Whats The Difference Between Progressive Supranuclear Palsy And Parkinsons
People with PSP generally progress more rapidly than people with Parkinsons. A person with Parkinsons tends to lean forward while a person with PSP tends to lean backward. Tremors are common in people with Parkinsons and rare in people with PSP. Speech and swallowing abnormalities are more severe and show up sooner in those living with PSP.
For more information on progressive supranuclear palsy, read this fact sheet and insights from the CurePSP organization website.
Neuronal And Glial Tau Pathology In Psp
PSP is a degenerative tauopathy characterized by accumulation of filamentous tau inclusions within neurons. Tau is a microtubule associated protein that is biochemically composed of six major isoforms related to alternative mRNA splicing, including three isoforms with four 32-amino acid conserved repeats in the microtubule binding domain and three isoforms with three repeats . In PSP, 4R tau preferentially accumulates, whereas in Alzheimers disease tau inclusions are composed on a nearly equal mixture of 3R and 4R tau. Monoclonal antibodies specific to 3R and 4R tau now permit assessment of the type of tau that accumulates within neuronal lesions with routine immunohistochemistry .
In addition to neurofibrillary tangles , tau pathology of PSP is characterized by inclusions in astrocytes and in oligodendroglia . The latter glial lesions are distinct from the glial cytoplasmic inclusions of MSA and the sparse glial lesions detected in PD, not only based on their immunoreactivity with tau, but also on their morphology. Tau also accumulates in cell processes , referred to as tau-positive threads.
What Causes Huntingtons Disease
Huntingtons disease is caused by a mutation in the HTT gene. The HTT gene is responsible for making the huntingtin protein, which is thought to play an important role in nerve cells of the brain.
In Huntingtons disease, a DNA segment within this gene, called the CAG trinucleotide repeat, is repeated more often than is normal.
Read Also: What Other Diseases Mimic Parkinson’s
Parkinsonism Different Than Parkinsons Disease
Study of Parkinsonism Offers Better Estimate of Its Rate of Occurrence
Journalists interested in receiving a copy of the JAMA article or in interviewing researchers may contact Nick Hanson at .
What Is Huntingtons Disease
Huntington disease usually appears in a persons thirties or forties. Early signs and symptoms can include depression, irritability, poor coordination, small involuntary movements, and trouble learning new information or making decisions. Many people with Huntington disease develop involuntary, repetitive jerking movements known as chorea. As the disease, progresses symptoms become more pronounced. People with this disorder also experience changes in personality and decrease in thinking abilities. Affected individuals usually live about 15 to 20 years after signs and symptoms begin.
There is no care for this disorder, and it is largely determined genetically due to mutations in the HTT gene. The juvenile form of this disorder also exists. Chorea can be controlled with medicines. However, other higher function abnormalities are difficult to control.
Coronal section from an MR brain scan of a patient with HD.
You May Like: Parkinson’s Donations In Memory Of
Whats The Difference Between Vascular Parkinsonism And Parkinsons
As the name implies, vascular parkinsonism is caused by cerebrovascular disease which affects the blood supply to the brain. Vascular parkinsonism is caused by one or more small strokes, while Parkinsons is caused by a gradual loss of nerve cells. One major difference from Parkinsons is that its not progressive, while Parkinsons becomes worse with time. Another difference is that there are no tremors in vascular parkinsonism.
For more information on vascular parkinsonism, read this journal article.
How Many Canadians Live With Parkinsonism And How Many Are Newly Diagnosed Each Year
Based on the latest estimates available , in 20132014, approximately 84,000 Canadians aged 40 years and older were living with diagnosed parkinsonism and 10,000 Canadians were newly diagnosed with this condition . The age-standardized prevalence was 1.5Footnote i times higher among males than among females , and similarly the age-standardized incidence was 1.7Footnote i times higher among males than females . The epidemiological burden of parkinsonism increases with age. In 20132014, when comparing estimates among Canadians aged 85 years and older vs. those aged 40-44 years, the prevalence of the condition was 169Footnote i times higher in the older age group , while the incidence was 48Footnote i times higher in the older age group .
