Parkinsons Disease Vs Als: Us Prevalence
One million Americans live with Parkinsons disease. The average cost of Parkinsons disease including treatment, lost work wages, and social security payments is $25 billion annually in the U.S.
It is not clear how many people are affected by ALS, but the estimates range between 12,000 and 15,000. Doctors tell roughly 5,000 patients annually that they have ALS. Records on ALS have not been well kept across the country, so estimates may fall way below the actual rates. Common age of ALS diagnosis is between 55 and 75, and life expectancy is anywhere between two and five years after the onset of symptoms. Longevity in ALS is strongly linked to a persons age. Younger individuals with ALS tend to live longer than those diagnosed at an older age.
Which Test Can Be Done When The Diagnosis Is In Doubt
I request a small set of tests on almost all patients I diagnose with Parkinsons. These detect some mimics of Parkinsons disease.
Some doctors dont request all these tests. And for a good reason.
The diagnosis of Parkinsons mimics is primarily based on a careful history and examination. Even in my practice, these tests change the diagnosis only in a minority of patients.
I like the additional confirmation provided by these tests. They also have other benefits. For example, they help me determine the proper dosages of medications like Amantadine.
| Simple tests to detect Parkinsons Mimics |
|---|
| 1. MRI-Brain with size measurements of brain parts called the midbrain and pons. I usually also request a unique picture called SWI, which shows iron inside the brain.
2. Blood tests: |
But when the diagnosis s really in doubt, there is another brain scan that can be done.
A Trodat scan. Or even better an F-DOPA scan. Both these scans measure dopamine activity inside the brain.
You can read more about Trodat & F-DOPA scans by clicking here.
These scans are not perfect. Let me tell you why very quickly:
In Parkinsons disease, dopamine activity inside the brain is deficient. This deficiency produces an abnormal scan. If the Trodat/F-DOPA scan is normal, it is unlikely that you have Parkinsons disease.
Transcranial Direct Stimulation In Parkinson’s Disease Gait Rehabilitation
| This article is an orphan, as no other articles link to it. Please introduce links to this page from related articles try the Find link tool for suggestions. |
Gait variability seen in Parkinson‘s Disorders arise due to cortical changes induced by pathophysiology of the disease process. Gait rehabilitation is focused to harness the adapted connections involved actively to control these variations during the disease progression. Gait variabilities seen are attributed to the defective inputs from the Basal Ganglia. However, there is altered activation of other cortical areas that support the deficient control to bring about a movement and maintain some functional mobility.
Don’t Miss: How Long Do Parkinson’s Patients Live After Diagnosis
Parkinsons Disease Vs Als: Risk Factors And Complications
Risk factors for Parkinsons disease include being over the age of 50, being male, having a family history of Parkinsons disease, carrying gene variations, experiencing a head injury, being exposed to environmental toxins, and taking certain medications such as anti-anxiety medications or sleeping pills.
Complications associated with Parkinsons disease include difficulty thinking, depression, emotional changes, swallowing problems, sleep problems and disorders, bladder issues, constipation, changes in blood pressure, smell dysfunction, fatigue, pain, and sexual dysfunction.
Studies into ALS have revealed some interesting insight. For example, it may just be that some people with this disease are triggered by certain environmental factors. The environmental triggers under investigation include smoking, lead exposure, and military service. Recent research has indicated that people who have served in the military are at a higher risk of getting ALS.
Studies are also looking at the entire human genome, since research has uncovered a number of genetic variations that people with familial ALS and some with non-inherited ALS have in common. These variations might make people more prone to ALS.
Imaging Biomarkers In Parkinsonism
DaTscan: dopamine-active transporter scans showing binding of 123I-fluoropropyl to DaT protein in the nigrostriatal nerve endings of the striatum. Normal: symmetrical normal specific binding of FPCIT in striatum. Parkinson’s disease: reduced specific binding of FPCIT in the posterior striatum, particularly on the left .
Further imaging approaches are in development on a research basis. 7-T MR scanning can detect structural nigral abnormalities. Diffusion-tensor MRI and diffusion-weighted imaging have shown some promise in diagnosing PD and its mimics. Transcranial sonography can detect hyperechogenicity in the midbrain of patients with PD. Although this is not specific, it may be a marker of susceptibility to PD.,,
Recommended Reading: Parkinson’s Dry Mouth Treatment
How Is Psp Diagnosed
Currently there are no tests or brain imaging techniques to definitively diagnose PSP. An initial diagnosis is based on the persons medical history and a physical and neurological exam. Identifying early gait problems, problems moving the eyes, speech and swallowing abnormalities, as well as ruling out other similar disorders is important. Diagnostic imaging may show shrinkage at the top of the brain stem and look at brain activity in known areas of degeneration.
