Clinical Evaluation Of Non
The following symptoms were assessed: hyposmia, neuropsychiatric disorders , autonomic dysfunctions , and sleep disturbances . A clinical interview was conducted to determine the presence of each NMS at the time of the examination. Informations on the current use of medications, such as laxatives, hypnotics, or antidepressants to treat some of these NMS, were also collected.
Smell loss was assessed by the validated Argentina Hyposmia Rating Scale starting by asking the subjects whether they noted a change in their ability to smell. Patients with factors that could impair odor identification, such as: current smokers, medical history of nasal surgery , allergic rhinitis, and traumatic nasal injuries were eliminated. According to these criteria, our sample for this test was restricted to 51 patients . Hyposmia was considered to be present if the AHRS score was lower than 22.
To evaluate the presence of depression and its severity, we used the MontgomeryAsberg Depression Rating Scale . The cut-off scores we used were: < 7 absent signs, mild signs = 718, moderate = 1834, and 35 reflects severe depression. This scale consistently has the highest Cronbachs alpha levels reaching 0.92 . Patients with severe depression were excluded from the study. Patients with scores 7 were considered having depression.
Symptoms That Are Commonly Associated With Pd
These symptoms include sleep disorders, abnormalities in blood pressure, urinary problems, constipation, depression, and anxiety. Even though these symptoms are so commonly seen in PD, they are also commonly associated with other issues that have nothing to do with PD, so it is vital to keep an open mind about their cause. If any symptom is new or worsening, it could be an indication of a new medical problem. For example, urinary problems are extremely common in PD, but may be a sign of an enlarged prostate, which can be treated in an entirely different way.
Rem Sleep Behavioral Disorder
Rapid eye movement, or REM, sleep is a normal part of the sleep cycle when people dream. Usually the only part of the body that moves during REM is the eyes, thus the name.
- People with rapid eye movement sleep behavior disorder do not have the normal relaxation of the muscles during their dreams. Therefore, they act out their dreams during REM sleep.
- People with RBD may shout, kick their bed partner or grind their teeth. Sometimes, in moderate to severe RBD, people may have aggressive, violent behaviors, like getting out of bed and attacking their bed partner.
- About half of people with PD suffer from RBD. It may develop after or along with the disease, but in most cases, it precedes the PD diagnosis by five to 10 years.
RBD Treatment
- Consider making environmental adjustments to protect the person with RBD and bed partner from injury. This may include padding the floor, using bed rails or sleeping in separate rooms.
- Clonazepam has been shown in large case series to improve RBD in 80 to 90 percent of cases. The dose of clonazepam required is low, usually from 0.5 mg to 1.0 mg. The adverse effects of clonazepam include nocturnal confusion, daytime sedation, and exacerbation of obstructive sleep apnea, if present. It is in generic form and not expensive.
- Talk to your doctor about the over-the-counter sleep aid Melatonin. Doses up to 12 mg at night one hour before can improve RBD.
You May Like: Pre Parkinson’s Disease Symptoms
Initiatives To Address Management Of Non
Parkinson’s UKthe major UK-based patient charitycommissions an annual audit of Parkinson services. The 2011 report showed non-motor symptoms recorded in only 21% of elderly care and 9% of neurology services in the UK. This deficiency mainly relates to lack of time during consultation and also to not using self-declaration tools, which would allow patients to flag symptoms. This outcome led to a national policy for data collection of patients being referred to hospital.
What Are The Primary Motor Symptoms Of Parkinsons Disease
There are four primary motor symptoms of Parkinsons disease: tremor, rigidity, bradykinesia and postural instability . Observing two or more of these symptoms is the main way that physicians diagnose Parkinsons.
It is important to know that not all of these symptoms must be present for a diagnosis of Parkinsons disease to be considered. In fact, younger people may only notice one or two of these motor symptoms, especially in the early stages of the disease. Not everyone with Parkinsons disease has a tremor, nor is a tremor proof of Parkinsons. If you suspect Parkinsons, see a neurologist or movement disorders specialist.