Figure 1: Prevalence of diagnosed parkinsonism, including Parkinsons disease, by sex and age group, Canada, 20132014
| Age group |
|---|
| 44.7 | 55.1 |
Note: The 95% confidence interval shows an estimated range of values which is likely to include the true value 19 times out of 20. Data source: Public Health Agency of Canada, using Canadian Chronic Disease Surveillance System data files contributed by provinces and territories, July 2017.
You May Like: Parkinson’s Disease Treatment Guidelines
Whats The Difference Between Multiple System Atrophy And Parkinsons
Parkinsons and MSA both affect the movement control system and the involuntary autonomic control system and early symptoms can make a differential diagnosis a challenge. MSA, however, tends to progress faster than Parkinsons balance problems and a stooped posture happen earlier and get worse more quickly with MSA and autonomic functions such as blood pressure, heart rate, breathing, sweating, bladder function, and sexual problems are more severe in people with MSA.
For more information on multiple symptom atrophy, read this fact sheet.
Possible Link To Alzheimers
Though Alzheimers, Huntingtons, and Parkinsons are distinctly different diseases, some evidence has emerged that shows a common link between the three.
All three diseases have proteins within the cells that do not assemble properly. Though the molecular and cellular changes that occur in each disease vary greatly, this protein degradation has been shown to precede early clinical signs in each disease. This is promising news, as more studies are being done to determine whether this can either predict or prevent these neurodegenerative diseases.
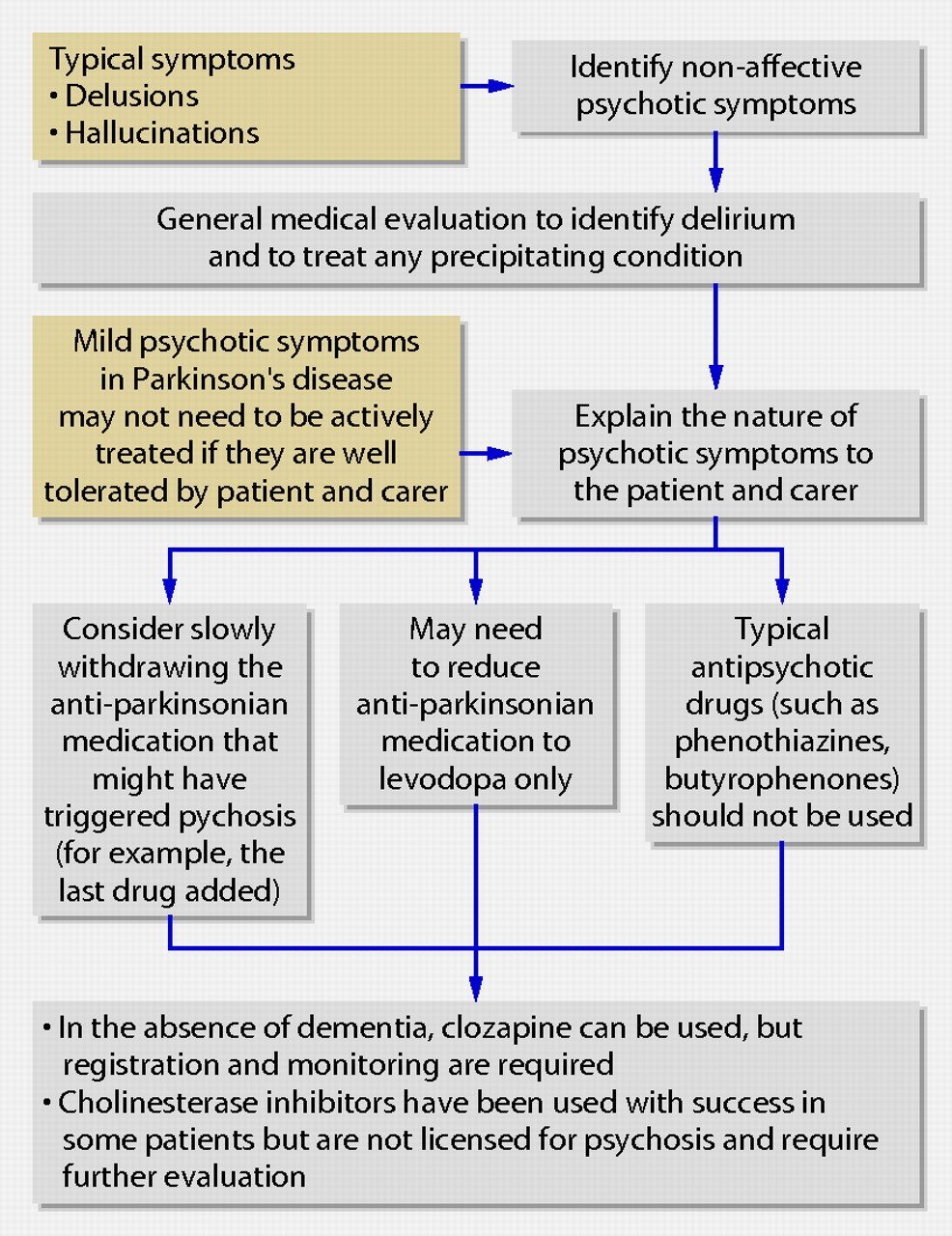
Don’t Miss: Can Parkinson’s Psychosis Be Reversed
Longitudinal Alterations Of Mirnas That Regulate Autophagy
