Increased Risk Of Overactive Bladder In Patients With Idiopathic Parkinsons Disease: Insight From A Nationwide Population
-
Roles Conceptualization, Investigation, Methodology, Writing original draft
Affiliation Department of Neurology, China Medical University Hospital, China Medical University School of Medicine, Taichung, Taiwan
-
Affiliation Department of Neurology, China Medical University Hospital, China Medical University School of Medicine, Taichung, Taiwan
You May Like: Pfnca Wellness Programs
Urinary Tract Infection In Parkinsons Disease
Article type: Review Article
Authors: Hogg, Elliota | Frank, Samuela | Oft, Jillianb | Benway, Brianc | Rashid, Mohammad Haruna | Lahiri, Shourid*
Affiliations: Department of Neurology, Cedars-Sinai Medical Center, Los Angeles, CA, USA | Department of Infectious Diseases, Cedars-Sinai Medical Center, Los Angeles, CA, USA | Department of Urology, Cedars-Sinai Medical Center, Los Angeles, CA, USA | Departments of Neurology, Neurosurgery, and Biomedical Sciences, Cedars-Sinai Medical Center, Los Angeles, CA, USA
Correspondence: Correspondence to: Shouri Lahiri, MD, Departments of Neurology, Neurosurgery, and Biomedical Sciences, Cedars-Sinai Medical Center, 8700 Beverly Blvd., Los Angeles, CA 90048, USA. E-mail: .
Keywords: Parkinsons disease, urinary tract infection, delirium, falls, exacerbation
DOI: 10.3233/JPD-213103
Journal: Journal of Parkinsons Disease, vol. Pre-press, no. Pre-press, pp. 1-15, 2022
Abstract
Recommended Reading: Azithromycin Urinary Tract Infection Dose
What’s Next For Those Suffering From Urinary Incontinence
I decided I did not want to add another medication to the medicine bag. I was trying to see if there was something I could do besides resigning myself to wearing pads or some other incontinence protection all the time. At 53 years old, I wanted to see if there was a way I could help myself.
Part 2 of this article will address my experiences. I plan to discuss what I lovingly refer to as “PEE PEE PT” – physical therapy to help treat urinary incontinence.
Recommended Reading: On And Off Phenomenon
Urinary And Fecal Incontinence
I just wanted to say, as a care provider, that this topic should be more discussed as an issue with PD. We have two neurologists, one who is really renowned as a PD specialist in the area, but discuss this topic with them and they get kind of quiet and say thats not really their domain. But when you read articles like this one: bladderandbowel.org/associa it clearly indicates that it IS a part of PD. Why dont more people talk about this or am I just not looking in the right places. The coordination of messaging between the brain and muscles is the thing, right? So both the urinary and bowel systems have muscles and sphincter muscles that need messaging from the brain, hence PD problem. If anyone has any tips with how to help my loved one in this area, Id greatly appreciate it. Its demoralizing and wish I could just fix it.
According to a Michael J. Fox podcast several years ago urinary problems effect 43% of people with Stage 1 Parkinsons. 90% of those at stage 4 and 5. So you are on track with your suggestion that these subjects should be talked about more here.
There was an report on a study published last February that might be of interest as it points to a solution. Title was:
Clinical study of the effects of deep brain stimulation on urinary dysfunctions in patients with Parkinsons disease. Briefly . . .
SKCW:
Let me know directly by messaging me.
Sharon
What Is Parkinsons Disease
Parkinsons disease is a progressive neurological disorder that affects how your muscles move. In the beginning stages, it can be easy to miss the early signs and symptoms of Parkinsons disease. The most common ones include:
- Tremors, usually starting with the fingers or hand
- A noticeable change in handwriting
- Walking is slower, movement is stiffer
- Stiff, rigid muscles
Also Check: What Causes Urinary Urgency And Frequency
You May Like: Yopd Life Expectancy
Overactive Bladder Is The Major Symptom In Pd
LUTS are divided majorly into two: storage symptoms and voiding symptoms. Storage symptoms are the most common of the LUTS symptom types in PD. Storage symptoms include nocturia , which is the most prevalent symptom reported by patients with PD ., Patients also complain of urinary urgency and daytime frequency . Urinary incontinence was present in 26% of male and 28% of female patients with PD.
