Parkinson’s And Cognitive Impairment
Our findings indicate in a stratified, random sample of 1,152 Mexican-American and NHW elderly residents of El Paso County, Texas, that PD is significantly associated with CImp on three disparate measures of this phenomenon. Despite the small number of respondents formally diagnosed with PD, its association with CImp remains significant after the powerful effects of education, age, ADLimp, and Mexican-American ethnicity are removed from the statistical equation . The ORs for PD sufferers are 4.14 on the MMSE, 4.12 on CLOXII, and 10.51 on CLOXII. It should be noted that effects of tremor on ability to draw do not contribute to cognitive function scoring on either of these Clock drawing tests , or drawings associated with the MMSE . Thus, along with above cited research findings, we suggest that our PD findings are clinically meaningful. We suggest that medical professionals involved with the treatment of PD patients be aware of the possibility of a PD-CImp connection during ongoing treatment.
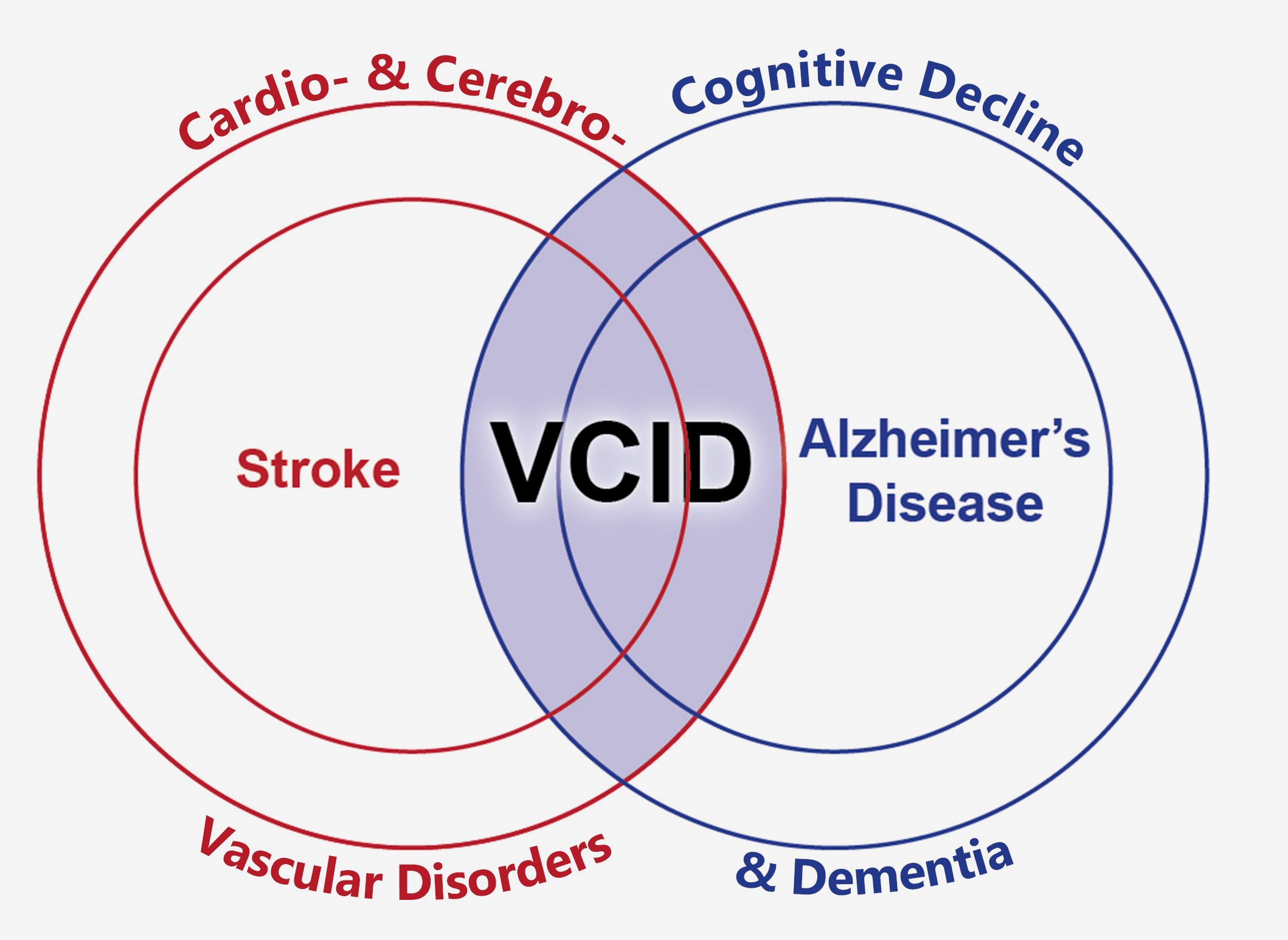
Is There A Proposed Mechanism Of Vascular Parkinsonism
Ischemic basal ganglia or subcortical white matter lesions disrupt interconnecting fiber tracts between the basal ganglia, thalamus, and motor cortex leading to disruption of sensory-motor integration as well as descending reticular pathways to major centers of the brain stem.
Infarctions affecting basal ganglia lacunae, including the thalamus, external globus pallidus, and putamen, that extend into the caudate and internal capsule, can mimic features of idiopathic PD. The second form with subcortical white matter lesions often produces clinical features resembling the classical lower body parkinsonism and has a more relentless rather than step-wise progression.
Cognitive Impairment And Dementia In Vascular Parkinsonism