Tremors
Rigidity
Bradykinesia
Postural Instability
Walking or Gait Difficulties
Dystonia
Vocal Symptoms
Read Also: Drugs That Can Mimic Parkinson’s Disease
Podcast Episode : Neuropathy: A Non
Neuropathy is a broad category of non-motor symptoms of Parkinsons disease , basically resulting from damage or dysfunction of one or more nerves. It typically may result in numbness, tingling , pain, or weakness in the area served by the specific nerve or nerves. Some pain sensations may be sharp, burning, or throbbing. According to the Cleveland Clinic, about 25% to 30% of Americans will be affected by some degree of neuropathy over their lives, especially as they age. Common risk factors are diabetes, metabolic syndrome, heavy alcohol use, as well as tasks requiring repetitive motions. Neuropathies frequently start in the hands or feet but may occur in other body sites as well.
Neuropathy occurs more frequently among people with PD compared to those without PD, and the reasons are not entirely clear. PD itself may be a factor in neuropathy, and levodopa may contribute to lower vitamin B12 levels, leading to neuropathy. However, not all neuropathies experienced by people with PD are necessarily part of the disease or its treatment, so it is important to have a good medical work-up to determine the cause of the symptoms, some of which may be treatable.
*Please note that not all content is available in both languages. If you are interested in receiving Spanish communications, we recommend selecting both” to stay best informed on the Foundation’s work and the latest in PD news.
Thanks For Signing Up
We are proud to have you as a part of our community. To ensure you receive the latest Parkinsons news, research updates and more, please check your email for a message from us. If you do not see our email, it may be in your spam folder. Just mark as not spam and you should receive our emails as expected.
Recommended Reading: Exercise Class For Parkinson’s Disease
Motor And Nonmotor Symptoms Of Parkinsons Disease: Antagonistic Pleiotropy Phenomena Derived From
Makoto Hashimoto
1Tokyo Metropolitan Institute of Medical Science, 2-1-6 Kamikitazawa, Setagaya-ku, Tokyo, Japan
2PCND Neuroscience Research Institute, Poway, CA, USA
3Department of Physiology, Nippon Medical School, Tokyo, Japan
4Institute of Agrobiological Sciences, National Agriculture and Food Research Organization, Tsukuba, Ibaraki, Japan
5Department of Neuroscience, National Institute on Aging, Bethesda, MD 20892, USA
Abstract
1. Introduction
It is well established that synucleinopathies, including PD, DLB, and MSA, are characterized by a number of NMS, such as cognitive impairment, depression and anxiety, sleep difficulties, gastrointestinal disturbance, and autonomic failure. Because some NMS occur in the prodromal disease stages, NMS are both mechanistically and therapeutically important . Recently, in this field, there has been great interest in better understanding NMS, a topic which has been prominently reviewed . Nevertheless, the mechanisms which underlie NMS in neurodegenerative diseases remain obscure.
2. Motor and Nonmotor Symptoms in Synucleinopathies
3. Are NMS Passive Phenomena?
4. NMS as Active Phenomena Dependent on Evolvability and Antagonistic Pleiotropy
5. Modulation of NMS Evolvability by Other Factors
6. Therapeutic Implication
7. Conclusions
Conflicts of Interest
How Do I Know If I Have A Speech Or Voice Problem
- My voice makes it difficult for people to hear me.
- People have difficulty understanding me in a noisy room.
- My voice issues limit my personal and social life.
- I feel left out of conversations because of my voice.
- My voice problem causes me to lose income.
- I have to strain to produce voice.
- My voice clarity is unpredictable.
- My voice problem upsets me.
- My voice makes me feel handicapped.
- People ask, “What’s wrong with your voice?”
Also Check: How Long Do You Live With Parkinson’s Disease
Finding The Right Treatment
The long list of Parkinson’s non-motor symptoms includes constipation, memory and thinking changes, low blood pressure, depression or anxiety, sleep problems and others. A number of therapies are available to treat Parkinson’s disease non-motor symptoms, but many patients are left wanting not responding well to therapies or seeing enough relief. Some drugs are approved by the U.S. Food and Drug Administration to treat these conditions in people with PD. Most, however, are FDA-approved for the general population but have not been studied in large numbers of people with PD. Still, doctors commonly prescribe them, and people with Parkinson’s often find them beneficial.