Read Also: Yopd Life Expectancy
Diagnosing A Urinary Tract Infection In Older Adults
Vague, uncommon symptoms such as confusion make UTIs challenging to diagnose in many older adults. Once your doctor suspects a UTI, its easily confirmed with a simple urinalysis.
Your doctor may perform a urine culture to determine the type of bacteria causing the infection and the best antibiotic to treat it.
There are home UTI tests that check urine for nitrates and leukocytes. Both are often present in UTIs. Because bacteria are often in the urine of older adults to some degree, these tests arent always accurate. Call your doctor if you take a home test and get a positive result.
Antibiotics are the treatment of choice for UTIs in older adults and younger people. Your doctor may prescribe amoxicillin and nitrofurantoin .
More severe infections may require a broad-spectrum antibiotic such as ciprofloxacin and levofloxacin .
You should start antibiotics as soon as possible and take them for the entire duration of treatment as prescribed by your doctor. Stopping treatment early, even if symptoms resolve, increases the risks of recurrence and antibiotic resistance.
Antibiotic overuse also increases your risk for antibiotic resistance. For this reason, your doctor will likely prescribe the shortest treatment course possible. Treatment typically lasts no more than 7 days, and your infection should clear up in a few days.
Its important to drink plenty of water during treatment to help flush out the remaining bacteria.
Also Check: How Does Someone Get A Urinary Tract Infection
You May Like: Zhichan Capsule
Papers Of Particular Interest Published Recently Have Been Highlighted As: Of Importance Of Major Importance
Whats Next For Those Suffering From Urinary Incontinence
I decided I did not want to add another medication to the medicine bag. I was trying to see if there was something I could do besides resigning myself to wearing pads or some other incontinence protection all the time. At 53 years old, I wanted to see if there was a way I could help myself.
Part 2 of this article will address my experiences. I plan to discuss what I lovingly refer to as PEE PEE PT physical therapy to help treat urinary incontinence.
You May Like: Voice Amplifiers For Parkinsons
Read Also: Similar To Parkinsons
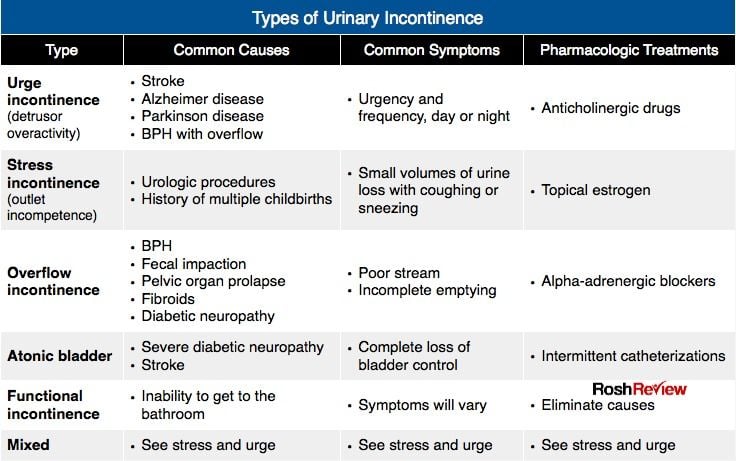
What Medications Help To Treat Urinary Incontinence
So back to the TV ads for urinary incontinence that have us adding MORE medication to our already full medication bag here are many medications that can help this problem. Medications include:
- Oxybutynin
- Mirabegron
- Phenoperidine fumarate
Do we really want to add that medication to the already growing list to our medications? The answer is YES!
Problems Caused By Limited Mobility
Some people with Parkinsons might soil their underwear. This is because mobility problems can make it difficult to wipe after using the toilet. If this is the case, it might help to use wet wipes, a bidet, or an adapted bottom wiper. An occupational therapist or the Disabled Living Foundation can offer further advice.
Bowel problems are common. But you should tell your GP if there are any changes in your bowel habits, particularly if you see blood in your stool. Some problems are difficult to avoid, but there are things you can do to make them less likely to happen.