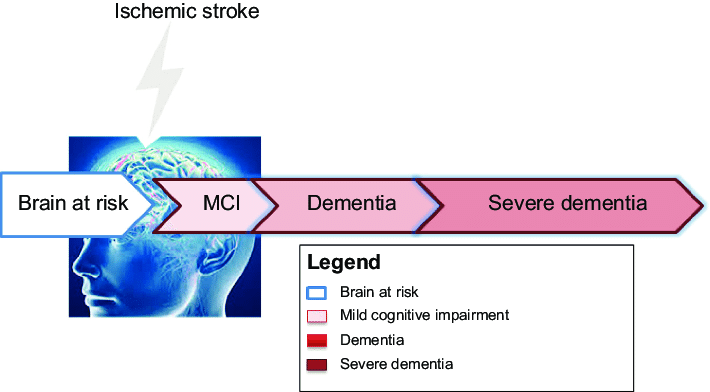
Unlike in PD, cognitive decline can occur in VP at presentation or develop early inthe disease course. The dementia in VP is subcortical, manifesting as dysexecutivesyndrome with impairment of attention, planning, judgment, goal-directed behaviour,abstract thinking, verbal fluency, in association with behavioural problems,especially apathy, which becomes more common and severe in later stages.,-
In the study by Zijlmans et al.of 17 patients with VP, five had some degree of cognitive dysfunction at the time oftheir initial presentation with Parkinsonism. In two, dementia was later confirmedby neuropsychological testing, while in two others, a frontal lobe syndrome withslowing of thought processes, loss of abstract thinking, apathy and perseverationwere seen. The fifth patient had isolated short-term memory impairment. Six otherpatients developed cognitive decline after disease onset, progressing to dementia infour.
In the Bambuí Study, eightof the 13 VP patients presented the diagnosis of VD, a feature that was moreprevalent than in PD cases.
You May Like: Does Sam Waterston Have Parkinson
Risk And Protective Factors
Risk factors are factors associated with an elevated incidence rate ofdisease, higher odds of developing disease, or earlier onset of disease,depending on the type of statistical analysis that is performed. Protectivefactors represent the converse. An observed risk factor does not necessarilycause disease a protective factor does not necessarily prevent disease andalmost certainly will not treat the disease. The observed effects canpotentially reflect selection or survival bias or confounding, or sometimesreverse causality. They may also depend on the timing and duration of exposureto the factor, with mid-life often being the critical period.