How Is Parkinsonism Diagnosed
You should be referred to a Parkinsons specialist for the diagnosis of any parkinsonism. They may wish to explore different things before giving you a diagnosis.
Your specialist will look at your medical history, ask you about your symptoms and do a medical examination.
Telling the difference between types of parkinsonism isnt always easy, for the following reasons:
- The first symptoms of the different forms of parkinsonism are so similar.
- In many cases, parkinsonism develops gradually. Symptoms that allow your doctor to make a specific diagnosis may only appear as your condition progresses.
- Everyone with parkinsonism is different and has different symptoms.
Find out more: see our information on symptoms of Parkinsons, and diagnosing Parkinsons.
One of the most useful tests to find out what sort of parkinsonism you may have is to see how you respond to treatment.
If your specialist thinks you have idiopathic Parkinsons, theyll expect you to have a good response to Parkinsons drugs such as levodopa . A good response means that your symptoms will improve. Sometimes, it will only be clear that youve responded to medication when the drug is reduced or stopped, and your symptoms become more obvious again.
If you dont have any response to Parkinsons medication, your specialist will have to look again at your diagnosis.
Although not routinely available, your specialist may wish to carry out some of the tests below.
Current tests available include:
Don’t Miss: Stages Of Parkinson’s What To Expect
Thanks For Signing Up
We are proud to have you as a part of our community. To ensure you receive the latest Parkinsons news, research updates and more, please check your email for a message from us. If you do not see our email, it may be in your spam folder. Just mark as not spam and you should receive our emails as expected.
Is There Any Treatment
There is currently no effective treatment for PSP and symptoms usually do not respond to medications.
- Parkinsons disease medications, such as ropinirole, rarely provide additional benefit. In some individuals, other antiparkinsonian medications, such as levodopa, can treat the slowness, stiffness, and balance problems associated with PSP, but the effect is usually minimal and short-lasting.
- Botulinum toxin, which can be injected into muscles around the eyes, can treat excessive eye closing.
- Some antidepressant drugs may offer some benefits beyond treating depression, such as pain relief and decreasing drooling.
Non-drug treatment for PSP can take many forms.
- Weighted walking aids can help individuals avoid falling backward.
- Bifocals or special glasses called prisms are sometimes prescribed for people with PSP to remedy the difficulty of looking down.
- Exercise supervised by a healthcare professional can keep joints limber but formal physical therapy has no proven benefit in PSP.
A gastrostomy may be necessary when there are swallowing disturbances or the definite risk of severe choking.
Deep brain stimulationwhich uses surgically implanted electrodes and a pacemaker-like medical device to deliver electrical stimulation to specific areas in the brain to block signals that cause the motor symptoms of several neurological disordersand other surgical procedures commonly used in individuals with Parkinson’s disease have not
Also Check: Social Security Blue Book Parkinson’s
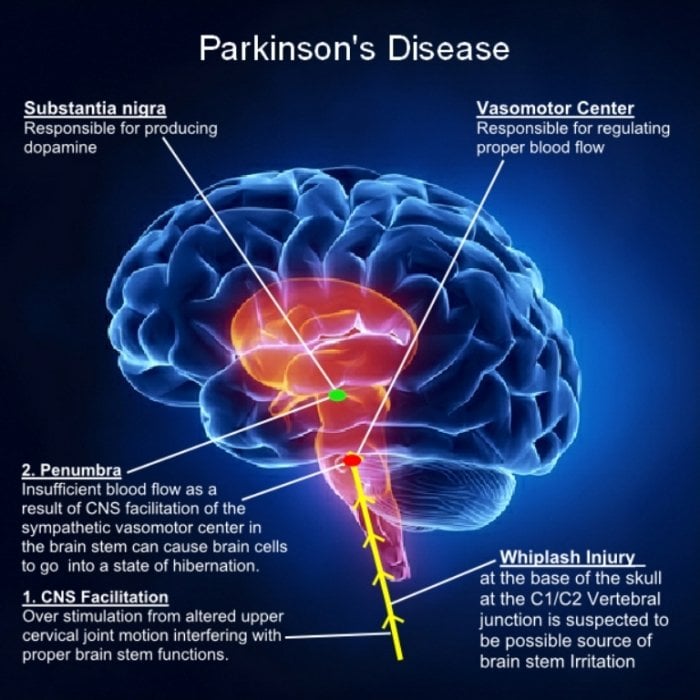
What Causes Parkinson Disease
Parkinson disease arises from decreased dopamine production in the brain. The absence of dopamine makes it hard for the brain to coordinate muscle movements. Low dopamine also contributes to mood and cognitive problems later in the course of the disease. Experts don’t know what triggers the development of Parkinson disease most of the time. Early onset Parkinson disease is often inherited and is the result of certain gene defects.
