Selection And Appraisal Of Documents
All study designs were included if they used a non-pharmacologic intervention to treat apathy in PD, either as a primary or secondary outcome, and were published in the English language. Initial treatment studies were identified by a previous scoping review on apathy in PD . Two authors independently screened titles and abstracts for the initial scoping search and the updated search . At the abstract stage, any abstract that discussed the treatment of apathy in PD was included. Two authors independently screened full text articles for the initial scoping search and the updated search . At the full text stage, any article that discussed the treatment of apathy in PD with a non-pharmacologic intervention was included.
The quality appraisal of included studies was adapted from Booth and colleagues , which takes into consideration whether included studies address the theory being tested and whether included studies support conclusions drawn by the researchers . Two authors assessed quality of data.
Icipating In Clinical Trials
Clinical trials and their participants have revolutionized Parkinsons treatment, and have changed the lives dramatically of those affected. They have helped make available many new treatments in addition to improving the delivery methods of medications and new deep brain stimulation techniques.
Clinical trials are essential to the future of Parkinsons research, and APDA is committed to this vital effort.
A Review On Parkinsons Disease Treatment
5214526Tori K. Lee Eva L. Yankee
Department of Biology, Angwin, CA 94508, USA .
Received:First Decision:Revised:Accepted:Available online:Academic Editors:Copy Editor:Production Editor:
© The Author 2021. Open Access This article is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, sharing, adaptation, distribution and reproduction in any medium or format, for any purpose, even commercially, as long as you give appropriate credit to the original author and the source, provide a link to the Creative Commons license, and indicate if changes were made.
You May Like: Music Therapy For Parkinson’s
Monoamine Oxidase B Inhibitors
Selegeline is an example of this class of drug. It selectively and irreversibly inhibits intracellular and extracellular monoamine oxidase B and therefore reduces or delays the breakdown of dopamine to dihydroxyphenylacetic acid and hydrogen peroxide. The latter has been implicated in oxidative damage in dopaminergic neurons in the substantia nigra. It also inhibits reuptake of dopamine from the synaptic cleft. Adding selegeline to L-dopa may allow a reduction of the L-dopa dose of 10%15%, occasionally up to 30%.Mild L-dopa response fluctuations can often be reduced by adding selegeline. Monotherapy in de novo patients delays the need for additional treatment by approximately a year.Possible neuroprotective effects will be discussed later . Side effects of L-dopa, including dyskinesias and psychiatric problems, are potentially enhanced by selegeline. Orthostatic hypotension may also occur.
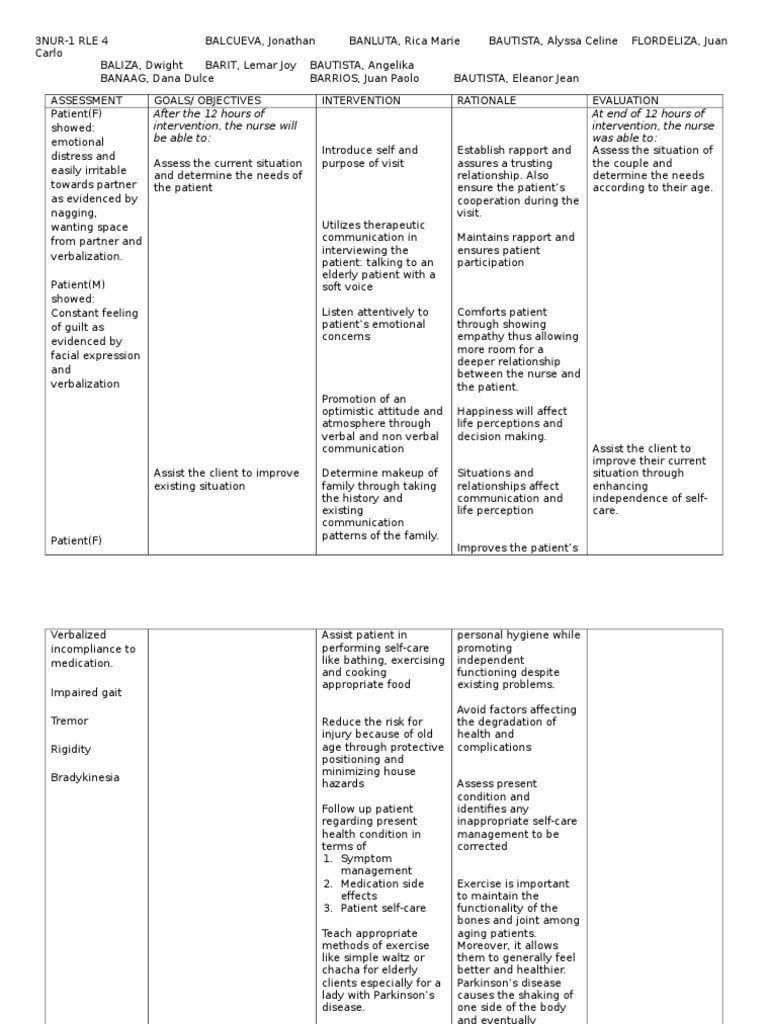
Causes Of Parkinsons Disease
Parkinsons disease is an idiopathic illness, which means that its cause is unknown.
