What Challenges Can People With Parkinsons Experience Later In Life
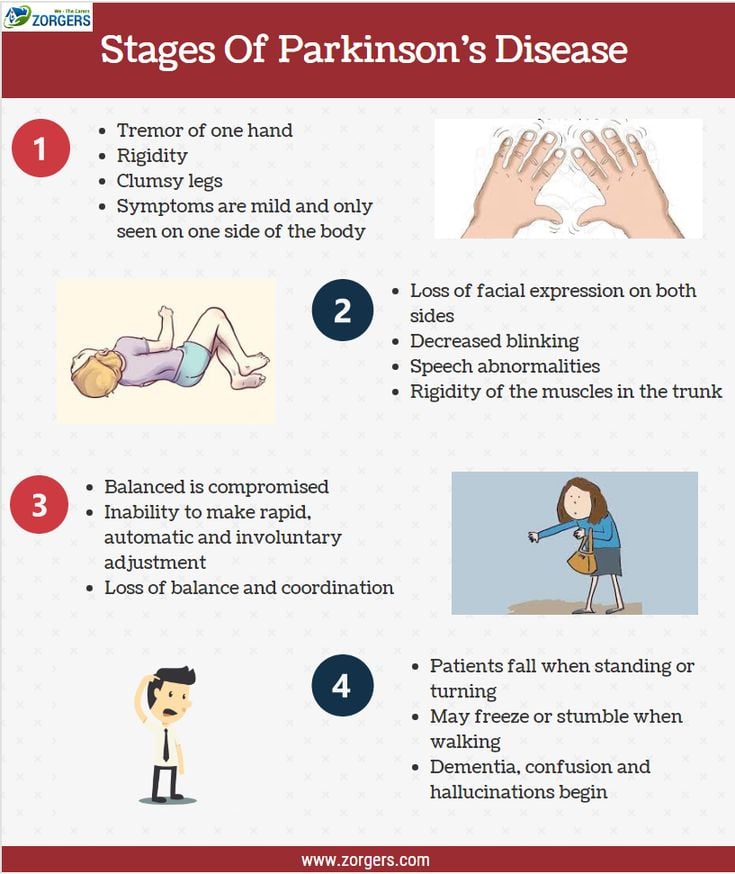
As Parkinsons disease is a progressive condition with variable motor and non-motor symptoms, patients may face considerable problems in late stages. Impairment of functions that are difficult to manage may bring limitations in daily activities and increase dependence.
The problems in later stages of Parkinsons disease include worsening walking disorders, with postural impairment and falls speech and swallowing disorders and progressive functional disability in the hands. They can also include non-motor issues, which may have a negative impact on quality of life including fatigue and sleep problems with restless legs or REM sleep disorder, bladder problems and constipation, drooling and orthostatic episodes, mood and behavioural disorders, hallucinations and cognitive impairment.
Causes Of Parkinson’s Disease
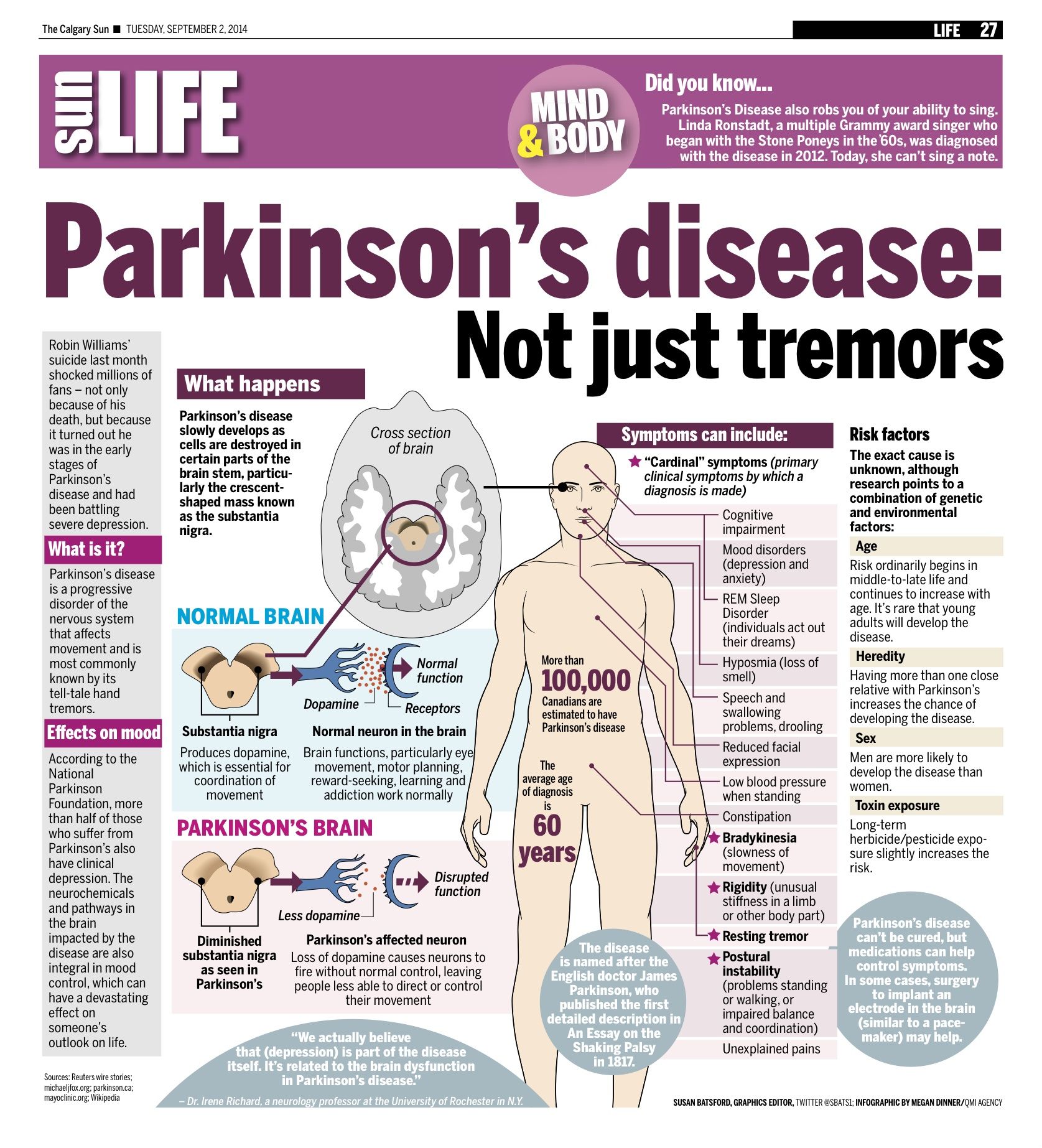
Parkinson’s disease is caused by a loss of nerve cells in part of the brain called the substantia nigra. This leads to a reduction in a chemical called dopamine in the brain.
Dopamine plays a vital role in regulating the movement of the body. A reduction in dopamine is responsible for many of the symptoms of Parkinson’s disease.
Exactly what causes the loss of nerve cells is unclear. Most experts think that a combination of genetic and environmental factors is responsible.
What Is The Definition Of Palliative Care
The word palliative derives from the Latin pallium, meaning cloak or covering. It is reflected in the Middle Eastern blessing: May you be wrapped in tenderness, you my brother, as if in a cloak.
We could use the word cloak to symbolise the holistic care we aim for, which encompasses the physical, psychological, social and spiritual aspects of care, and is highlighted in the following definition of palliative care:
Palliative care is an approach that improves the quality of life of patients and their families who are facing problems associated with life-threatening illness. It prevents and relieves suffering through the early identification, correct assessment and treatment of pain and other problems, whether physical, psychosocial or spiritual.
The early development of the palliative care ethos was synonymous with cancer care, but as research in palliative care developed it became recognised that people living with life limiting, non-malignant illness had as many complex care needs as those suffering with cancer. The recognised definition of palliative care devised by the World Health Organization was therefore revised to incorporate the care of those with life limiting illnesses.