Vrfs And Wmls And Risk Of Pd
Concerning WMLs, we found an association with a trend towards significance with a Wahlund score greater than 4 and PD-MCI. This finding is in agreement with the longitudinal studies carried out by Chahine et al. and by Sunwoo et al. Similarly, Stojkovic et al. reported an association between WMLs and PD-MCI with a trend towards significance . However it should be noted that in the study carried out by Park et al. the presence of severe cerebral small vessel disease in the basal ganglia was found to be strongly associated with PD-MCI.
In our study we did not find any association between tobacco smoking and occurrence of neither PD-MCI nor PDD. In the general population, the role of nicotine in favoring or preventing cognitive decline is still controversial. In particular, if on the one hand nicotine increase oxidative stress-related cerebrovascular damage, favoring cognitive decline, on the other hand it could counterbalance cholinergic deficits preventing dementia.. However, a recent meta-analysis of prospective cohort study, reported that tobacco smoking increased the risk of cognitive decline in PD .
You May Like: How Do You Treat Parkinson’s Disease Naturally
Assessment Of Control Variables
Control variables include ethnicity, life satisfaction, education, age and sex. Ethnicity is defined through respondent’s self-selection and childhood and adolescent developmental history. This procedure has yielded samples of 799 elderly Mexican Americans and 353 NHWs. Life satisfaction is measured with a 12-item scale containing the response format, “Disagree”, “?” “Agree”. Total scale scores can range 12-36. Chronbach’s alpha for this scale is 0.77 among the El Paso County sample. Life Satisfaction is included as a control variable because quality of life and/or life satisfaction appear to be associated with diabetes and PD . This variable is also linked with functional capacity and cognitive function .
Educational attainment is included because of its powerful influence on time of onset for cognitive impairment and is measured as years of formal education, including ordinal categories for “high-school graduate”, college graduate”, and “at least some post-college education”. Thirty-five percent of the Mexican-American sample possesses at least a high school degree, thus providing a meaningful comparison between ethnic groupings. Age and sex are also included as control variables.
What Are The Imaging Findings In Vascular Parkinsonism
The literature in neuroimaging in VP is scarce. Computer tomography, magnetic resonance imaging , and cerebral angiography can be performed to delineate lesions. Even though imaging findings in VP are nonspecific and poorly defined, there are certain findings that would suggest VP over idiopathic PD. Ischemic changes in multiple vascular territories, periventricular white matter ischemia, global subcortical ischemic white matter involvement, ischemia in the basal ganglia and brain stem, and cortical atrophy are significant and more commonly seen in patients with VP
You May Like: Parkinson’s And Boxing Connection
Clinical Features And Diagnostic Criteria
The clinical picture of VP is heterogeneous. Several clinical features have beendescribed relating brain vascular lesions to Parkinsonism. A clinical diagnosis ofVP remains difficult to establish as infarction of the basal ganglia and deep whitematter occur frequently in elderly people who do not have Parkinsonism and vascular lesions are a commonincidental finding in pathologically-confirmed PD. Hence, a large proportion of patients withlate-onset PD have some degree of white-matter change on CT/MRI brain scans.
Given its clinical heterogeneity, Fénelon and Houéto stratified VP into four typesaccording to clinical manifestations:
-
VP manifesting in a manner identical to PD
-
unilateral Parkinsonism following contralateral vascular lesion
-
“atypical” Parkinsonian syndromes
-
“Parkinsonian” gait disorders.
Unilateral Parkinsonian syndromes caused by contralateral vascular lesions represent”pure” VP, whose criteria include the appearance of unilateral Parkinsonismfollowing an ischemic and haemorrhagic stroke in the substantia nigra, thalamus orat strategic locations that disrupt the striatopallidal loop. Striatal or striatopallidalischemic lesions have been more frequently observed than substantia nigralesions.,,
In 2004, Ziljmans et al. proposednew clinical criteria for diagnosing VP based on their clinico-pathological findings.