Read Also: Parkinson Bicycle Cleveland Clinic
Treatment For Genitourinary Dysfunctions
Unlike the motor symptoms of PD, genitourinary dysfunctions do not respond to levodopa therapy, and other treatments must be used. There are several medications that can help manage urinary difficulties, including Detrol® , Ditropan® , Enablex® , and Vesicare® . These medications work to block or reduce overactivity in the bladder. Treatments for sexual dysfunction include counseling or talk therapy, treating erectile dysfunction with Viagra® or Cialis® , and the use of lubricants in women.1,3-5
Compliance With Ethical Standards
Amit Batla and Natalie Tayim each declare no potential conflicts of interest.
Mahreen Pakzad has been a speaker for Astellas.
Jalesh N. Panicker has received royalties from Cambridge University Press, has been involved in trials supported by FirstKind Ltd, Allergan and Ipsen and has received speaker honoraria from Wellspect, Astellas and Allergan.
You May Like: Prayers For Parkinson’s Disease
Ui And Adverse Health Outcomes
The mean follow-up of time of the participants was nearly 8 years . We employed a Cox proportional hazards model adjusted for age, sex, and education to examine the association of baseline UI with incident parkinsonism. Baseline UI was associated with incident parkinsonism . Since we treated UI as a numerical scale, inspection of the hazard ratio suggests that an individual with severe incontinence , had about a 30% increased risk of developing parkinsonism as compared to an individual without incontinence.
Since the pathologic basis for parkinsonism in older adults with and without a clinical diagnosis of PD may vary , we repeated this analysis excluding 65 cases with a clinical diagnosis of PD. Baseline UI remained associated with incident parkinsonism . In a final model, adding terms for seven chronic health conditions and BMI did not attenuate the association of UI with incident parkinsonism .
In further analyses, we examined whether baseline UI was associated with other adverse health outcomes. Baseline UI was also associated with risk of death and incident ADL and mobility disability, but was not associated with incident MCI or AD dementia . These findings were unchanged when we controlled for seven chronic health conditions and BMI .
The Cross-Sectional and Longitudinal Associations of Baseline Urinary Incontinence and Global Cognition in Community-Dwelling Older Adults*
| Model Terms . |
|---|
Reduced Functional Bladder Capacity At Night
Functional bladder capacity is diminished if the bladder wall compliance is reduced, the detrusor is involuntarily contracting , or if the bladder has incompletely emptied following a void. All three of these are known to occur in PD. Nocturia results whenever the urine volume produced at night exceeds the functional bladder capacity. Urodynamic evidence for detrusor overactivity has been reported in 45% to 93% of PD patients, , and correlates with scores in overactive bladder questionnaires. In urodynamic studies, 81.0% had storage disorder, 54.8% had abnormalities of storage and voiding, whereas 19.0% had only a voiding disorder.,
A likely mechanism for DO in PD is disruption of the dopamine D1-GABAergic direct pathway and its GABAergic collateral to the micturition circuit,, resulting in loss of inhibition of the micturition reflex and OAB. Severity of OAB symptoms has been shown to correlate with impairments observed on urodynamic testing and dopaminergic deficiency observed in dopamine transporter scans.,
You May Like: Pre Parkinsons Disease Symptoms
Don’t Miss: Voice Amplifiers For Parkinson’s
Make Changes To Diet & Lifestyle
- Healthy and balanced diet means a happy bladder and bowels!
- A diet rich in veggies and fruits always helps with clean living.
- I have found that a diet rich in organic foods with less processed foods helps too.
- We get dehydrated easily! Drink fluids! Gatorade and water are great!!
- Alcohol, soda, and caffeine can irritate the bladder, so I try to drink those sparingly.
Urinary Problems In Parkinson’s Disease
Parkinsons disease has many features that have little or nothing to do with movement. Among these non-motor symptoms are problems with the autonomic nervous system the part of the nervous system that controls automatic bodily functions, such as heart rate, blood pressure, sweating, sexual function and both gastrointestinal and urinary function. These symptoms are often among the most serious and complex issues faced by people with PD.
Unlike bowel dysfunction , which often occurs before Parkinsons movement symptoms, urinary dysfunction is not typically a problem until the later stages of the disease.