Key autophagy genes ATG12 , ATG5 BECN1 , and MAP1LC3C are gene targets associated with autophagy, as predicted using Ingenuity Pathway Analysis software . These miRNAs are significantly decreased in patients with moderately severe PD in the placebo group between baseline and 12 months, indicating an increase in the expression of autophagy genes, suggesting possible changes of autophagy in the progression of PD. These genes were shown to change in animal models treated with nilotinib,, these genes are well characterized for their roles in the initiation and early stages of autophagosome construction for macroautophagy and chaperone-mediated autophagy. An increase in ATG5 and conjugated ATG12 suggests initiation of autophagy, but expression of MAPLC3C indicates accumulation of autophagosomes.,,, Moreover, lysosome-associated membrane protein -1, a component of the lysosome membrane, is the target of hsa-miR-3166, whose expression is significantly increased in placebo-treated patients, suggesting reduction of this lysosomal protein. Together, this pattern of disinhibited and suppressed genes suggests an attempt of neurons to execute autophagic flux and clearance over 1 year, consistent with animal data, and postmortem human brains, showing accumulation of undigested autophagic vacuoles.
Parkinsonism Vs Parkinson’s Disease
Often confused as one and the same, Parkinsons disease is actually the most common kind of Parkinsonism, accounting for nearly 80% of all cases.2 PD is a progressive neurodegenerative disorder characterized by the same motor conditions as Parkinsonisms including tremor, rigidity, bradykinesia, and impaired balance. Other contributing causes of Parkinsonism include multiple system atrophy, progressive supranuclear palsy, and corticobasal degeneration. PD has no directly attributable cause or cure.
