations: Imagining strong smells
- Confusion: Not being sure whats real and what isnt. In Parkinsons disease, hallucinations and confusion can occur as a result of certain PD drugs, so your doctor may wish to change your medication if you report these symptoms
- Paranoia: Believing that people aren’t who they say they are, or that your loved ones or doctors are trying to hurt you. You may also feel an intense suspicion of abandonment or extreme jealousy of others who are well
- Delusions: Irrational or illogical beliefs not based in reality
- Agitation: A state of high anxiety or extreme restlessness
- Argumentative and aggressive behavior: Lashing out at others or refusing help
Confusion and delusional thinking are common in PD psychosis, so you may not be able to identify psychotic symptoms in yourself. Usually, Parkinson’s disease psychosis is noticed by loved ones or care staff. However, if you think you’re displaying some of the signs, report them to your doctor immediately. Psychotic episodes can be incredibly frightening and upsetting, but there’s no need to suffer in silence.
What Are The Considerations For Pain Management In The Last Days Of Life In Pd
It is important to consider that pain can be a risk factor for, and associated with, many other symptoms which might be the presenting features in a patient with complex or advanced PD. These include a new or worsened confusion, hallucinations, agitation and symptoms of depression or apathy.
As well as being an underlying cause of another symptom, pain can also be the symptom of other features of PD, such as rigidity, dyskinesia, but also non-motor features, for example, depression and fatigue.
Identifying whether pain is at the root of the presenting complaint and what might be causing the pain is therefore the most important part of the initial history from the patient and the carer. Then using the clinical examination to confirm findings from the history and identify any features not already elicited such as abnormal posturing, or dystonia.
A recent review into the pathophysiology and treatment of pain in PD suggests simple analgesia with paracetamol and non-steroidal anti-inflammatory drugs but advises caution with opiate analgesia as constipation is a recognised problem in PD patients.25 The review mentions, however, the lack of evidence for many widely used analgesics specifically in PD.26
Dont Miss: Nocturnal Leg Cramps Parkinsons
Also Check: Power For Parkinson’s Exercise Videos
Stage Five Of Parkinsons Disease
Stage five is the most advanced and is characterized by an inability to rise from a chair or get out of bed without help, they may have a tendency to fall when standing or turning, and they may freeze or stumble when walking.
Around-the-clock assistance is required at this stage to reduce the risk of falling and help the patient with all daily activities. At stage five, the patient may also experience hallucinations or delusions.
While the symptoms worsen over time, it is worth noting that some patients with PD never reach stage five. Also, the length of time to progress through the different stages varies from individual to individual. Not all the symptoms may occur in one individual either. For example, one person may have a tremor but balance remains intact. In addition, there are treatments available that can help at every stage of the disease. However, the earlier the diagnosis, and the earlier the stage at which the disease is diagnosed, the more effective the treatment is at alleviating symptoms.
Also Check: Parkinsons And Similar Diseases
Understanding Parkinsons Care In The Later Stages: Part 3 Of 3
Parkinsons care moves to a whole new level as the disease progresses.
A Parkinsons disease diagnosis has an effect on family members along with the person experiencing this illness. Understanding what to expect as the disease progresses is paramount to being prepared for the changes to come and also to making life the best it can be each day.
Over the last couple of months, we have published blog posts about what to expect in the early and middle stages of Parkinsons disease. Information has included what family caregivers can do to best assist a family member with Parkinsons and how Anthem Home Care, a leader in professional home care in Taft, TX and surrounding areas, can help. In this closing segment in the series, we offer advice about Parkinsons care for someone in the late stages of this illness.
Don’t Miss: Do Tremors Come And Go With Parkinson’s
What Causes Psychotic Symptoms
Psychotic symptoms in people with PD are usually caused as a side effect of medications used to treat PD.
All of the current PD medications can potentially cause psychotic symptoms. Hallucinations and delusions may also be caused by the chemical and physical changes that occur in the brain as a result of PD. 3
My Parkinsons Story: Advanced Parkinsons
This 10-minute video alternates between an interview with a man and his wife and his palliative care team, including a doctor, nurse, clerg and social worker. The man and his wife shares his experience with late stage Parkinsons. The palliative care team explains that their job is to support the best physical, emotional and spiritual wellbeing of the immediate family as well as help the family make end of life decisions.
Recommended Reading: Parkinson’s Vaccine Shows Positive Results
Theory Of Pd Progression: Braaks Hypothesis
The current theory is that the earliest signs of Parkinsons are found in the enteric nervous system, the medulla and the olfactory bulb, which controls sense of smell. Under this theory, Parkinsons only progresses to the substantia nigra and cortex over time.