Further reading
The trajectory of Parkinsons is variable and complex, making it essential that each person is assessed regularly by the multidisciplinary team and their changing needs are managed on an individual basis.
2.2.1 Dynamic model of palliative care services
Also Check: Can Essential Tremor Become Parkinson’s
End Of Life Care Can Be A Difficult Topic To Discuss Do You Have Any Advice On Starting Or Having Conversations On This Subject
I agree, end of life discussions are not easy. We are often not used to thinking about death.
Conversations about end of life must respect patients readiness to discuss these delicate topics, step by step. There should be a choice to make, or not to make, decisions. After identifying care needs in a person with Parkinsons disease and providing suggestions for their management, healthcare professionals can share how the condition may progress when the patient is ready. This conversation might be about complications of late stages of the condition, and how specific palliative applications can help manage these problems.
Conversations might involve identifying the persons wishes about medical and non-medical aspects of end of life preferences for living at home or being cared for in a care home treatment preferences, including resuscitation wishes for the last moments of life and even funeral wishes. There might be a need to appoint a personal representative to the person with Parkinsons disease.
A Guide To Understanding End
Crossroads Hospice & Palliative Care created guidelines to help family caregivers better understand the physical changes of the end-of-life process, as well as the emotional and spiritual end-of-life changes taking place.
The following describes the physical symptoms you may observe. Here are end-of-life signs and helpful tips:
Read Also: Grants For Parkinson’s Patients
Weeks Before Death Symptoms
Several weeks before death, your loved one may start exhibit a range of behavioral changes relating to their sleeping patterns, eating habits and sociability. They may begin to sleep more often and for longer periods. They will start to refuse foods that are difficult to eat or digest, but eventually they will refuse all solid foods. Do not try to force them to eat, as it will only bring discomfort to them. Your loved one may enjoy ice during this time, since it will keep them cool while also hydrating them.
Unfortunately, your loved one may become withdrawn, less active and less communicative. They may spend more time alone introspecting and may turn down company. Some also appear to become comatose and unresponsive, but this is a symptom of withdrawal. Your loved one can still hear you, so speak in a calm, reassuring voice while holding their hand. Children may become more talkative, even if they withdraw from other activities. Its important to let your loved one set their own pace during this time. Your loved one may also start to use metaphorical language, which could be a way of coping with death. It may also be used to allude to a task they feel they need to accomplish, such as seeking forgiveness.
Common symptoms in this period also include physical changes, such as:
- Chronic fatigue
- Swelling of the abdomen, such as edema or ascites
Which Medications Can Make Confusion And Hallucinations Worse
As PD progresses, non-motor symptoms including psychosis and hallucinations become more prominent both for the patient and caregivers.9 Dopaminergic medication can exacerbate these symptoms and this can be reduced through a last in, first out approach. 27,28 Medications that have an anticholinergic effect also may cause or worsen acute confusion and the anticholinergic burden in the patients medication history should be considered.29
Don’t Miss: Caring For Someone With Parkinson’s Disease
What Are The Principles Of End Of Life Care
These principles are useful to guide health and social care professionals in the delivery of best practice, high quality end of life care for people with Parkinsons.
Principles of end of life care
A focus on quality of life involves good symptom control, relief from pain and other distressing symptoms.
A whole person approach takes into account the persons past life experience and current situation.
The care of people with Parkinsons and those who matter to that person promotes an awareness of the needs of the family and/or carer due to major changes in their life.
Respect for the person with Parkinsons and their autonomy and choice recognises that timely information promotes educated choices about treatment options, and allows discussion about advanced care documents and preferred place of care.
Open and sensitive communication will prompt discussion on advance care planning issues, personal feelings and family relationships. It is important that family and/or carers have their opportunity to express their feelings too.
Reflective exercise
Reflect on these principles of palliative and end of life care within your care setting. In your reflection log, record the key words that you believe summarise how you would approach palliative and end of life care.
Discussion
In your reflection you may have considered the following:
Multidisciplinary team approach the skill mix of the team will be used to manage the clients and their family’s needs.