Read Also: Average Age Of Parkinson’s Onset
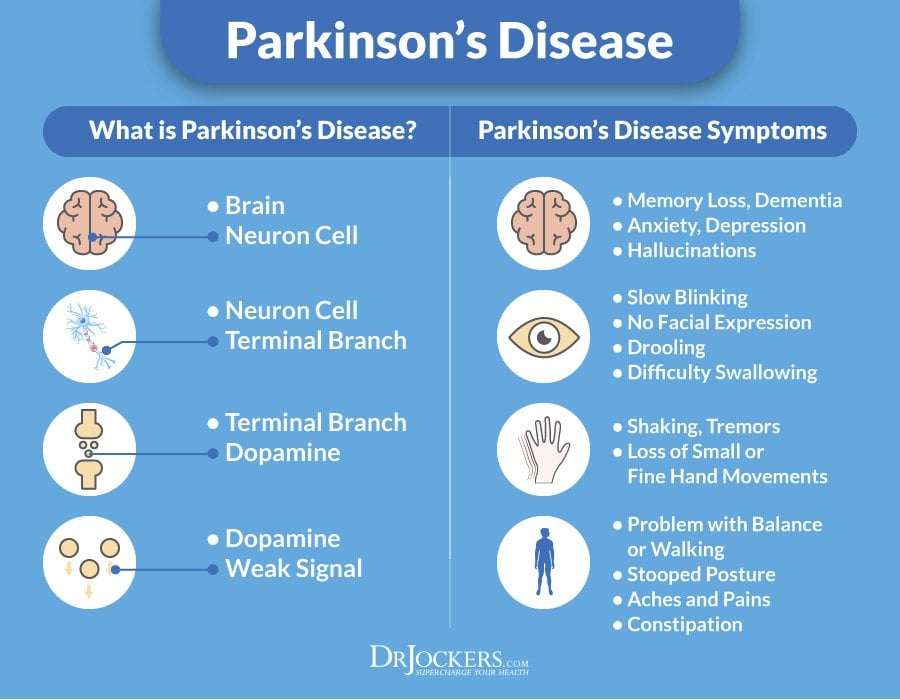
What Causes Parkinsons Disease
Parkinsons disease is caused by a combination of genetic, lifestyle, and environmental factors. A deficiency in the chemical dopamine can cause symptoms of Parkinsons disease.
In about 15% of cases, Parkinsons occurs in individuals with a family history of the disease, due to gene mutations and alterations that are passed down.
Age is a large risk factor for developing Parkinsons. People over the age of 60 have the highest risk of developing the disease.
Studies show that men are 1.5 times more likely to develop Parkinsons than women.
Other environmental risk factors that can lead to Parkinsons include:
- Head injury
- Exposure to pesticides and herbicides
- Exposure to toxins such as trichlorethylene and polychlorinated biphenyls
Is There A Link

Some people have MS and Parkinsonâs, but it could be a coincidence.
Research suggests that the damage that MS causes to your brain can lead some people to develop Parkinsonâs later on.
If you have MS, your immune system triggers ongoing inflammation. This can create lesions in your brain that cause Parkinsonâs disease. If lesions form in certain spots in your brain, they can affect how it makes dopamine.
You May Like: Plan Of Care For Parkinson’s Disease
Nilotinib Regulates Mirnas Associated With Ubiquitination
Changes of miRNAs associated with the ubiquitination pathways were detected only in nilotinib, 300 vs 150 mg and placebo . We observed disinhibition of SQSTM1, SMURF2, FBXW7, BTRC , and SKP1 , which mediate substrate recognition and recruitment for lysosomal degradation. These specific gene targets show that while initiation of lysosomal-autophagy is functioning, nilotinib, 300 mg, is able to facilitate the completion of these biological waste-control mechanisms. Nilotinib, 300 mg, significantly altered a number of ubiquitination genes and ubiquitin ligases, including NEDD4 , UBEs , MDM , and PSMDs as well as deubiquitination genes and ubiquitin-specific proteases , suggesting regulation of the ubiquitination/deubiquitination cycle, in agreement with previous reports., Alterations of autophagy-ubiquitination genes are also concurrent with significant changes of several heat shock proteins and vesicular transport genes , suggesting facilitation of cellular transport and protein clearance.
