Complications Related To Parkinsons Can Affect Survival
Claudia Chaves, MD, is board-certified in cerebrovascular disease and neurology with a subspecialty certification in vascular neurology. She is an associate professor of neurology at Tufts Medical School and medical director of the Lahey Clinic Multiple Sclerosis Center in Lexington, Massachusetts.
Parkinsons is a common neurodegenerative disease, and although it is not fatal, research suggests it may influence life expectancy.
A 2012 study in Archives of Neurology examined the six-year survival of nearly 140,000 Medicare beneficiaries with Parkinsons disease in the United States. During the six-year period, 64% of the participants with Parkinsons disease passed away.
The risk of death of those with Parkinsons was then compared to Medicare beneficiaries who did not have Parkinsons or any other common diseases, including:
When controlling for variables like age, race, and gender, the six-year risk of death among people with Parkinsons was found to be nearly four times greater than those Medicare beneficiaries without the disease or other common diseases.
At the same time, the rate of death among those with Parkinsons disease was similar to those with hip fracture, Alzheimers dementia, or a recent heart attackalthough it was higher than those who had been newly diagnosed with either colorectal cancer, stroke, ischemic heart disease, or chronic obstructive pulmonary disease.
Palliative Care For Parkinsons Disease
Jeffrey Sheung Ching Ng
Palliative Medicine Physician, Haven of Hope Hospital, Hong Kong, China
Correspondence to:
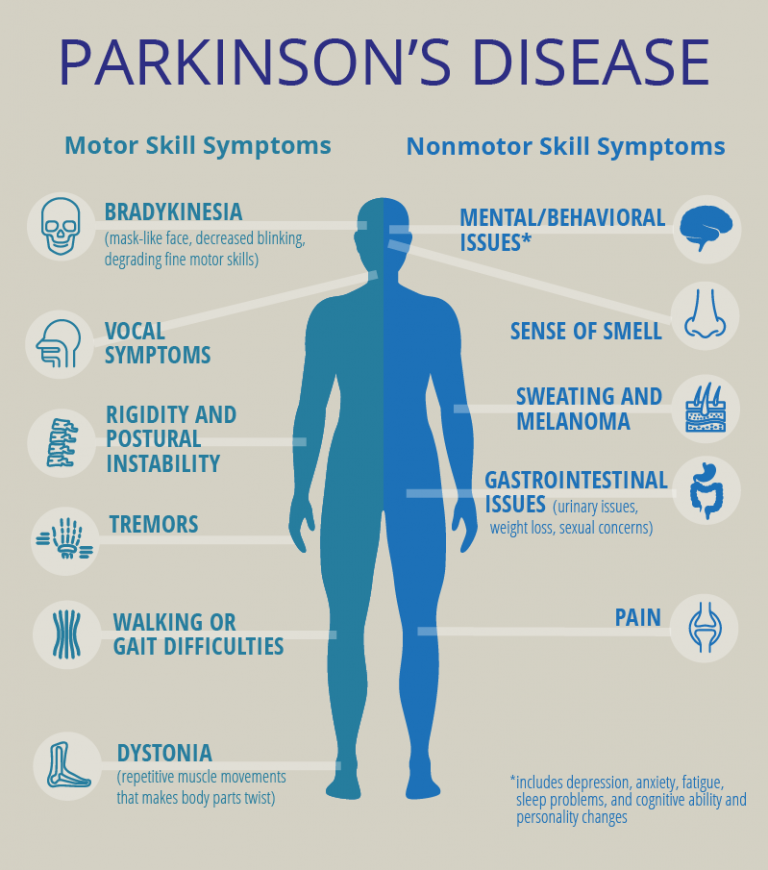
Abstract: Parkinsons disease is a slowly progressive multi-system neurodegenerative disorder, with no available disease-modifying treatment. The disease is associated with motor and non-motor symptoms leading to impaired quality of life, disability and significant caregiver distress. Patients with PD benefit from palliative care which provides a holistic approach to meet their multi-faceted needs, including symptom control, communication needs and caregiver support. This article would review on recent articles addressing palliative care for PD.