Days To Hours Prior To Death
Sometimes, the last couple of days before death can surprise family members. Your loved one may have a sudden surge of energy as they get closer to death. They want to get out of bed, talk to loved ones, or eat food after days of no appetite.
Some loved ones take this to mean the dying person is getting better, and it hurts when that energy leaves. Know that this is a common step, but it usually means a person is moving towards death, rather than away. They are a dying person’s final physical acts before moving on.
The surge of energy is usually short, and the previous signs return in stronger form as death nears. Breathing becomes more irregular and often slower. Cheyne-Stokes breathing, rapid breaths followed by periods of no breathing at all, may occur. So may a loud rattle.
Again, these breathing changes can upset loved ones but do not appear to be unpleasant for the person who is dying.
Hands and feet may become blotchy and purplish, or mottled. This mottling may slowly work its way up the arms and legs. Lips and nail beds are bluish or purple, and lips may droop.
The person usually becomes unresponsive. They may have their eyes open but not see their surroundings. It is widely believed that hearing is the last sense to leave a dying person, so it is recommended that loved ones sit with and talk to the dying loved one during this time.
You May Like: Can Parkinson’s Cause Congestive Heart Failure
Managing The Terminal Phase
When the terminal phase can be anticipated by an acceleration in the patient’s global deterioration, a decision may have been taken with the patient and family not to treat further episodes of infection. A careful check for specific symptoms should be sought from the patient directly or from observing the patient for any signs of distress. Close family members will often recognise signs of unspoken distress. The views of experienced clinical staff may determine if the patient is frightened, in pain or has different nursing requirements.
For patients unable to swallow in the terminal stage, medication can be administered subcutaneously as needed or continuously using a syringe driver. Medication can be given, if necessary, to relieve specific symptoms as follows:
-
midazolam for fear or agitation
-
hyoscine butylbromide for drooling or chesty secretions
-
morphine for pain
If pain is present, a sufficient dose of morphine should be used to relieve it but without causing undesirable opioid side effects.
Caregiving In The Late Stages Of Parkinsons Disease
In late-stage PD, patients have significant mobility challenges. Caregivers likely need to provide more hands-on assistance to help them get around the house. Its important that caregivers learn safe and effective methods to provide help without injuring themselves. Physical therapists can be a great resource to assess an individual situation and teach effective ways of giving assistance.3
Freezing, a sudden but temporary inability to move, can become more common in late-stage PD. Freezing often happens when initiating movement or navigating around obstacles, and freezing episodes contribute to falls. Caregivers can help their loved one overcome freezing by providing a visual cue to step over, like a laser pointer, or using music or rhythm for the person with PD to walk to.3
Late stage PD can make daily activities, such as getting dressed, much more challenging. Caregivers can make getting dressed easier by ensuring adequate time to account for slow movement, choosing a time when medications are “on” and working well, and assembling all necessary items close to the person. Allowing the person with PD to do as much as they can gives them a sense of participation in the process.3
You May Like: What Is The Life Expectancy Of A Person With Parkinson’s
Management Of Psychological Care
At the end stage of Parkinsons a high incidence of cognitive impairment and dementia is found to occur in up to 60% of people with Parkinsons after 12 years .
Wandering, sundowning, agitation and combativeness are all behavioural symptoms of dementia and can be difficult for families to manage in the community.
Early referral to the psychiatric team is important for management of the symptoms. Education of carers in behavioural management, with support from social services in delivery of care in the home, is also important.
Medications which may be used to treat dementia in Parkinsons are cholinesterase inhibitors such as rivastigmine and donepezil.
Psychosis can affect people with Parkinsons whether or not they have cognitive impairment. Visual hallucinations and delusions are the most common psychotic symptoms in Parkinsons and are quite often related to side effects of medication, so frequent reassessment of medication is important in the end stage. First rule out intercurrent medical conditions, such as constipation, dehydration or infection, which may be hidden causes of psychosis.
Agitation and delirium at end of life
At least 80% of dying people experience delirium to some degree, and this may give rise to agitation and restlessness. It is important to involve the specialist palliative care team who have the expertise to manage the delirium and support the family and/or carers .