Jellinger Staging Scheme For Msa
It has been more challenging to stage pathology in MSA and PSP because of the rarity of these disorders and because of their inherent variability. Nevertheless, Jellinger has proposed a staging scheme for MSA that scores severity of striatonigral degeneration and olivopontocerebellar atrophy , each on a three-point scale. The final classification is indicated by an OPCA + SND score . proposed a similar scheme and graphically illustrated the two major MSA types, as well as the overlap in OPCA and SND system degenerations. Ozawa and colleagues used a semiquantitative scoring scheme for lesion density and found differences in the proportion of MSA types in Japanese compared to European autopsy cohorts, with far more OPCA in Japanese . Detection of MSA in neurologically normal individuals is extremely uncommon , and large numbers of such cases would be needed to determine the earliest sites of involvement to develop a staging scheme for MSA analogous to the Braak staging scheme for PD.
You May Like: On Off Phenomenon In Parkinson’s Disease
Treatment For Atypical Parkinsonism Symptoms
Because PD medication response is poor in these syndromes, treatment focuses on symptom management e.g. physical therapy for fall prevention, speech therapy to maximize communication, swallow therapy to prevent aspiration.
Other symptoms that can be addressed include dystonia, myoclonus, blood pressure dysfunction and urinary dysfunction.
Tips and takeaways:
- Atypical parkinsonism is a very complicated group of diseases that are hard to diagnose. Sometimes a neurologist will change the diagnosis as new symptoms develop or become more apparent.
- Despite the fact that these conditions typically do not respond well to medications for PD, many of the presenting symptoms can be addressed, so make sure to raise all of your concerns with your neurologist.
Do you have a question or issue that you would like Dr. Gilbert to explore? Suggest a Topic
Dr. Rebecca Gilbert
APDA Vice President and Chief Scientific Officer
Distribution Of Pathology In Psp
The distribution neuronal loss and neurofibrillary degeneration in PSP was beautifully documented in the original report by Steele, Richardson, and Olszewski based on classic silver staining methods . Modern neuropathologic methods with tau immunohistochemistry have extended these observations, by recognizing glial involvement, as well as greater cortical pathology than noted in the original report, particularly affecting motor and premotor cortices of the frontal lobe . Nevertheless, the cardinal nuclei affected in PSP remain those originally described and include the globus pallidus, subthalamic nucleus, substantia nigra, midbrain tectum, periaqueductal gray, locus ceruleus, and the cerebellar dentate nucleus. Other regions that are consistently affected include corpus striatum, ventrolateral thalamus, red nucleus, pontine and medullary tegmentum, pontine base, and inferior olivary nucleus. Spinal cord involvement is also common, where neuronal inclusions can be found in intermediolateral cell columns. Heterogeneity in the distribution of tau pathology in PSP is increasingly recognized , but a staging scheme remains to be defined. The presence of PSP-like pathology in neurologically normal individuals is uncommon . As in MSA, the paucity of such cases precludes development of staging scheme for PSP.
Also Check: Housing For Parkinson’s Patients
Csf Mirnas Are Not Altered After A Single Dose Of Nilotinib
miRNAs are dynamic regulators of gene expression and may play short- and long-term roles in gene expression. To assess whether miRNAs can be rapidly altered after a single dose of nilotinib, we performed whole-genome miRNA sequencing in the CSF of 75 patients with PD collected after a single oral dose of 150, 200, 300, and 400 mg nilotinib or placebo . Expression profile analysis across all treatment groups shows no short-term effect of nilotinib on miRNA compared with placebo . Only hsa-miR-451a was significantly altered but appears to have no known associated gene targets according to miRTarBase . miRNAs may not require large changes in expression to regulate miRNA targets therefore, we evaluated all miRNAs that met p< 0.05 for treated vs untreated and dose-dependent effects. Even with these relaxed statistical thresholds, there were no miRNAs that show treatment effects compared with placebo after a single dose of nilotinib. In addition, principal component analysis was unable to distinguish treated samples from placebo or any distinct nilotinib treatment groups .