Comparing Parkinsons Disease And Als Causes
When certain nerve cells in the brain begin to die or break down that is what causes Parkinsons disease, but why this occurs is unclear. Some factors that contribute to nerve cell death include genetics as specific gene mutations have been identified to contribute to Parkinsons disease, environmental factors such as exposure to certain toxins, the presence of Lewy bodies in the brain, as well as alpha-synuclein found in Lewy bodies.
There are many unanswered questions about ALS, including the root cause. What we do know is that nerve cells that control the movement of muscles gradually die in ALS patients.
Researchers around the world continue to investigate the possible causes of ALS, including whether the immune system plays a role in attacking the body cells, potentially killing nerve cells. Scientists are examining chemical imbalance and trying to determine if proteins in people with ALS are being incorrectly processed by nerve cells.
Environmental factors are also being put under the scrutiny. One study has stated that members of the military personnel in the Gulf region during the 1991 war were more likely to develop Lou Gehrigs disease than military personnel stationed anywhere else. The question is, could mechanical or electrical trauma, exposure to high levels of exercise, exposure to high levels of agricultural chemicals, or heavy metals play a role?
You May Like: Insomnia And Parkinson’s Disease
Tdcs Mechanism In Parkinson Disease
Transcranial Direct Current stimulation is thought to restore the neural activity in motor and prefrontal Cortices in PD. It promotes Motor learning and Consolidation and may enhance long-term retention. This is the basic rationale of using tDCS for neuro rehabilitative procedures in PD.
tDCS works on the concept of priming which depends on pre-existing neural activity referred to as homeostatic plasticity. This effect on plasticity produce persistent effects. This makes it a useful tool to be combined with another non-invasive brain stimulation technique like rTMS. Cathodal tDCS lowers the excitability of cortex thereby reversing the inhibition of low frequency rTMS whereas Anodal tDCS increases cortical excitability reversing facilitation of High frequency rTMS. Dopamine also primes the brain activity with anodal tDCS into inhibition. Though this remains to be tested.
Cortical Silent Period reflects excitability of motor cortex involved in inhibitory circuits. IN PD CSP is shortened during OFF period and normalized on medications and lengthened in dyskinetic state. It correlates with UPDRS motor score. However, tDCS effects on CSP is not yet known.
Role of Tdcs to induce dopamine release is not yet known. As anodal tDCS is known to cause widespread activation it may trigger some effects. It is also assumed that dopamine plays a role in acute effects of Tdcs.
Movement Disorders Similar To Parkinsons
Conditions causing excess movement or decreased movement that are sometimes associated with Parkinson’s disease-like symptoms include:
What Movement Disorder Could I Have?
When making a Parkinson’s diagnosis, your doctor will review your medical history and symptoms, perform a careful neurological exam, and, if necessary, carry out further tests to rule out other movement disorders.
Your symptoms may be caused by a movement disorder other than Parkinson’s disease if:
- You display Parkinson’s disease symptoms and features that are characteristic of an additional movement disorder.
- The results of a brain imaging study or laboratory test, such as a blood test, confirm the presence of another movement disorder.
- Your symptoms do not respond to Parkinson’s disease medication.
Because movement disorders are not all treated the same way, it is important to get a proper diagnosis as early as possible so you can formulate the right treatment plan with your doctor.
You May Like: Alternative Treatment For Parkinson’s Disease
What Is Parkinsons Disease
Parkinson’s disease belongs to a group of conditions called motor system disorders, which are the result of the loss of dopamine-producing brain cells. Parkinson’s disease is a brain disorder that leads to shaking, stiffness, and difficulty with walking, balance, and coordination. Symptoms generally develop slowly over years. Parkinson’s symptoms usually begin gradually and get worse over time.
What Causes The Condition
First described in 1917 by James Parkinson as the shaking palsy, PD is characterized by a loss of neurons in the substantia nigra portion of the brain. A buildup of the protein alpha-synuclein causes dopamine producing cells to fail and die. There is no known specific cause of PD but it is considered to be a combination of genetic and environmental factors just like PSP.