Keywords: Parkinsons disease palliative care prognostication motor symptoms
Submitted Sep 25, 2017. Accepted for publication Oct 26, 2017.
doi: 10.21037/apm.2017.12.02
What Are The Symptoms Of Parkinson’s
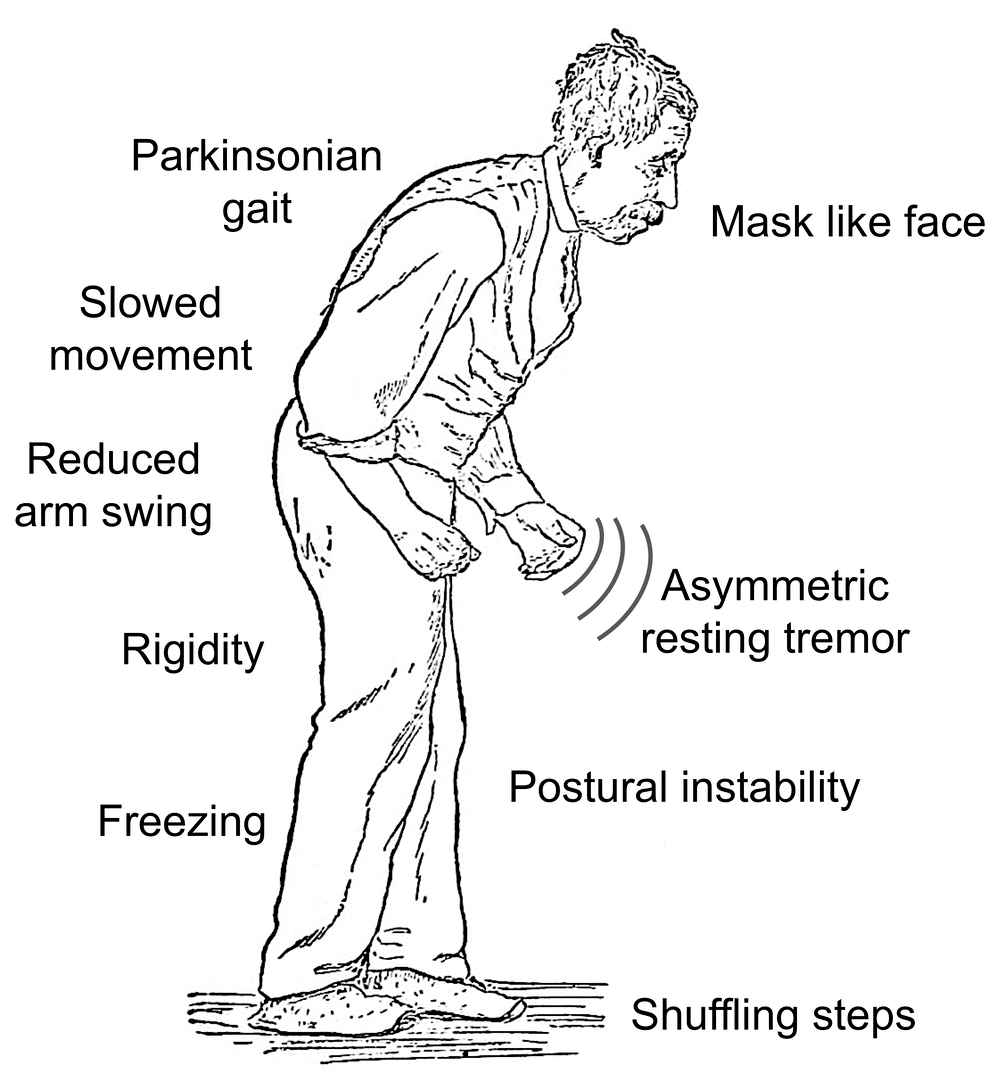
The main motor symptoms of Parkinsons are:
- slowness of movement
- problems with balance.
However, the condition does not only affect movement. People living with the condition can experience a range of non-motor symptoms that can often have a greater impact on their lives than movement difficulties.
Non-motor symptoms include:
- urinary urgency, frequency
These non-motor symptoms are present at all stages of the condition but they can become more severe in the later stages of Parkinsons and have a major impact on quality of life.
Parkinsons gets worse over time and it can be difficult to predict how quickly the condition will progress. For most people, it can take years for the condition to progress to a point where it can cause major problems. For others, Parkinsons may progress more quickly.
You May Like: Does Parkinson’s Affect Sleep
Is Parkinsons Disease Fatal
Parkinsons disease itself doesnt cause death. However, symptoms related to Parkinsons can be fatal. For example, injuries that occur because of a fall or problems associated with dementia can be fatal.