Incidence And Prevalence: Als Compared With Parkinsons
All neurodegenerative diseases are conditions where there is an impact on the brain and/or the central nervous system.
According to statistics, ALS currently affects around 30,000 people in the USA, with around 6,000 new cases being identified each year.
Parkinsons Disease affects around a million people in America and there are about 60,000 new cases annually.
Famous individuals affected by Parkinsons include Michael J Fox and Scottish comedian Billy Connelly. In terms of ALS, the late Professor Stephen Hawking was one prominent public figure who had been diagnosed with a form of ALS. The late legendary US baseball player Lou Gehrig was also diagnosed with ALS and subsequently the condition has been commonly referred to as Lou Gehrigs disease ever since.
Parkinsons is perhaps a much more well known condition, due to its increased prevalence throughout the world, however ALS has received a lot more attention and awareness since the Ice Bucket Challenge which went viral on social media during the summer of 2014.
Recommended Reading: What Can Mimic Parkinson’s Disease
Understanding The Differences Between Parkinsonism And Parkinson Plus Syndromes
Parkinsonism means looks like Parkinsons disease. To neurologists this means that the person has a somewhat flexed posture, moves slowly, is stiff and usually walks slowly, with small steps and reduced or no arm swing. We call the syndromes atypical because they usually differ from Parkinsons Disease in a few ways:
Very often when the condition is mild, at the earliest stages, we cant tell whether it is Parkinsons Disease or atypical Parkinsons Disease and we treat it as if it is Parkinsons Disease because we dont have treatments for the atypical Parkinson disorders. Sometimes they respond to the usual Parkinsons Disease medications, but usually they dont. And when they do, the response is not as good as it is with PD.
Parkinson plus syndromes refer to syndromes which look like atypical PD, but also include additional abnormalities that are not seen in PD. These include: abnormalities of eye movements, gait ataxia , dystonia , severe problems with low blood pressure on standing, or changes on the neurological exam that are only detected by the neurologist in the form of abnormal reflexes.
Is Parkinsons Disease Inherited
Scientists have discovered gene mutations that are associated with Parkinsons disease.
There is some belief that some cases of early-onset Parkinsons disease disease starting before age 50 may be inherited. Scientists identified a gene mutation in people with Parkinsons disease whose brains contain Lewy bodies, which are clumps of the protein alpha-synuclein. Scientists are trying to understand the function of this protein and its relationship to genetic mutations that are sometimes seen in Parkinsons disease and in people with a type of dementia called Lewy body dementia.
Several other gene mutations have been found to play a role in Parkinsons disease. Mutations in these genes cause abnormal cell functioning, which affects the nerve cells ability to release dopamine and causes nerve cell death. Researchers are still trying to discover what causes these genes to mutate in order to understand how gene mutations influence the development of Parkinsons disease.
Scientists think that about 10% to 15% of persons with Parkinsons disease may have a genetic mutation that predisposes them to development of the disease. There are also environmental factors involved that are not fully understood.
Read Also: Is Drooling A Sign Of Parkinson’s Disease
How Are They Alike
MS and Parkinsonâs both affect your central nervous system, which includes your brain and spinal cord. Thatâs why they both can affect how you move, sleep, feel, and talk.
These diseases both affect your nerves. MS can break down the coating, called myelin, that surrounds and protects your nerves. In Parkinsonâs, nerve cells in a part of your brain slowly die off.
Both can start out with mild symptoms, but they get worse over time.
Common symptoms of both diseases include:
- Shaky fingers, hands, lips, or limbs
- Slurred speech thatâs hard for others to understand
- Numb or weak limbs that make your walk unsteady
- Loss of muscle control that often affects one side of your body at first, then later both
- Spastic limb movements that are hard to control
- Loss of bladder or bowel control
- Poor balance
Depression is another symptom common to both conditions.