The signs and symptoms it present are caused by the loss of nerve cells in the part of the brain called substantia nigra.
This part of the brain is responsible for the production of dopamine, a neurotransmitter that links the brain and nervous system to coordinate body movements.
Loss of dopamine results in uncoordinated body movements, thereby producing the signs and symptoms of the disease.
Though the exact cause of Parkinsons disease is still unknown, there are possible explanations that may be responsible for the condition, such as:
- Genetics. Studies have shown that a minority of cases of PD have genetic involvement.
- Environmental factors. Exposure to pesticides, herbicides, and industrial pollution is now being looked at as a possible cause of PD. However, the results are still inconclusive.
- Presence of Lewy bodies. Lewy bodies are clumps of substances in the brain cells. These are often seen in people with Parkinsons disease. The studies about them are still inconclusive, but researchers believe that these substances hold useful information to what causes PD. Researchers are also focusing into alpha-synuclein found in the Lewy bodies.
The following are the associated risk factors in developing Parkinsons disease:
Don’t Miss: Stem Cells For Parkinson’s Disease Therapy
Mindfulness Context Mechanism Outcome Configurations
From the two included mindfulness studies, we generated nine CMO configurations focused on explaining what mindfulness interventions, worked for whom, under what circumstances, and why . The Parkinsons active living program reduced apathy in persons with PD . The PAL program focuses on behavioural activation therapy. The PAL program uses program coaches that are paraprofessional and trained as interventionists, and encourages the involvement of caregivers . The program focuses on providing foundational skills in activity planning, scheduling, and monitoring to encourage self-management and independence. Further mechanisms that may lead to the improvements in apathy include providing treatment by telephone, to prevent transportation barriers. Semantics may also play an important role in the success of the PAL program, as the use of the term program instead of intervention has a more positive connotation . Personality may also play a role in the success of mindfulness interventions at improving apathy, given some persons may dislike scheduling or persons may be too concerned with disappointing program coaches to focus on the intervention . The other included mindfulness study found a mindfulness-based stress reduction program yielded non-statistically significant improvements in apathy among persons with PD and no cognitive impairment . Mindfulness interventions may not be completed by persons that prioritize physical components of PD over emotional and cognitive symptoms .
What Is The Outlook For Persons With Parkinsons Disease
Although there is no cure or absolute evidence of ways to prevent Parkinsons disease, scientists are working hard to learn more about the disease and find innovative ways to better manage it, prevent it from progressing and ultimately curing it.
Currently, you and your healthcare teams efforts are focused on medical management of your symptoms along with general health and lifestyle improvement recommendations . By identifying individual symptoms and adjusting the course of action based on changes in symptoms, most people with Parkinsons disease can live fulfilling lives.
The future is hopeful. Some of the research underway includes:
- Using stem cells to produce new neurons, which would produce dopamine.
- Producing a dopamine-producing enzyme that is delivered to a gene in the brain that controls movement.
- Using a naturally occurring human protein glial cell-line derived neurotrophic factor, GDNF to protect dopamine-releasing nerve cells.
Many other investigations are underway too. Much has been learned, much progress has been made and additional discoveries are likely to come.
Don’t Miss: Stabilizing Spoon For Parkinson’s
What Causes Parkinsons Disease
Parkinsons disease occurs when nerve cells in an area of the brain called the substantia nigra become impaired or die. These cells normally produce dopamine, a chemical that helps the cells of the brain communicate . When these nerve cells become impaired or die, they produce less dopamine. Dopamine is especially important for the operation of another area of the brain called the basal ganglia. This area of the brain is responsible for organizing the brains commands for body movement. The loss of dopamine causes the movement symptoms seen in people with Parkinsons disease.
People with Parkinsons disease also lose another neurotransmitter called norepinephrine. This chemical is needed for proper functioning of the sympathetic nervous system. This system controls some of the bodys autonomic functions such as digestion, heart rate, blood pressure and breathing. Loss of norepinephrine causes some of the non-movement-related symptoms of Parkinsons disease.