This theory is increasingly borne out by evidence that non-motor symptoms, such as a loss of sense of smell , sleep disorders and constipation may precede the motor features of the disease by several years. For this reason, researchers are increasingly focused on these non-motor symptoms to detect PD as early as possible and to look for ways to stop its progression.
Page reviewed by Dr. Ryan Barmore, Movement Disorders Fellow at the University of Florida, a Parkinsons Foundation Center of Excellence.
Hallucinations And Rem Sleep Disorders In Parkinson’s Disease
At timestamp 1:58 in this recording of Thrive: HAPS 2020 Caregiver Conference, you will find a one hour talk by neurologist Joohi Jimenez-Shahed, MD. In it she delves into what REM sleep behavior disorder is and is not, and the distinctions between hallucinations, delusions, and delirium. Managment options for RBD and hallucinations are included.
Recommended Reading: What Are The Signs Of Parkinson’s Disease
What To Expect In The Late Stages
The late stages of PD are medically classified as stage four and stage five by the Hoehn and Yahr scale:
- Stage Four of Parkinsons Disease In stage four, PD has progressed to a severely disabling disease. Patients with stage four PD may be able to walk and stand unassisted, but they are noticeably incapacitated. Many use a walker to help them. At this stage, the patient is unable to live an independent life and needs assistance with some activities of daily living. The necessity for help with daily living defines this stage. If the patient is still able to live alone, it is still defined as Stage Three.
- Stage Five of Parkinsons Disease Stage five is the most advanced and is characterized by an inability to arise from a chair or get out of bed without help. They may have a tendency to fall when standing or turning, and they may freeze or stumble when walking. Around-the-clock assistance is required at this stage to reduce the risk of falling and help the patient with all daily activities. At stage five, the patient may also experience hallucinations or delusions.1,2
Also Check: Is Cbd Good For Parkinsons
Diagnosis Of Dip And The Role Of Dat Imaging
The clinical diagnostic criteria for DIP are defined as 1) the presence of parkinsonism, 2) no history of parkinsonism before the use of the offending drug, and 3) onset of parkinsonian symptoms during use of the offending drug. Since asymmetrical rest tremors are common in many DIP patients and symptoms persist or progress after cessation of the offending drug, patients clinically diagnosed with DIP may include individuals in the preclinical stage of PD whose symptoms were unmasked by the drug.,,,
DATs are presynaptic proteins in the membrane on terminals of dopaminergic neurons. They take up dopamine from the synaptic cleft projections that extend from the substantia nigra to the striatum. These transporters control dopaminergic transmission by spatial and temporal buffering, rendering the molecule an imaging target in diseases affecting the dopaminergic nigrostriatal pathway. Single-photon-emission computed tomography and positron-emission tomography scans are available using several DAT ligands., SPECT radioligands include 123I-N-3-fluoropropyl-2-carbomethoxy-3-nortropane , 123I-ioflupane, DaTSCAN, and 123I-2-carbomethoxy-3-tropane . PET scans may be superior to SPECT for imaging DATs, in that the lower energy of positrons provides higher resolution, resulting in better image quality with widespread clinical applications. However, most DAT imaging studies, including those in patients with DIP, have utilized SPECT.,-
Also Check: On Off Phenomenon
Don’t Miss: Parkinson’s Spoon And Fork
How Is Parkinsons Disease Diagnosed
Diagnosing Parkinsons disease is sometimes difficult, since early symptoms can mimic other disorders and there are no specific blood or other laboratory tests to diagnose the disease. Imaging tests, such as CT or MRI scans, may be used to rule out other disorders that cause similar symptoms.
To diagnose Parkinsons disease, you will be asked about your medical history and family history of neurologic disorders as well as your current symptoms, medications and possible exposure to toxins. Your doctor will look for signs of tremor and muscle rigidity, watch you walk, check your posture and coordination and look for slowness of movement.
If you think you may have Parkinsons disease, you should probably see a neurologist, preferably a movement disorders-trained neurologist. The treatment decisions made early in the illness can affect the long-term success of the treatment.
Are There Alternative Therapies For Essential Tremor
Currently, there is no evidence that alternative treatments are beneficial in treating Essential Tremor. Patients who have tremors that worsen with emotional stress may find relaxation therapies helpful at temporarily easing symptoms.
Some herbal supplements may make tremor worse. Always consult your doctor before trying any alternative therapy.
Show Sources
Don’t Miss: First Signs Of Parkinson’s Disease Uk