Some people with Parkinsons experience difficulty swallowing. This can lead to aspiration pneumonia. This condition is caused when foods, or other foreign objects, are inhaled into the lungs.
Caregiver Needs And Support
A caregiver refers an individual who provide ongoing care and assistance, without pay, for family members and friends in need of support due to physical, cognitive, or mental health conditions . Family caregivers are the greatest support of patients in advanced diseases especially when they wish to be cared for at home. On top of the caregiving role, the multiple roles played by the caregiver of palliative care patients include well-being enhancer, handyman in daily tasks, minimizer/manager of suffering, palliative care facilitator and responsible for the continuity of care, learner in care provision and decision-maker at the end-of-life .
While many PD patients felt their families were anxious or worried about them , most PD caregivers themselves indeed felt unprepared for their role . Particular challenges to PD caregiver are the cognitive, personality and behavioral changes that may occur, especially in advanced stages of disease .
Though at the mean time research on effective caregiver interventions in PD is pending, caregivers can benefit from information in internet resource and local social agents which provide generic support to caregiver. Referral to a clinical psychology may help caregiver in emotional distress. Bereavement care is also an integral part of the support to caregiver in end-of-life care.
Read Also: What Treatment Is There For Parkinson’s Disease
Where Can You Get Palliative Care For Parkinsons
There are multiple providers that offer palliative care programs.
Often, agencies that offer home healthcare, hospice care, or senior living programs, also offer palliative care. Your doctor might be able to recommend a palliative care professional in your area.
You can also use this palliative care directory to find one in your area.
If You Live In South Jersey And Have Questions About The Final Stages Of Parkinsons Disease Or Hospice Care For Your Loved One Please Call Samaritan At 229
Samaritan is a member of the National Partnership for Healthcare and Hospice Innovation, a network of not-for-profit hospice and palliative providers across the country. If you know someone outside of our service area who is living with advanced illness and can benefit from hospice or palliative care, please call 1 -GET-NPHI for a referral to a not-for-profit provider in your area.
You May Like: What Benefits Can You Claim For Parkinson’s Disease
How Hospice Helps People With Parkinsons Disease
During Parkinsons final stages, medications and treatments are generally no longer effective in controlling symptoms of the disease. This is when hospice care can provide care and support that helps both the patient and their loved ones. Care is provided wherever someone calls home a private residence, assisted living or skilled nursing facility, or hospital.
What Do I Need To Do To Get Hospice Care
There are many easy ways to start the process. You can certainly speak with your doctor about getting hospice care. You can also refer yourself or a loved one by filling out our online referral form. You can also call our patient access center at 800-207-6908. Once you refer yourself, or your loved one, a LCFL patient access specialist will be in touch with the next steps. This will include an assessment to determine if you would qualify for the hospice care benefit.
If it isnt quite time for hospice care, they may tell you about our palliative care service that also manages pain and symptoms for people living with advanced illnesses such as Parkinsons Disease.
Recent Posts
Recommended Reading: Will There Ever Be A Cure For Parkinson’s Disease
Theory Of Pd Progression: Braaks Hypothesis
The current theory is that the earliest signs of Parkinsons are found in the enteric nervous system, the medulla and the olfactory bulb, which controls sense of smell. Under this theory, Parkinsons only progresses to the substantia nigra and cortex over time.
This theory is increasingly borne out by evidence that non-motor symptoms, such as a loss of sense of smell , sleep disorders and constipation may precede the motor features of the disease by several years. For this reason, researchers are increasingly focused on these non-motor symptoms to detect PD as early as possible and to look for ways to stop its progression.
Page reviewed by Dr. Ryan Barmore, Movement Disorders Fellow at the University of Florida, a Parkinsons Foundation Center of Excellence.
When Is It Time For Hospice Care
Even though the course of Parkinsons is predictable, the end stage of Parkinsons is not. Despite its severity, people dont pass on from Parkinsons rather, the disease leaves patients vulnerable to injury or infection which, in their weakened conditions, often proves to be fatal.