What Is Parkinson Disease
Parkinson disease is a movement disorder. It can cause the muscles to tighten and become rigid This makes it hard to walk and do other daily activities. People with Parkinsons disease also have tremors and may develop cognitive problems, including memory loss and dementia.
Parkinson disease is most common in people who are older than 50. The average age at which it occurs is 60. But some younger people may also get Parkinson disease. When it affects someone younger than age 50, it’s called early-onset Parkinson disease. You may be more likely to get early-onset Parkinson disease if someone in your family has it. The older you are, the greater your risk of developing Parkinson disease. It’s also much more common in men than in women.
Parkinson disease is a chronic and progressive disease. It doesn’t go away and continues to get worse over time.
Also Check: Are There Service Dogs For Parkinson’s Patients
Parkinson’s Diabetes And Cognitive Impairment
Logistic regression results are summarized in Table 1. Shown for MMSE, CLOXI and CLOXII are variable-by-variable effects on CImp after controlling for effects of all other variables in the equation. Blocks 1 in Subtable 1A, Subtable 1B, and Subtable 1C indicate that diabetes and PD are significantly, and somewhat independently, associated with CImp on all three measures. The OR of 1.95 for diabetes in Subtable 1A indicates that respondents with diabetes possess odds for MMSE-impairment 1.95 times those of their non-diabetic counterparts. The corresponding OR for respondents diagnosed with PD is 6.31. Similar outcomes are found in Subtable 1B, and Subtable 1C when CImp is measured with CLOXI and CLOXII. The odds for executive function impairment among those enduring PD are 6.31 times those for non-sufferers. The corresponding OR for elderly respondents diagnosed for diabetes is 1.47. Both diseases appear to impair cognitive performance related to the straightforward copying task required in CLOXII. Relevant ORs for PD and diabetes in Subtable 1C are 14.74 and 1.87.
White Matter Lesions Assessment
Patients underwent 1.5 T MRI scan ±1 month the baseline neuropsychological evaluation.
WMLs were defined as areas of hyperintensities on either T2 or FLAIR images, using a validated semiquantitative method proposed by Wahlund et coll . Two blinded neurologists have independently evaluated the findings on MRI images.
Don’t Miss: Stabilizing Spoon For Parkinson’s
Vascular Parkinsonism Mimics Array Of Traits
PORTO, PORTUGAL Vascular parkinsonism displays a range of noncognitive symptoms, which explains why its diagnosis can depend on the bias of the specialist doing the evaluation, said Joseph Ghika, M.D., at the Fourth International Congress on Vascular Dementia.
The same group of symptoms might be referred to as vascular parkinsonism by movement disorder specialists, central incontinence by urologists, vascular depression by psychiatrists, apraxia of gait by neuropsychologists, gait disorder of hydrocephalus by neurosurgeons, cardiogenic dementia by cardiologists, senile gait disorder by geriatricians, and small- and/or large-vessel disease by stroke specialists, said Dr. Ghika of the Centre Hospitalier Universitaire Vaudois in Lausanne, Switzerland.
Vascular parkinsonism accounts for 3%6% of all Parkinson’s disease cases. The evolution of vascular parkinsonism is more rapid than that of PD and may have a stepwise progression. Generally, patients with vascular parkinsonism are older than those with PD and have vascular risk factors. They are usually nonresponsive to dopa treatment.
Presentation may involve a number of symptoms that are not seen in other forms of cognitive impairment/dementia: gait disturbances , focal deficits, loss of sphincter control, emotional lability , and psychomotor slowing.
Neurocognitive Disorder Due To Huntingtons Disease
Huntingtons disease is a neurodegenerative disease caused by anautosomal dominant mutation consisting of CAG repeats on Chromosome 4. Theneurotoxic Huntingtin protein begins by damaging the striatum of the basalganglia but eventually affects the entire brain. Although adult onsetHuntingtons disease usually manifests in the fourth or fifth decades,patients have a median survival of 15 20 years after diagnosis, and canthus present to geriatric services. A few patients develop their first symptoms atolder ages in the absence of a family history. Progressive cognitive impairment toeventual dementia is inevitable. Although cognitive deficits and behavioral symptoms often emerge before the motor abnormalities , clinical diagnosis is rarely made on the basis of cognitive symptoms alone.A family history of the disease should alert clinicians to the possibility, andgenetic testing for the HTT mutation is diagnostic.
Read Also: Loss Of Smell And Parkinson’s
How Is Parkinson Disease Treated
Parkinson disease can’t be cured. But there are different therapies that can help control symptoms. Many of the medicines used to treat Parkinson disease help to offset the loss of the chemical dopamine in the brain. Most of these medicines help manage symptoms quite successfully.
A procedure called deep brain stimulation may also be used to treat Parkinson disease. It sends electrical impulses into the brain to help control tremors and twitching movements. Some people may need surgery to manage Parkinson disease symptoms. Surgery may involve destroying small areas of brain tissue responsible for the symptoms. However, these surgeries are rarely done since deep brain stimulation is now available.
Functional Decline And Cognitive Impairment
No such doubts exist about the relationship between cognitive and functional and impairments. Results reported in Table 1 indicate that for each unit increase in ADLimp there is a corresponding 1.33 unit increase in odds for MMSE impairment. Corresponding ADL findings for CLOXI and CLOX2 are 1.22 and 1.21. The significant nature of these associations is compatible with those reported in a large number of other studies, including the above-cited. The only debate in this area appears to be causal direction. Is ADLimp a derivative of CImp, or is this relationship more reciprocal in nature? Whatever the causal connection, these statistically significant findings are clinically relevant to medical professionals who deal with patients undergoing cognitive decline.
Recommended Reading: Drugs Prescribed For Parkinson’s Disease
Neuropsychological And Behavioral Assessment
At baseline and follow-up examinations, all PD subjects underwent a comprehensive neuropsychological and behavioral assessment in on state. The following five cognitive domains were evaluated with two tests for domain: episodic memory attention executive functioning visuo-spatial functioning language . Neuropsychological tests were considered as impaired when the subject scored two standard deviation below normality cut-off values. Diagnosis of PD-MCI was made according to the Movement Disorder Society Task Force criteria-level II . Diagnosis of PDD was made according to the MDS criteria . Details about the neuropsychological assessment used in the PACOS have been extensively reported elsewhere .
Dementia In The Population
Prevalence, defined as the proportion of people with an illness in agiven population at a given time, is an index of the burden of disease in thepopulation. Incidence is the rate at which new disease occurs in a givenpopulation, i.e., the proportion of new cases in that population over a givenperiod of time. Incidence is therefore an index of the risk of disease in thatpopulation. Prevalence is a function of both incidence and duration. Since mostdementias are not curable, their duration reflects how long individuals livewith their dementia. Thus, the public health burden of dementia depends both onthe development of new cases and on the survival of those cases after onset holding incidence constant, groups with longer life expectancy will have higherprevalence.
Also Check: Music Therapy For Parkinson’s
Education And Cognitive Activity
Where educational opportunities are universal, higher education mayreflect innate reserve the process of education may also promote thedevelopment of reserve through mechanisms such as increased dendritic branching.Education may also reflect general socioeconomic status and thus also representquality of environmental factors like nutrition, or health care. Regardless ofmechanism, higher education is associated with lowerprevalence of dementia.
Bilingualism has been associated with delayedonset of dementia,independent of education, and may specifically protect against declines inattention and executive functioning.
Cognitive activity: Lifelong occupations that donot require higher education or skilled vocational training appear to beassociated with a higher risk of dementia., Several popular leisureactivities have been found associated with lower risk of dementia. Cognitively stimulatingactivities appear to have both protective and enhancing effects oncognition.
Csf Biomarkers In Pdd
Many studies on CSF aimed to identify biomarkers reflecting the abnormal protein aggregates associated with PDD. In the majority of them, the level of Aß was found reduced4952 whereas the levels of total and phosphorylated tau were increased49,50,53,54 or unchanged52,55 in PDD. The use of more or less strict definition for dementia and the inclusion of more or fewer patients with AD- memory problems can partially account for the discrepancies in the tau level reported.
Based on the data from cross-sectional and longitudinal studies there is the strongest evidence that low levels of A and increased levels of tau in the CSF at baseline might predict future cognitive decline in patients with PD.5659
We performed a longitudinal study in non-demented PD patients including CSF, neuropsychological and MRI at baseline and 18 months follow-up.60 We found that a combination of lower CSF A, reduced verbal learning, semantic uency, and visuoperceptual scores, as well as cortical thinning in superior-frontal/anterior cingulate and precentral regions, were predictive for PDD. In this sense, different studies have shown that a combination of clinical, biological, and neuroimaging markers could be predictive for deterioration in cognition in PD with good accuracy.59,61,62
Also Check: What Kills A Person With Parkinson’s Disease
Assessment Of Specific Diseases
Specific diseases are assessed by asking whether a doctor had told respondent that he/she had a heart attack , high blood pressure, diabetes , stroke, broken hip, cancer, arthritis , or Parkinson’s disease. Bivariate cross-tabulation findings indicate that, of these 8 diseases, only diabetes and PD significantly associate with all three measures of cognitive function only diabetes and PD are included in multivariate analyses. Almost 25% of our sample have been formally diagnosed with diabetes, as opposed to less than 2% with PD . Percentages for diabetes among Mexican Americans and NHWs are 30.5 versus 11.7, a significant difference clinically as well as statistically. Percentage differences in PD for the two ethnic groupings are not statistically significant . As can be seen in the 95% confidence interval summaries for PD the small number of formally diagnosed PD respondents renders odds ratio interpretation problematic. On the other hand, statistically significant results for small samples are highly salient. The degree of severity of Parkinson’s disease was considered to be mild to moderate in this sample. Patients with the diagnosis of Lewy Body dementia were excluded in order to maintain a minimum number of confounding variables.
Table 1: Logistic regression analysis predicting impaired cognitive functiona for parkinson’s disease and diabetes mellitus . View Table 1
Dementia With Lewy Bodies
Dementia with Lewy bodies is the second most common neurodegenerativedementia. The underlying disease is primarily characterized by alpha-synucleinmisfolding and aggregation within the pathognomonic Lewy bodies, which are alsofound in Parkinsons disease. Onset of symptoms is between the sixth andninth decades, and average survival is 57 years.
With insidious onset and gradual progression, the cognitive deficits aremost prominent in the domains of attention, visuospatial and executive functioning.Additional core features include fluctuating cognition, recurrent visualhallucinations, and parkinsonism.The key distinction between DLB and dementia of Parkinsons disease is basedon the temporal sequence of the cognitive impairment and the movement disorder. InDLB, cognitive impairment precedes the onset of parkinsonism, while in the latter,the cognitive impairment occurs in the context of established Parkinsonsdisease.
Suggestive features of DLB include REM sleep behavior disorder and severeneuroleptic sensitivity. Low dopamine transporter uptake in basal gangliademonstrated by SPECT or PET imaging has been proposed as a suggestive feature.Supportive clinical features include repeated falls and syncope, transient andunexplained loss of consciousness, severe autonomic dysfunction, hallucinations inother modalities, systematized delusions and depression.
Read Also: Stem Cells For Parkinson’s Disease Therapy