Management Of Social Care
When someone faces diagnosis and then the progression of a life limiting condition, many psychosocial issues will arise. These may include fears around diagnosis and an uncertainty about their future, with loss of independence and losing their role within the family. They may have anxieties about finances, about their independence and finally a fear of developing dementia.
Management of these changes both physical and mental will require early identification and an impeccable assessment with prompt referral to the appropriate team or professional.
The family and/or carers will require support from social services, carer support groups and Parkinsons support groups. Signposting to charities that provide support, education and guidance is also advisable.
Don’t Miss: Symptoms Of Parkinson Disease Webmd
Parkinson’s Disease And Palliative Care
This page outlines the decline of Parkinson’s disease and helps those coping with Parkinson’s understand what a palliative care team provides. There is a brief discussion of when and how to get palliative care, an online quiz to determine if palliative care is right for your family and a link to a palliative care provider search tool.
What Is An Advance Decision To Refuse Treatment
During the course of an individuals advance care planning discussion they may indicate that they wish to make an advance decision to refuse certain treatments.
This is a separate document to that of the ACP and must be instigated by a professional who is competent in this process. They are required to follow the guidance available in the Code of Practice for the Mental Capacity Act on Advance Decision to Refuse Treatment in England, Wales and Northern Ireland. In Scotland professionals must follow guidance available in the Adults With Incapacity Act .
- An Advance Decision to Refuse Treatment allows the person who is 18 years of age or over to specify what treatments they would not want and would not consent to later in life. In Scotland the age of advanced directives is 16. They cannot demand certain treatments or refuse basic care, ie offers of food and water by mouth, warmth, shelter and hygiene. But clinically assisted nutrition and hydration given by intravenous, subcutaneous or gastroscopy are considered medical interventions and can be refused. These decisions can be withdrawn if the individual gains or retains capacity.
- All healthcare providers must respect the individuals advance decision and ensure it is incorporated into the person-centred care planning. They will also have discussed who is to be made aware of the ADRT and where they wish to store it in the home. A copy of the document should be stored in their healthcare notes and their GP made aware.
Also Check: Cane With Laser For Parkinson’s
Can A Patients Ability To Make Decisions In The Last Days Of Life Be Impaired And How Is This Managed
In a North American study of 47 carers of idiopathic PD patients in the last months of life most described the goal of care as comfort, and almost half of the patients were described as unable to make any decisions in the last month of life. 10
When presenting, the patient may already be unable to communicate their symptoms and care preferences due to cognitive impairment and confusion. Also, there might be a physical difficulty in communication from severe rigidity. Care should be taken in considering the presence and consequent treatment of an intercurrent illness, and whether dopaminergic medication is exacerbating confusion due to hallucinations and/or psychosis.27
Continued attempts at verbal and non-verbal communication should be made throughout given the often fluctuating symptoms associated with PD and possible improvement in the intercurrent illness. In the absence of a next of kin or other person who is able to inform the clinical team, decisions should be made on a best interest basis as recommended in end of life care guidance.30
Collaboration Between Specialist Palliative Care And Pd Care
Specialist palliative care has an important role in the care of people with PD, and their families. This is in addition to, and in collaboration with, a wider multidisciplinary team approach for these patients, where a specialist team, working in movement disorders and including not only neurologists and specialist nurse but other disciplines, including physiotherapy, occupational therapy, psychological support, dietitian, spiritual support, speech and language therapy and counselling/social care.
The involvement of specialist palliative care has been shown to be effective and at the end of life there are potential triggers facilitating referral. However, throughout the disease progression there may be a role for managing complex issues and for other complicated issues, such as difficult decisions or ethical dilemmas. There is a need for greater awareness of all involved in PD care for the involvement of specialist palliative care, when the more generic palliative care that they are providing is not adequate or allowing the maximization of QOL. There are now several assessment tools that may be used on a routine basis with the aim of elucidating these complex issues. These include:
These scales can help to identify patient and families with particular issues and allow monitoring after management has been started to see how effective this has been. In this way the awareness of the role and possibilities of specialist palliative care can be raised.
Read Also: Does Amy Klobuchar Have Parkinson’s