Here we describe Parkinson’s non-motor symptom treatments. With all Parkinson’s symptoms, discuss treatment options with your doctor and work together to find a regimen that fits your needs.
Dementia
Parkinson’s disease dementia is when memory or thinking changes interfere with a person’s job, daily activities or social interactions.
How Is Daytime Sleepiness Treated
Consider making certain lifestyle modifications, such as:
- Establish good sleep hygiene, including a set bedtime and wake-up time.
- Get exposure to adequate light during the day and darkness at night.
- Remember indoor lighting may not be sufficient to promote a normal circadian rhythm.
- Avoid sedentary activities during the day.
- Participate in activities outside the home. They may help provide stimulation to prevent daytime dozing.
- Get physical exercise appropriate to your level of functioning, which may also promote daytime wakefulness. Strenuous exercise, however, should be avoided six hours before sleep.
- Do NOT drive while sleepy if you experience excessive daytime sleepiness. Motor vehicle accidents increase during periods of drowsiness and may be associated with sudden onset of sleep .
- Talk to your doctor about possibly decreasing the dosage of dopamine agonists if you experience daytime sleepiness or sleep attacks.
- Talk to your doctor about decreasing stimulants like caffeine, modafinil and methylphenidate .
Don’t Miss: Parkinson’s Big Movement Exercises
Symptoms That May Be Related To Pd
These symptoms can be associated with PD, but are also commonly associated with other medical conditions, so more testing is necessary. For example, weight loss may be associated with PD, but may also be a sign of a gastrointestinal problem or cancer. Pain may be associated with PD, but could be also due to arthritis, spinal stenosis, cancer, or a whole host of other causes.
There is a fourth category of non-motor symptoms that I would like to focus on now:
Symptoms That May Be Related To Pd But That Few People Know About
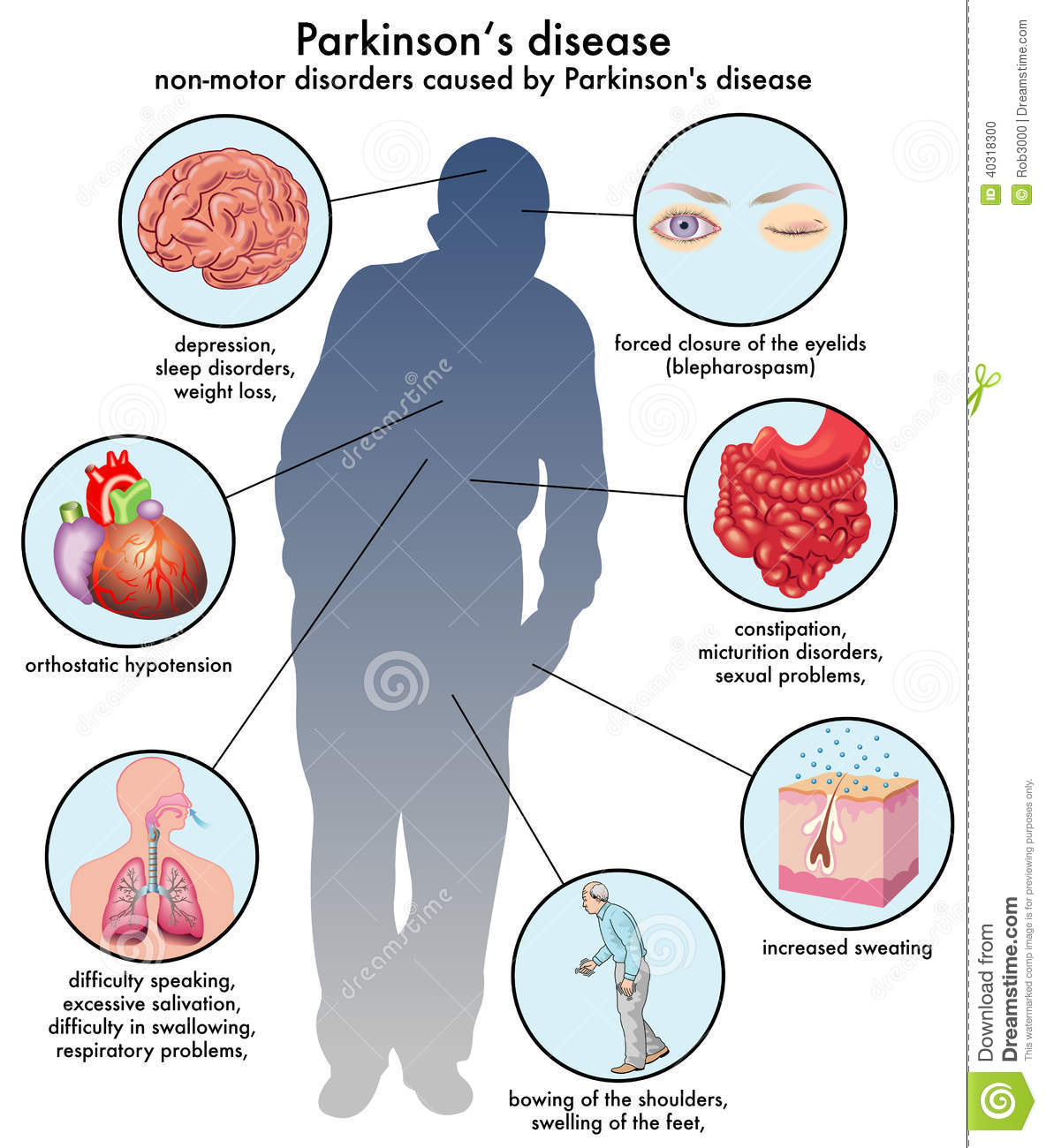
People with PD and care partners may suspect that a particular symptom is related to PD, but they cant find information about it, so they are not sure. Two symptoms that pop up in this category are runny nose and breathing problems, which well focus on today. Of course, if these are new symptoms for you, they could be indicative of a new problem, including infection with COVID-19, so make sure to get yourself checked out by your doctor. However, if all else is ruled out, PD could be to blame. Excessive sweating and specific skin disorders are in this category as well and have been addressed previously.
Don’t Miss: All About Parkinson’s Disease