Recommended Reading: Parkinson’s Double Vision
Why Do Some People With Parkinson’s Disease Experience Urinary Incontinence
Parkinson’s is best known for its effects on balance and movement, but it impacts the autonomic nervous system as well. The autonomic nervous system controls specific bodily functions, like heart rate, blood pressure, libido, and urine production.
Over time, changes to the autonomic nervous system affect your bladder’s ability to store and release urine. That means you might have trouble making it to the bathroom on time or need to urinate more frequently.
Treating And Managing Bladder Problems
It is important to discuss any bladder difficulties, including those listed below, with your doctor, even if this may appear embarrassing. Your doctor will then be able to properly assess and treat any problems, for example:
- inability or difficulty emptying the bladder even when it feels full
- significant, uncontrolled leakage of urine at any time
- unusually frequent urination
- an urgent, immediate need to urinate, or urine leaking if you do not immediately do so
- pain when urinating.
It may be helpful to write notes to discuss with your doctor, for example, the type of difficulties experienced, their frequency, when you first noticed a change, and your normal eating and drinking habits.
Bladder problems can occur for a number of reasons, so the first approach will be to eliminate causes other than Parkinsons, such as urinary infections and prostate problems in men.
Don’t Miss: Weighted Silverware
Sexual Dysfunction In Parkinsons Disease
People with PD may experience sexual dysfunction, including loss of desire, inability to orgasm, erectile dysfunction in men, decreased lubrication in women, or pain with intercourse in women. Some studies have found that sexual dysfunction may occur in 60-80% of men and women with PD. Older patients with PD have more sexual dysfunction than younger patients, although sexual dysfunction is also greater in older adults who do not have PD. In addition to age, conditions such as diabetes, hypertension, and depression can factor into sexual dysfunction.3,4
There are several factors that can lead to sexual dysfunction in people with PD. In addition to the motor symptoms of PD, which may create practical barriers to engaging in sexual activity, non-motor symptoms like depression, anxiety, or sleep disturbances can also impact a persons sex drive. Many people with PD express dissatisfaction with their sexual life.3,5
Some people with PD who are treated with dopamine agonists develop impulse control disorders, like hypersexuality. Hypersexuality can lead to unusual or increased sexual behavior, which may have devastating effects on relationships. Changing medications or reducing the dose of medication can help, and people who experience any side effects such as impulse control disorders should bring it to the attention of their doctor.3
How Is Parkinsons Linked To Incontinence
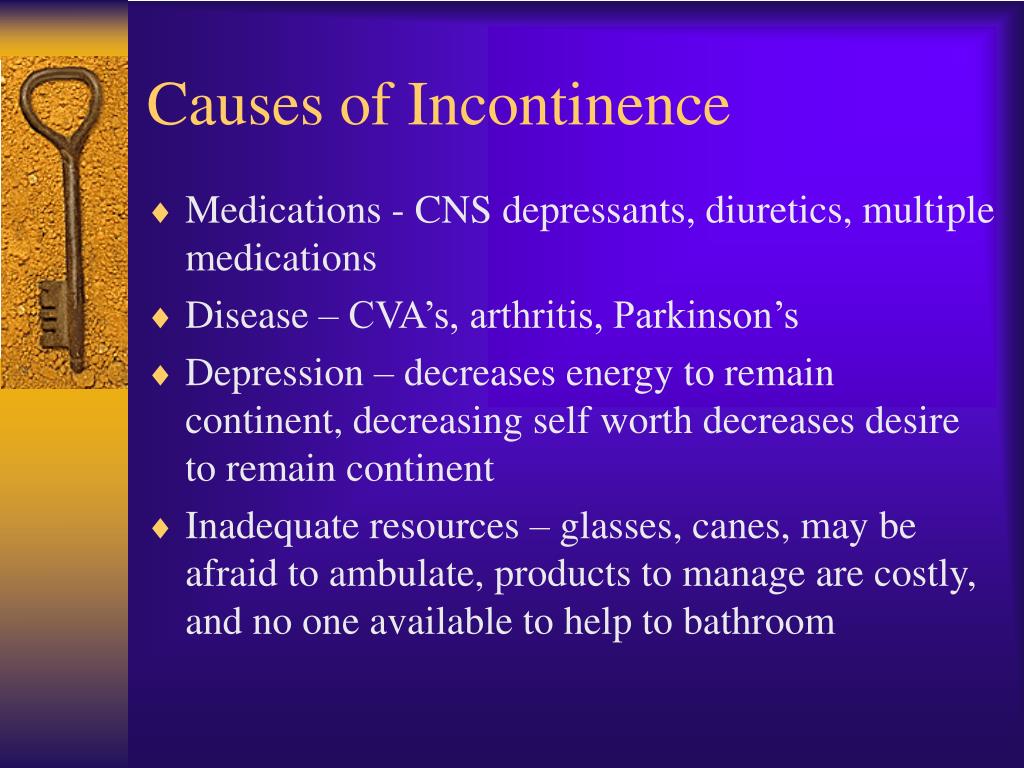
People with Parkinsons disease are more likely to have incontinence because messages going from their brain to their bladder can be interrupted. This is due to Parkinsons being triggered by having fewer nerve cells which contain dopamine this is a chemical messenger which helps you to have coordinated movement.