Scientists arent sure what causes the neurons that produce these neurotransmitter chemicals to die.
Parkinsons Disease Nurse Specialist Interventions
care has been pioneered in the UK over the last 10 years supported by the UK . A PDNSs role is defined as a practitioner with essential skills in:
- providing ongoing support and advice
- referral to other therapists
- education.
A recent report from the UK identified the key roles and responsibilities of the in the UK as:
- making and receiving referrals directly to create an integrated and responsive service for people with
- admitting and discharging people for specified conditions and within agreed protocols
- managing caseloads
- providing information, education and support to people in their homes, in clinics and in hospitals
- prescribing medicines and treatment and monitoring the effectiveness of changes in medication and treatment
- using the latest information technology to triage people with to the most appropriate health professional
- using IT to identify people at risk and speed up responses to crises.
What is the effectiveness of care versus standard medical care in the management of people with ?
Read Also: What Kills A Person With Parkinson’s Disease
Falls Can Be Prevented With Appropriately Prescribed Exercise In People With Mild To Moderate Pd
Physiotherapy aimed at preventing falls in people with PD should consider the individuals risk of falls and their fall risk factors. A systematic review showed that exercise reduces the frequency of falls in PD by 60 per cent . However, detailed investigation of randomised controlled trials indicates that when exercise is semi-supervised , falls are reduced in people with milder disease , but are increased in those with more advanced disease .
It is recommended that physiotherapists use the three-step clinical prediction tool to quickly and accurately predict an individuals probability of falling in the next six months as low , moderate or high . People with a low to moderate risk are suitable for group or semi-supervised physiotherapy that targets their remediable fall risk factors commencing as soon as possible after diagnosis.
Evidence is scant regarding intervention for people with high fall risk. However, a carefully monitored multidisciplinary approach, including medical review and higher levels of exercise supervision, along with environmental and behavioural modifications, is suggested.
How Do I Prevent Falls From Common Hazards
- Floors: Remove all loose wires, cords, and throw rugs. Minimize clutter. Make sure rugs are anchored and smooth. Keep furniture in its usual place.
- Bathroom: Install grab bars and non-skid tape in the tub or shower. Use non-skid bath mats on the floor or install wall-to-wall carpeting.
- Lighting: Make sure halls, stairways, and entrances are well-lit. Install a night light in your bathroom or hallway and staircase. Turn lights on if you get up in the middle of the night. Make sure lamps or light switches are within reach of the bed if you have to get up during the night.
- Kitchen: Install non-skid rubber mats near the sink and stove. Clean spills immediately.
- Stairs: Make sure treads, rails, and rugs are secure. Install a rail on both sides of the stairs. If stairs are a threat, it might be helpful to arrange most of your activities on the lower level to reduce the number of times you must climb the stairs.
- Entrances and doorways: Install metal handles on the walls adjacent to the doorknobs of all doors to make it more secure as you travel through the doorway.
Also Check: Drugs Prescribed For Parkinson’s Disease
How Is Parkinsons Disease Diagnosed
Diagnosing Parkinsons disease is sometimes difficult, since early symptoms can mimic other disorders and there are no specific blood or other laboratory tests to diagnose the disease. Imaging tests, such as CT or MRI scans, may be used to rule out other disorders that cause similar symptoms.
To diagnose Parkinsons disease, you will be asked about your medical history and family history of neurologic disorders as well as your current symptoms, medications and possible exposure to toxins. Your doctor will look for signs of tremor and muscle rigidity, watch you walk, check your posture and coordination and look for slowness of movement.
If you think you may have Parkinsons disease, you should probably see a neurologist, preferably a movement disorders-trained neurologist. The treatment decisions made early in the illness can affect the long-term success of the treatment.
Is Medical Marijuana An Option For Me
What’s next for a person with PD who wants to know if medical marijuana is an option? “Marijuana should never be thought of as a replacement for dopaminergic and other approved therapies for PD,” said Dr. Michael S. Okun, the Parkinson’s Foundation National Medical Advisor.
Research is still needed to determine how medical marijuana should be administered and how its long-term use can affect symptoms of PD. To keep patients safe, states that legalize medical marijuana will eventually need to develop training programs for doctors and medical teams that prescribe medical marijuana. Consult your doctor to see if medical marijuana is an option for you.
The Parkinsons Foundation is designed to help guide the PD community in making informed decisions about using cannabis for Parkinsons. The statement is based on the input from 46 experts who attended the Foundations first-ever medical marijuana convening. Read it now.
Page reviewed by Dr. Bhavana Patel, Movement Disorders Fellow at the University of Florida, a Parkinsons Foundation Center of Excellence.
Read Also: Does Sam Waterston Have Parkinson
Anticholinergics For Early On
The first pharmacological agents used in PD therapy were anticholinergic drugs. They reduce the activity of acetylcholine by acting as antagonists at choline receptors, hoping to restore the balance between dopamine and acetylcholine levels that was disturbed by PD. These drugs have largely been replaced by L-DOPA and other centrally acting dopaminergic agonists, but they still remain available for use in the treatment of PD. Benztropine, biperiden, diphenhydramine, ethopropazine, orphenadrine, procyclidine, and trihexyphenidyl are included in this therapeutic class of drugs, though there is little pharmacokinetic information available on them because of their low plasma drug concentrations. Typically, anticholinergic drugs have a greater role in tremor-predominant PD and can be a monotherapy in early stages, but are usually done in adjunct with L-DOPA or other prescribed medications.
How Well Do The Outcomes Of The Intervention Provided To Mr Jennings Match Those Suggested By The Systematic Review
The interventions provided for Mr Jennings were most similar to those in the general physical therapy and exercise trials. Tomlinson et al reported significant improvements in the FRT with data from the exercise and cuing groups and in the TUG with data from the exercise, cuing, dance, and martial arts groups. Mr Jennings’ improvements in balance, as evidenced by the FRT and TUG results , were at the high end of the changes reported by Tomlinson et al.
Only limited data for the minimal clinically important difference of measures in people with PD are available they are predominantly from one study to date. The data reported may have been from people with much greater impairments, as indicated by the changes noted they would have been improbable for Mr Jennings, given his baseline status. Mr Jennings’ 6-minute walk test change score met the criterion of 50 m as the minimal clinically important difference reported for a variety of people with a variety of cardiopulmonary diagnoses.
Changes in FAR were not reported in the systematic review, but it is noteworthy that the change in FAR for Mr Jennings was at the high end of the improvements reported by Schenkman et al. No comparison data were found for the other 2 outcomes.
Don’t Miss: How Long Does A Parkinson’s Patient Live
Speech And Language Therapy
Deterioration in speech is a common manifestation of that increases in frequency and intensity with the progress of the disease.
The specific resulting from is known as hypokinetic dysarthria and it is characterised by:
- monotony with reduced loudness and pitch range
- difficulties in initiating speech
- imprecise consonant
- breathy or harsh voice.
Treatment programmes have focused on specific components of the such as respiratory exercise and prosodic exercises. These treatments can be used with individuals or in groups.
is a speech therapy programme developed specifically for individuals with . It focuses on improving voice loudness with immediate carry over into daily communication. The intensive nature of the programme helps individuals with PD to recognise that their voice is too soft, convince them that a louder voice is within normal limits and makes them comfortable using the new louder voice. It is now provided by certified clinicians in England.
Some people with may benefit from use of augmentative and alternative communication devices, which can include the use of:
- alphabet boards
Symptomatic And Neuroprotective Therapy
Pharmacologic treatment of Parkinson disease can be divided into symptomatic and neuroprotective therapy. At this time, there is no proven neuroprotective or disease-modifying therapy.
Levodopa, coupled with carbidopa, a peripheral decarboxylase inhibitor , remains the gold standard of symptomatic treatment for Parkinson disease. Carbidopa inhibits the decarboxylation of levodopa to dopamine in the systemic circulation, allowing for greater levodopa distribution into the central nervous system. Levodopa provides the greatest antiparkinsonian benefit for motor signs and symptoms, with the fewest adverse effects in the short term however, its long-term use is associated with the development of motor fluctuations and dyskinesias. Once fluctuations and dyskinesias become problematic, they are difficult to resolve.
Monoamine oxidase -B inhibitors can be considered for initial treatment of early disease. These drugs provide mild symptomatic benefit, have excellent adverse effect profiles, and, according to a Cochrane review, have improved long-term outcomes in quality-of-life indicators by 20-25%.
Neuroprotective therapy aims to slow, block, or reverse disease progression such therapies are defined as those that slow underlying loss of dopamine neurons. Although no therapy has been proven to be neuroprotective, there remains interest in the long-term effects of MAO-B inhibitors. Other agents currently under investigation include creatine and isradipine.
Don’t Miss: How Do You Treat Parkinson’s Disease Naturally
Physiotherapy Intervention In Parkinsons Disease: Systematic Review And Meta
- Accepted 4 July 2012