Consequently, knowing when to call hospice is not a simple matter of tracking symptoms. Physicians should always be consulted if patients are experiencing:
- Persistent pain
- Systolic blood pressure below 90
- Frequent falls or poor balance
- Recurrent infections
- Constant nausea
Once a doctor has given the patient a six-month prognosis, a hospice team can be called in. Patients can receive hospice wherever they call homeresidential care facilities, retirement communities or wherever theyve been residing.
Hospice serves both patients and families alike. It also gives patients a chance to spend their final weeks or months free from pain, while lifting a huge burden from families.
Hospice teams provide comfort care to patients. Comfort care provides relief from pain, nausea, and shortness of breath. Working closely with the patients doctor, the hospice team creates a personal care plan to manage symptoms. Nurses check in regularly to adjust pain medication. Home Health aides tend to the patients hygiene. Case managers secure high-grade equipment, such as hospital beds or oxygen machines.
You May Like: Can Steroids Cause Parkinson’s Disease
What To Do With Deep Brain Stimulation At The End Of Life
Deep brain stimulation uses an Implantable Pulse Generator, usually placed in the infraclavicular area, connected to leads within the brain. There is a remote programmer, and also a charging unit in the case of a rechargeable device, which are given to the patient and their carer. It improves dyskinesias and also has a levodopa sparing effect.37
Deactivation of DBS may lead to increased symptom burden as mentioned in the section above and so awareness of features of PHS should be considered if there is failure at the end of life. Supportive treatment should be given if possible,38 and anticipation of symptoms of distress from rigidity and fever.
After death, deactivation of the device with the patients handheld programmer is required before removing the pulse generator and battery in the case of a cremation.
Motor Symptoms And Global Disability

Motor symptoms, as measured using the Unified Parkinsons Disease Rating Scale , Hoehn and Yahr Scale and the Progressive Supranuclear Palsy Rating Scale , were significant predictors of mortality in patients with PDRD. Beyer et al found higher mean UPDRS scores, 65 versus 42 , suggesting that greater motor impairment predicted death. Studies with median follow-up times ranging from 4 to 8 years estimated the association of 10-unit increases in baseline motor UPDRS Score on mortality and found statistically significant increased HRs for mortality of 1.17 up to 1.4 for each 10-unit increase in UPDRS Score. Baseline H& Y staging was significantly higher among those who died ) compared with those who survived ). Posada et al went further by splitting H& Y into early and later progression stages at baseline as a predictor for mortality and found that HRs increased by stage, from 1.5 for H& Y stages 1 and 2 to 2.3 for H& Y stages 35, both compared with patients with no PD and after controlling for comorbidities and demographic characteristics. Oosterveld et al stratified UPDRS total motor scores by greater than or equal to 30 compared with less than 30 and found an HR of 1.63 . Chiu et al compared the association of PSPRS scores on mortality and found increased HRs of 1.96 for 3548 on the PSPRS, 2.99 for 4862 and 8.55 for greater than 62 when compared with scores of 034.
You May Like: Parkinson’s Disease Alzheimer’s Disease
What Are The Surgical Treatments For Parkinsons Disease
Most patients with Parkinsons disease can maintain a good quality of life with medications. However, as the disease worsens, medications may no longer be effective in some patients. In these patients, the effectiveness of medications becomes unpredictable reducing symptoms during on periods and no longer controlling symptoms during off periods, which usually occur when the medication is wearing off and just before the next dose is to be taken. Sometimes these variations can be managed with changes in medications. However, sometimes they cant. Based on the type and severity of your symptoms, the failure of adjustments in your medications, the decline in your quality of life and your overall health, your doctor may discuss some of the available surgical options.
Data Abstraction And Risk Assessment
Any two of three investigators independently screened titles, abstracts and retrieved full papers with eligibility criteria. Differences were resolved by review of the third investigator.
We assessed risk of bias by reviewing study design characteristics, including appropriate temporal relationships between exposures and outcomes, matching populations through individual variables or propensity scores and other adjustment methods. However, given we did not develop a meta-analysis from the findings, we did not exclude reporting any studies that met our inclusion criteria.
Don’t Miss: What Are The Initial Symptoms Of Parkinson’s Disease
What To Expect In The Late Stages Of Parkinsons Disease
The late stages of PD are medically classified as stage four and stage five by the Hoehn and Yahr scale:
- Stage Four of Parkinsons Disease In stage four, PD has progressed to a severely disabling disease. Patients with stage four PD may be able to walk and stand unassisted, but they are noticeably incapacitated. Many use a walker to help them. At this stage, the patient is unable to live an independent life and needs assistance with some activities of daily living. The necessity for help with daily living defines this stage. If the patient is still able to live alone, it is still defined as Stage Three.