As a result of this, the bladder will contract when its not even particularly full, meaning that your loved one may not have time to get to the toilet before urine leakage occurs.
The types of urinary incontinence most often experienced by those with Parkinsons will be nocturia and urge incontinence. It is also common for people with Parkinsons to suffer from bowel incontinence.
Don’t Miss: Does Vitamin B12 Help Parkinson’s
Cardiovascular Dysautonomia And Nocturia
An association is known to exist between orthostatic hypotension and nocturia, and nocturnal polyuria. In health, blood pressure is known to decrease at night, and this is often absent in patients with PD reporting autonomic failure. This may be mediated through inappropriate mineralocorticoid receptor activation. Consequent to this, pressure natriuresis occurs, resulting in increased urine output and the patient reports nocturia. OH and supine hypertension frequently coexist in PD, and older age, akinetic-rigid motor subtype, and pre-existing hypertension are independent risk factors for supine hypertension. Improvement of nocturia, however, has not been a consistent finding in studies evaluating treatments for supine hypertension,, , and therefore cardiovascular dysautonomia is likely to be only one of several mechanisms responsible for nocturia in PD.
Evaluating And Treating Urinary Issues In Parkinsons Disease Multiple System Atrophy And The Other Atypical Parkinsonism Disorders
In this hour-long webinar, neuro-urologist Ekene Enemchukwu, MD focuses on urinary incontinence, overactive bladder, urinary retention, and other urinary issues in PD, MSA, and the atypical parkinsonism disorders. Following the presentation, moderator Candy Welch, Brain Support Networks MSA caregiver support group leader, asks Dr. Enemchukwu many questions submitted by webinar participants.
Recommended Reading: Stretching Exercises For Parkinsons Disease
You May Like: What Foods Should Be Avoided When Taking Levodopa
Management Of Incontinence In Patients With Parkinsons Disease
It is estimated that two-thirds of all patients with PD have some degree of bladder problems ranging from complete inability to empty the bladder to the more common problem of urinating too often and to the ability to make it to the bathroom in time . Common dysfunctions are bladder overactivity, causing urinary urgency, frequency, and incontinence . Getting up at night to use the bathroom is the most prevalently reported non-motor symptom with PD, reported by more than 60%. Weak voiding is also a common dysfunction. Patients may feel like they must go frequently, but when they go it may take longer than average to void. Constipation is another common issue that may arise and being constipated can affect medication absorption. Some studies suggest that 80% of people who have Parkinsons Disease report constipation.
Patients with Parkinsons Disease may also have difficulty eliminating urine. This can be caused by a sphincter that wants to close when the bladder is ready to empty or by a bladder muscle that is too weak to expel urine. This is a concern because incomplete bladder emptying can cause accumulation of urine and the growth of bacteria. The latter can result in an infection. The symptoms of difficulty eliminating urine include weak urinary stream, dribbling or leaking, and feeling that the bladder has not completely emptied.
Patient should be educated to alert their health care provider is they have any of the following signs: