Rem Sleep Behavior Disorder
In vivid dreaming states most peoples bodies are still. However people with RBD lack muscle paralysis resulting in their acting out their dreams. This can include talking, screaming, shouting, hitting, punching or kicking, even propelling them out of bed. This can be scary and dangerous if they strike their partners or other bedside objects involuntarily. RBD is common in and can begin long before the onset of declining motor function. Fortunately it is also a very treatable condition.
Medications And Supplements Used To Treat Tardive Dyskinesia
A number of medications and supplements have been identified that ameliorate TD symptoms.
Cholingergic Agents.
Cholinergic agents are used as muscle stimulants to diagnose myasthenia gravis and to treat glaucoma. These agents can also improve the Parkinsonian features of TD. Donepezil, a reversible acetylcholinesterase inhibitor, is currently the only cholinergic medication that has shown benefit against TD. Overall, however, cholinergic agents are not a widely accepted treatment for TD as sufficient evidence is lacking to suggest they are more helpful than other treatments.
Clozapine, Quetiapine, Olanzapine, and Apomorphine.
Clozapine, a serotonin and dopamine receptor antagonist, is an atypical APD used to treat schizophrenia. Clozapine is the best current medication recommended for patients who require antipsychotics and simultaneously have TD, as clozapine has been reported to reverse TD symptoms., Clozapine has been linked to TD however, the incidence is much lower compared to other atypical APDs. Drugs with similar mechanisms of action such as quetiapine, a weak striatal dopamine antagonist, and olanzapine, a dopamine and serotonin receptor antagonist, have also been shown to be effective in ameliorating TD symptoms. Apomorphine, a dopamine receptor antagonist, can be given in conjunction with L-DOPA to decrease dyskinesias.
Tetrabenazine Analogs.
Clonazepam.
Propranolol.
Amantadine.
Branched-Chain Amino Acids.
Ginkgo Biloba.
Antioxidant Medications and Supplements.
Dystonia Vs Dyskinesia In Parkinson’s Disease
Claudia Chaves, MD, is board-certified in cerebrovascular disease and neurology with a subspecialty certification in vascular neurology. She is an associate professor of neurology at Tufts Medical School and medical director of the Lahey Clinic Multiple Sclerosis Center in Lexington, Massachusetts.
Dystonia and dyskinesia are movement problems that commonly occur in Parkinsons disease . You may experience one or both of them, particularly in late-stage PD. Dystonia is muscle stiffening caused by PD, while dyskinesia is a type of muscle twisting caused by some PD medications.
Dystonia and dyskinesia can both cause distress, and they are distinguished from each other based on their visible features. They can be managed with medication or surgery, typically with a moderate improvement of symptoms.
PD is characterized by four primary symptoms:
- Resting tremor
- Postural instability
- Rigidity
While they can fluctuate in severity, the primary symptoms of PD tend to be present most of the time.
Dystonia and dyskinesia are recurrent, abrupt, and short-lived muscle movements. Not everyone who has PD experiences dystonia and dyskinesia. If they do, the symptoms they experience can be telling.
For example, dystonia can cause your toes to curl, making it difficult to walk. Or it may manifest primarily in your neck muscles, causing your head to turn painfully to one side.
Recommended Reading: Nutritional Support For Parkinson’s Disease
Other Causes Of Dyskinesia And Dystonia
There are many types of dystonia unrelated to Parkinsons disease. Many forms of dystonia occur with no known cause. Some causes of dystonia are hereditary, while brain injury can also cause dystonia.
Huntingtons disease is a rare, genetic condition in which nerve cells in the brain degenerate over time. This disease causes movement disorders similar to Parkinsons, including chorea and dystonia.
Multiple system atrophy and progressive supranuclear palsy are other rare, degenerative disorders that affect muscle movements. Dyskinesia can occur when people with MSA or PSP are treated with levodopa, and untreated MSA or PSP can lead to the development of dystonia.
What Causes Dyskinesia In Parkinson’s Disease
Unlike “off” time, patients typically experience dyskinesia in Parkinson’s when medications are working and other symptoms are under control. Researchers aren’t exactly sure what causes dyskinesia, but it is believed to be a side effect of long-term levodopa use, not a symptom itself. Levodopa-induced dyskinesia can look like fidgeting, writhing, wriggling, head bobbing, or body swaying. LID can sometimes be confused with Parkinson’s tremor, which is a back and forth shaking caused by the disease.
Because levodopa is taken throughout the day, dopamine levels in the brain rise and fall. These fluctuating levels of dopamine combined with the continued loss of dopamine in the brain make it difficult to maintain regular dopamine levels, and lead to dyskinesia.
Individuals diagnosed with Parkinson’s at a younger age are more likely to experience dyskinesia. It’s also more common in later stages of Parkinson’s or in those who have taken levodopa for several years.
Read Also: What Can Mimic Parkinson’s Disease
Dyskinesia And Wearing Off
If youve been taking a Parkinsons drug that contains levodopa for example, co-beneldopa or co-careldopa for some time, you may develop motor fluctuations, wearing off and dyskinesia. These are side effects that can affect your movement.
Dyskinesia is muscle movements that people with Parkinsons cant control. They can include twitches, jerks, twisting or writhing movements. Dyskinesia can affect various parts of the body such as the arms, legs and torso.
There are different types of movements, and when and how often they appear can be different for each person with Parkinsons. Some people can have dyskinesia for most of the day. Others may only experience it after taking their medication or just before the next dose is due.
People with Parkinsons can also experience this side effect when levodopa is at its highest level in the bloodstream , and the dopamine levels in their brains are at their highest. Dopamine is a chemical messenger made in the brain. The symptoms of Parkinson’s appear when dopamine levels become too low.
Because dyskinesia causes people to move around so much it can sometimes cause weight loss. If youre worried about this, speak to your GP, specialist or Parkinsons nurse. They can refer you to a dietitian, who will be able to help you maintain a healthy weight.
If you go from having good control of your movement symptoms to having less control, its called a motor fluctuation. This change can happen slowly or quickly.
How Levodopa Can Impact Uncontrolled Movements In Parkinsons Disease
Carbidopa-levodopa is a drug combination that works to reduce symptoms in Parkinson’s disease for as long as a patient takes it. Levodopa converts into dopamine in the brain, helping to control movement, while carbidopa prevents the breakdown of levodopa in the bloodstream so more levodopa can enter the brain.
In Parkinson’s, dopamine-producing brain cells are lost and dopamine levels decrease, leading to disease symptoms. Levodopa effectively treats motor symptoms, such as tremors, stiffness, and slowness of movement by crossåing into the brain through what is referred to as the blood/brain barrier. It is combined in medications with carbidopa, which slows the breakdown of levodopa in the bloodstream so more medication can reach the brain. Carbidopa can also reduce nausea and vomiting, common levodopa side effects.
While effective at managing some symptoms, it does not slow or stop disease progression or treat non-motor symptoms like sleep issues and depression.
As the underlying disease progresses and symptoms get worse, patients may need to increase their dose or take levodopa more frequently to experience the same reduction in symptoms. Patients may experience what is referred to as “off” time when the medication wears off before it’s time for another levodopa dose. “Off” time can lead to motor fluctuations as well as the return of other symptoms.
Don’t Miss: How Do You Stop Parkinson’s Tremors
Prevalence And Risk Of Td
The mean prevalence of TD in people treated with APs was 2025% according to meta-analyses of articles published between 1959 and 2015.27,28 A 20-year longitudinal study initiated prior to the widespread use of second-generation APs calculated a yearly cumulative incidence of TD of 4%5%.27 The frequent occurrence of TD and acute extrapyramidal symptoms, such as drug-induced parkinsonism and acute dystonia, encouraged the development of second-generation APs, which were intended to minimize the incidence of adverse neurological effects. Although acute drug-induced parkinsonism and acute dystonia are lessened, TD has not been eliminated. The annual prevalence of TD among patients receiving APs was estimated to be 7.6 to 9.7 per 1000 people according to a large retrospective observational study of electronic health records, with nearly 80% of study participants using second-generation APs.15 A direct comparison of annualized incidence between first- and second-generation APs indicates a reduced but not eliminated risk of TD with use of second-generation APs .6,29
The most important risk factors for the development of TD include older age and cumulative exposure to the DRBA. Other risk factors include the dopamine-receptor binding affinity of the DRBA in question, female sex, mood disorders, dementia, and prior drug-induced parkinsonism.4, Smoking and substance abuse may also be associated with a higher risk of developing TD.33
Ataxia / Dysmetria / Asynergia
Ataxia is an unsteady and swaying walk, often with feet planted widely apart. People have difficulty walking a straight line with their heel touching the toe of the shoe in front . Ataxia can occur in a number of neurologic conditions.
Dysmetria is misjudging the distance to a target. A person with dysmetria will have problems reaching out and accurately touching a targeted object.
Asynergia is a breakdown of movement, so that movements of the arms and legs become irregular and clumsy.
For more information, visit the National Ataxia Foundation website at www.ataxia.org.
Read Also: Is Drooling A Sign Of Parkinson’s
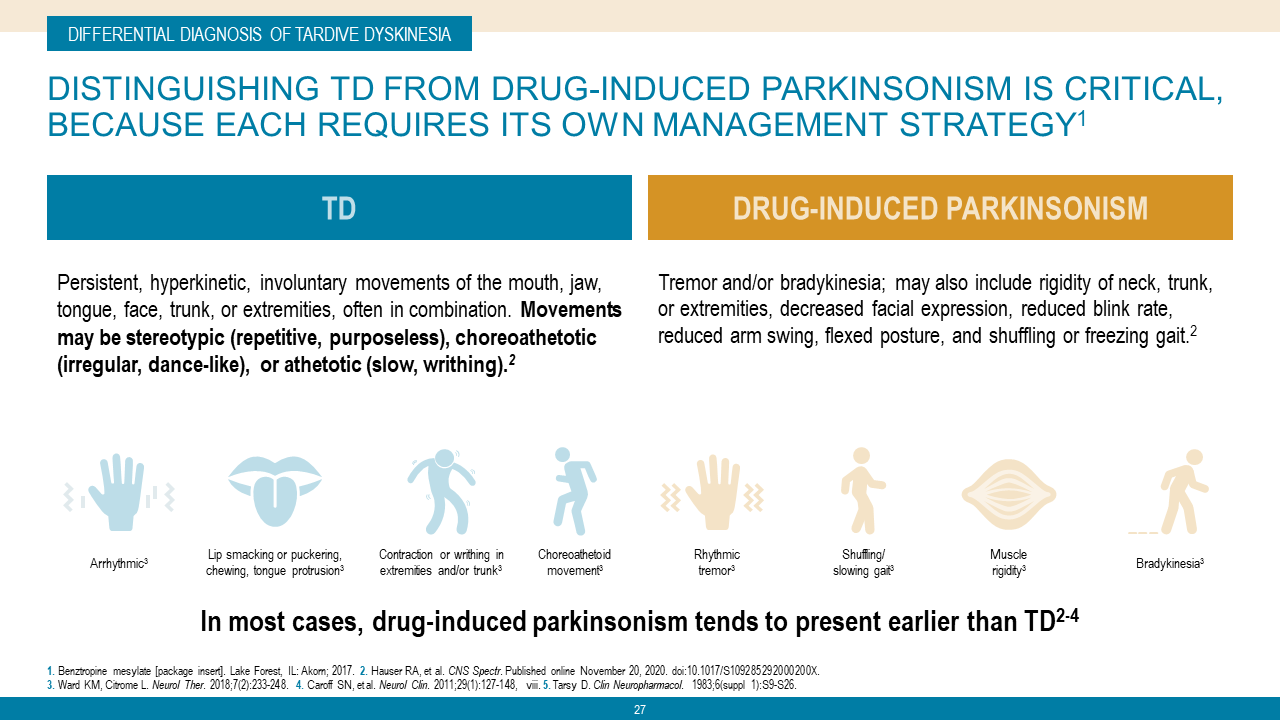
Measuring Tardive Dyskinesia Against Drug Induced Parkinsonism
The symptoms of tardive dyskinesia and drug-induced parkinsonism can be remarkably similar, but an accurate diagnosis is critical when treatment for one condition may worsen the other.
Kristen M. Ward, PharmD
An accurate diagnosis for patients with either drug-induced parkinsonism or tardive dyskinesia is imperative and can minimize the impact of the symptoms on the patients quality of life, according to a new review of movement related disorders.
Researcher duo Kristen M. Ward, PharmD, and Leslie Citrome, MD, MPH, conducted a literature review of articles published as of the spring of 2018 that related to the presentation, pathophysiology, epidemiology, and management of DIP and TD. The pair found that there was sparse primary literature that supported the use of most medications for treatment of DIP and TD, except for valbenazine and deutetrabenazine.
The study authors wrote that while both DIP and TD are stigmatizing movement disorders associated with exposure to dopamine receptor blocking agents such as antipsychotics they differ in their pathophysiology and clinical management.
The differences in treatment are immensely important, they said, because treatment for one may worsen the other. The treatments are different for DIP and TD and rely on accurate diagnoses.
Leslie Citrome, MD, MPH
The study authors noted that it is possible for patients to have both DIP and TD DIP usually precedes TD. This is not currently understood clearly.
Impact Of Td In Older People
The impact of TD on an individuals physical, mental, and economic health may intensify with age.3,22 The social and emotional effects of symptoms are highly debilitating for people with TD of all ages, but feelings of isolation and depression may be especially profound for older people.3,16 Older individuals are also uniquely vulnerable to the physical consequences of TD, such as impaired gait and balance, which can lead to falls.16,26 TD in older patients often presents as oro-bucco-lingual dyskinesia, and these movements can interfere with eating and swallowing incidents of choking resulting from respiratory TD have been reported.7,19,46 Further, oro-bucco-lingual TD can cause loosening of natural and artificial teeth and be augmented by edentulousness and denture use edentulousness itself can cause abnormal movements of the mouth in the absence of neurological disorders such as TD.26,46,47 Older patients may also be affected by dyskinesias of the limbs, trunk, and respiratory system, with symptoms such as grunting.7,26,48
Don’t Miss: Deep Brain Stimulation For Parkinson’s Disease Before And After
Mechanism Of Adverse Medication Reactions
The exact mechanisms of adverse medication reactions that cause TD are not well defined. However, the blockade of dopamine receptors by dopamine antagonists is the most widely accepted theory. Chronic dopamine blockade caused by dopamine D2 receptor antagonists or APDs could result in an upregulation of dopamine receptor responsiveness, resulting in a compensatory supersensitivity of the receptors, especially in the basal ganglia. However, some studies suggest that D3, D4, and D5 receptors are also involved in the pathogenesis of TD., D3 and D5 receptors have a consistent positive correlation with TD, but evaluations of D4 yield inconsistent results.,
Anticholinergic agents are also linked to TD, and taken together with the dopamine receptor supersensitivity hypothesis, an imbalance of dopamine and acetylcholine is likely involved in TD pathogenesis. Evidence also suggests an imbalance of serotonin. Selective serotonin reuptake inhibitors such as fluoxetine inhibit dopamine neurons in the nigrostriatal pathway by increasing serotonin in the raphe nucleus. SSRIs act by potentiating the inhibitory effects of serotonin on dopamine production in the basal ganglia. This decrease in dopamine production by serotonin could contribute to the pathogenesis of TD.
Akinesia / Bradykinesia / Hypokinesia
Akinesia means absence of movement. Bradykinesia means slowness of movement. Hypokinesia means decreased amplitude or range of movement. These three terms are commonly grouped together and referred to as bradykinesia. Bradykinesia is a prominent feature of parkinsonism and is mild in early disease stages but becomes more severe in advanced stages of parkinsonism.
Also Check: Parkinson’s Dry Mouth Treatment
How Is It Treated
When dyskinesia is a direct result of taking levodopa, the treatment differs from person to person. Some treatment options may include:
- adjusting the dose of your levodopa to avoid large fluctuations in the amount of dopamine in your system
- taking levodopa in a continuous infusion or an extended release formulation
- taking amantadine extended release , which has been approved to treat dyskinesia
- taking levodopa in smaller doses more often
- taking Duodopa, a medication that helps stabilize the amount of dopamine in the blood, which may help with smoother motor functions
- undergoing deep brain stimulation, which is a surgical treatment for severe symptoms. Certain criteria must be met for this to be an effective treatment. Ask your doctor if this is an option for you. Deep brain stimulation is only done after other treatments have not worked.
As with any treatment, be sure to discuss all side effects with your doctor before deciding on the best treatment for you.
Paroxysmal Dyskinesias And Exercise
Interestingly, in contrast to LID, only physical activities such as domestic activities in patients with PED can activate dyskinesias, a rarer and less well-documented group. Many studies of genetic studies have been carried out to understand the pathophysiology of the attacks. In summary, the attacks are triggered by prolonged exercise like walking or running characterized by attacks of dystonia and chorea, typically lasting for 5-30 min1414. Meneret A, Roze E. Paroxysmal movement disorders: An update. Rev Neurol. . 2016 :433-45.. The attacks often start in the body part involved in the activity and last for 10-15 min after stopping the exercise. PED made walking impossible and caused falls in some of the patients. Some patients were able to stand despite the PED, or walk with difficulty, but most patients had to sit down until the movements subsided. A summary of the studies is shown in Table 3.
Recommended Reading: Nursing Care For Parkinson’s Disease
Distinction From Similar Conditions
Unlike TD, Sydenham chorea is a disorder associated with a history of group A streptococcal infection and rheumatic fever in children. It typically affects children and adolescents 6 months or more after an infection with group A streptococci. Prompt administration of antibiotic therapy for infections with group A streptococci dramatically reduces the incidence of Sydenham chorea. The female-to-male ratio is approximately 2:1.
Sydenham chorea is characterized by the rapid onset of chorea, muscular weakness, hypotonia, dysarthria, obsessions, compulsions, and other behavioral and emotional disturbances. After an abrupt or insidious onset, Sydenham chorea worsens over 2-4 weeks and then resolves over 36 months. Chorea may persist after the episode has ended. One fifth of patients with Sydenham chorea experience a recurrence, typically within 2 years of the initial episode.
Pantothenate kinase-associated neurodegeneration occurs in patients aged 1015 years, a different age group than that of persons with TD. PKAN is an extremely rare, progressive neurogenetic disorder with autosomal recessive inheritance associated with dementia and death . It is characterized by rigidity, dystonia, choreoathetosis, spasticity, foot deformity, and intellectual deterioration. It is associated with excessive iron deposition in the basal ganglia that can be observed on MRI.
Current Therapeutic Strategies For Td In Older Patients
The first step in developing the optimal treatment strategy for TD is timely diagnosis, which requires the clinician to be routinely vigilant.67 Diagnosis is based on history of exposure to DRBAs, and a minimum duration of only 1 month of AP exposure is required to diagnose TD in individuals aged 60 years, compared with 3 months in younger adults.2,7,60
An early strategy to mitigate TD symptoms involves modification of the existing AP medication regimen if clinically feasible.68 However, success with this approach is often limited.23,68,69 Two vesicular monoamine transporter 2 inhibitors, valbenazine and deutetrabenazine, have been approved by the US FDA to treat TD.68,70,71 Recent guidelines for the treatment of schizophrenia recommend VMAT2 inhibitors as first-line therapy for patients who have moderate to severe or disabling TD or for patients with mild TD on the basis of such factors as patient preference, associated impairment, or effect on psychosocial functioning.72 In two recent studies of subjects aged 55 years who had participated in clinical trials conducted by the manufacturer, Sajatovic et al demonstrated that valbenazine and deutetrabenazine (mean age: 63.1 years, range: 5581 years are well tolerated in older individuals.73,74 Of note, VMAT2 inhibition manages the symptoms of TD but does not cure them dyskinetic movements generally return when the VMAT2 inhibitor is discontinued.75
Don’t Miss: Fda Approved Parkinson’s Drugs