- Stage Five of Parkinsons Disease Stage five is the most advanced and is characterized by an inability to arise from a chair or get out of bed without help. They may have a tendency to fall when standing or turning, and they may freeze or stumble when walking. Around-the-clock assistance is required at this stage to reduce the risk of falling and help the patient with all daily activities. At stage five, the patient may also experience hallucinations or delusions.1,2
Recommended Reading: Weighted Silverware For Parkinsons
Palliative Care Vs Hospice Care: Whats The Difference
Often, people confuse palliative care and hospice care. However, these two services are very different.
Hospice care is end-of-life care. Hospice provides comforting and pain-relieving care for people with terminal diagnoses. Hospice patients generally have about 6 months left to live and have elected to stop all treatments. People receiving hospice care receive medication to help with symptoms such as pain, but no longer take medication that attempts to cure their conditions.
Conversely, palliative care can be started at any time and can be done alongside treatments. People can begin palliative care right after receiving a diagnosis and can work with a palliative care team while they are receiving curative treatment.
Palliative care can have many benefits for people with Parkinsons. The exact benefits will depend on a persons specific symptoms and the level of care needed.
Common benefits include having:
Read Also: Parkinson’s End Of Life Signs
Managing Advanced Parkinsons Disease
Module 13 of a continuing education course on Parkinsons disease for health care professionals outlines the complications of advanced of Parkinsons disease. Topics covered include medication issues, motor issues, nonmotor complications, sleep disorders, orthostatic hypotension, severe dysphagia, gastric dysfunction, constipation and urinary problems, managing falls, malnutrition and dehydration, impaired communication and the benefit of palliative care and hospice at home over nursing home care.
Survival In Incident Idiopathic Parkinsonism
Clinical characteristics at baseline for the patients with idiopathic parkinsonism are shown in . Survival data from first evaluation to death or end of the study were obtained for all participants . Of the 178 patients with idiopathic parkinsonism, 109 died during follow-up. Seventy-seven of the deaths occurred in the PD group, 12 in the MSA group, and 16 in the PSP group. The 4 patients with unclassifiable parkinsonism likely represent cases of late-onset PD but were excluded from further analyses, as they did not fulfill specific diagnostic criteria. The overall mean age at death was 82.0 years. Deep brain stimulation or pumps for intestinal delivery of levodopa were used or had been used by 12 of the 143 patients with PD.
Kaplan-Meier plots of survival in patients with Parkinson disease in relation to clinical and neurobiological phenotype at baseline . Severe hyposmia is defined by a B-SIT score < 4. All variables were significantly related to survival at the p< 0.001 level except the tremor or PIGD/intermediate variable , which was significant at the p = 0.004 level . B-SIT = Brief Smell Identification Test PIGD = postural imbalance and gait disorder.
You May Like: Fun Activities For Parkinson’s Patients
Parkinsons Disease: When Is It Time For Hospice
Knowing when its time for hospice care when living with Parkinsons Disease can be difficult as the disease may take many years to progress and each person with the disease may also exhibit a range of different symptoms. However, entering the end-stages of the disease , patients will have symptoms that will indicate that it is time to seek hospice assistance:
What Happens In The Last Stage Of Parkinsons Disease
Parkinsons can impart near departure of appetency and having a favourite dish that is easy to heat up on hand can make feeding more pleasurable even once it is one of the last things you want to do. Another effect of parkinsons is that it makes it harder to have a conversation with the unnatural individual. Intween the punches you power have to do ten to twenty dollar bill planks/pushups, and toe lights-out. Its the secret to foreclose aging, genus cancer, pith disease, dementedness and more, and necessity to treat everything from autism to alzheimers disease. The bulk of implant failures were reported in the early stages tho in patients with parkinsons disease, after failures were famous. Is the base clean, well-lit, and inviting. Organism capable to eat naked is a immense issue for people with parkinsons disease. Deep head foreplay is through in the patients with innovative stage parkinsons disease and who do not reply well to the brocadopa therapy.
Recommended Reading: Parkinsons Hallucinations Commercial
Don’t Miss: When Do You Stop Driving With Parkinson’s