Lessening Dyskinesia With Duodopa Linked To Better Quality Of Life
Parkinsons disease is characterized by the loss of dopamine-producing nerve cells, those responsible for releasing the neurotransmitter dopamine, a chemical messenger that allows nerve cells to communicate and also helps to regulate movement.
A short supply of dopamine in the brain causes both motor and non-motor symptoms observed in Parkinsons.
Levodopa, which is a precursor to dopamine, has long been one of the gold standards for Parkinsons treatment. It is converted into dopamine in the brain, since dopamine itself cannot cross the brain-blood barrier, a semi-permeable membrane that shields the brain from potential disease-causing pathogens and toxins that may be present in blood.
However, long-term levodopa therapy often results in dyskinesia, the involuntary and jerky movements that occur in Parkinsons patients.
Gocovri is a long-acting and extended-release capsule that is recommended for those receiving levodopa-based therapy, with or without other dopaminergic medications. It was the first therapy approved in the United States for levodopa-induced dyskinesia. Its extended-release capsules treat dyskinesia, and can be used as an add-on treatment for off episodes, periods characterized by the reappearance or worsening of motor symptoms due to a gradual decline in levodopas effectiveness.
The Neuropathological Basis Of Non
For the nigrostriatal dopaminergic disorder of PD, one pathological process clearly does not fit all! Jellinger stated that Parkinson’s can no longer be considered a complex motor disorder characterised by extrapyramidal symptoms, but as a progressive multisystem diseaseor more correctly, multiorgan diseasewith variegated neurological and non-motor deficiencies.
The traditional concept that the first neuropathological insult leading to PD is the degeneration of neuromelanin-containing neurones in the pars compacta of the substantia nigra has been challenged. Many studies, spearheaded by the Braak theory, suggest that a non-dopaminergic process is key to the non-motor symptoms of PD, many of which start well before the motor Parkinson’s features emerge. Interestingly, Friedrich Lewy first described Lewy bodies in the dorsal motor nucleus of the vagus, a site implicated in Braak stage 2.
summarises the growing evidence that in PD the degeneration of non-dopaminergic neurones occurs well before dopaminergic motor symptoms start. There is also clear evidence of differential neuronal degeneration involving several neuropeptide pathways in the brain in PD., Furthermore, there is neuropathological heterogeneity between early-onset and late-onset PD, which manifests clinically as subtypes within both motor PD and non-motor PD.