Don’t Miss: Reishi Mushroom Parkinson’s Disease
What Are The Symptoms
PSP affects movement, control of walking and balance, speech, swallowing, eye movements and vision, mood and behavior, and thinking. The pattern of signs and symptoms can be quite different from person to person. The most frequent first symptom of PSP is a loss of balance while walking. Individuals may have abrupt and unexplained falls without loss of consciousness, a stiff and awkward gait, or slow movement.
As the disease progresses, most people will begin to develop a blurring of vision and problems controlling eye movement. These symptoms may include:
- Slow eye movements.
What Causes Parkinson’s Disease
Parkinson’s disease occurs when nerve cells, or neurons, in an area of the brain that controls movement become impaired and/or die. Normally, these neurons produce an important brain chemical known as dopamine. When the neurons die or become impaired, they produce less dopamine, which causes the movement problems of Parkinson’s. Scientists still do not know what causes cells that produce dopamine to die.
People with Parkinson’s also lose the nerve endings that produce norepinephrine, the main chemical messenger of the sympathetic nervous system, which controls many functions of the body, such as heart rate and blood pressure. The loss of norepinephrine might help explain some of the non-movement features of Parkinson’s, such as fatigue, irregular blood pressure, decreased movement of food through the digestive tract, and sudden drop in blood pressure when a person stands up from a sitting or lying-down position.
Many brain cells of people with Parkinson’s contain Lewy bodies, unusual clumps of the protein alpha-synuclein. Scientists are trying to better understand the normal and abnormal functions of alpha-synuclein and its relationship to genetic mutations that impact Parkinsons disease and Lewy body dementia.
You May Like: Parkinson’s Donations In Memory Of
General Approach To Management
The primary goal in the management of PD is to treat the symptomatic motor and nonmotor features of the disorder, with the objective of improving the patients overall quality of life. Appropriate management requires an initial evaluation and diagnosis by a multidisciplinary team consisting of neurologists, primary care practitioners, nurses, physical therapists, social workers, and pharmacists., It is also important that the patient and his or her family have input into management decisions.
Effective management should include a combination of nonpharmacological and pharmacological strategies to maximize clinical outcomes. To date, therapies that slow the progression of PD or provide a neuroprotective effect have not been identified., Current research has focused on identifying biomarkers that may be useful in the diagnosis of early disease and on developing future disease-modifying interventions.,
Symptoms Of Parkinsons Disease
Parkinson’s disease has four main symptoms:
- Tremor in hands, arms, legs, jaw, or head
- Stiffness of the limbs and trunk
- Slowness of movement
- Impaired balance and coordination, sometimes leading to falls
Other symptoms may include depression and other emotional changes difficulty swallowing, chewing, and speaking urinary problems or constipation skin problems and sleep disruptions.
Symptoms of Parkinsons and the rate of progression differ among individuals. Sometimes people dismiss early symptoms of Parkinson’s as the effects of normal aging. In most cases, there are no medical tests to definitively detect the disease, so it can be difficult to diagnose accurately.
Early symptoms of Parkinson’s disease are subtle and occur gradually. For example, affected people may feel mild tremors or have difficulty getting out of a chair. They may notice that they speak too softly, or that their handwriting is slow and looks cramped or small. Friends or family members may be the first to notice changes in someone with early Parkinson’s. They may see that the person’s face lacks expression and animation, or that the person does not move an arm or leg normally.
People with Parkinson’s often develop a parkinsonian gait that includes a tendency to lean forward, small quick steps as if hurrying forward, and reduced swinging of the arms. They also may have trouble initiating or continuing movement.
Read Also: How To Prevent Getting Parkinson’s Disease
What Are Atypical Parkinsonian Disorders
Atypical Parkinsonian disorders are progressive diseases that present with some of the signs and symptoms of Parkinsons disease, but that generally do not respond well to drug treatment with levodopa. They are associated with abnormal protein buildup within brain cells.
The term refers to several conditions, each affecting particular parts of the brain and showing a characteristic course:
- Dementia with Lewy bodies, characterized by an abnormal accumulation of alpha-synuclein protein in brain cells
- Progressive supranuclear palsy, involving tau protein buildup affecting the frontal lobes, brainstem, cerebellum and substantia nigra
- Multiple system atrophy, another synucleinopathy that affects the autonomic nervous system , substantia nigra and at times the cerebellum
- Corticobasal syndrome, a rare tauopathy that typically affects one side of the body more than the other and makes it difficult for patients to see and navigate through space