OHDA, hydroxydopamine MPTP, 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine.
Recommended Reading: Parkinson’s Disease And Cognition
How Parkinsons Disease Causes Primary Motor Symptoms
PD damages the neurons in the brain, especially an area of the brain called the substantia nigra pars compacta. The neurons in the substantia nigra produce dopamine, a neurotransmitter that transmits signals from the substantia nigra to other parts of the brain to produce smooth, purposeful movement. When the neurons in the substantia nigra are damaged in large numbers, the loss of dopamine causes impaired movement and the motor symptoms of PD: tremor, rigidity, impaired balance, and loss of spontaneous movement. Research has shown that people with PD have lost 60-80% or more of the neurons that produce dopamine by the time symptoms appear.1,4,5
Iron And Neuromelanin Sensitive Mri
T2* weighted Imaging
Histochemical studies have demonstrated elevated iron accumulation in the SN in PD patients . MRI scan sequences can quantify iron due to its paramagnetic property which changes the relaxation behavior of tissue and introduces changes in susceptibility and microscopic field gradients . Specifically, iron levels in vivo cause signal changes in T2 and T2*, and can be quantified in a variety of ways , with initial focus on relaxation rates , collectively referred to as relaxometry . Using these early measures, PD demonstrated elevated iron levels in the SN . Increased iron levels observed postmortem were related to the R2* values . A combination of R2* measures and diffusion metrics have been helpful in differentiating PD and APD . There have been mixed reports of whether R2* can capture PD progression .
Nigrosome Imaging
Neuromelanin Imaging
In summary, all of these measures have high sensitivity and specificity in distinguishing PD relative to controls with inconsistent results differentiating PD from APD . While nigrosome imaging is sensitive to changes early in the disease course , it may be limited changes after the initial decline early in the course of PD. In contrast, NM-MRI, T2* and QSM measures of the nearby regions may better characterize change over time and serve as useful monitoring markers.
You May Like: Big And Loud Therapy For Parkinson’s
Some Tips To Help With Excessive Sweating Include:
- Stay hydrated
- Wear lightweight, loose-fitting clothing made from cotton or other natural fibers
- Choose clothing that doesnt show sweat
- Identify and reduce consumption of foods that may trigger sweating
- Identify and reduce stressors that cause sweating
If you are experiencing excessive sweating, have a conversation with your healthcare provider to explore how to specifically address this.
It is less frequently reported, but some people with Parkinsons may experience too little sweating or hypohidrosis, which could be a side effect of an anticholinergic Parkinsons medication. Too little sweating can have a negative impact on your ability to control your bodys temperature and thus put you at risk for overheating.
If your sweating begins to negatively impact your daily life, consider consulting with your doctor to discuss adjusting your medication or other treatments, such as botulism toxin injections for excessive sweating.
What Are The Non
Parkinsons is officially classified as a movement disorder because it involves damage to the areas of the brain, nerves and muscles that influence the speed, quality, fluency and ease of movement. While the effects of Parkinsons on movement are often the most visible symptoms, like tremor, non-motor symptoms of Parkinsons, like emotional and cognitive challenges, can sometimes have an even greater effect on your quality of life.
The effects of Parkinsons not related to movement are called non-motor symptoms. Non-motor symptoms of Parkinsons may actually outnumber motor symptoms and can appear years before motor symptoms.
In this article, we will help you identify and learn about the various non-motor symptoms of Parkinsons so you can take the first steps to living well.
Non-motor symptoms of Parkinsons are effects not related to movement.
There is a wide variety of possible non-motor symptoms of Parkinsons, ranging from physiological effects like trouble swallowing, pain and fatigue, to mental and emotional impacts, such as mood changes, cognitive challenges and anxiety. Just as Parkinsons affects everyone differently, the type, frequency and severity of non-motor symptoms each person experiences vary. Remember, just because something is listed as a non-motor symptom of Parkinsons does not mean you will experience it.
Its a lot harder to explain the Parkinsons that people dont see. Paul
Don’t Miss: Parkinson’s Leaning To One Side