My Parkinson’s Story: Pain
This 10-minute video alternates between an interview with a man and and doctors. The man shares his experience with pain as a symptom of Parkinson’s disease. The doctors explain that pain is common in Parkinson’s disease, often due to rigidity or dystonia, which can be exacerbated by “off” periods. Pain caused by Parkinson’s symptoms can be relieved by Parkinson’s medications, exercise, DBS and botox injections. Pain is an invisible symptom that should be mentioned to your neurologist.
What Can We Do
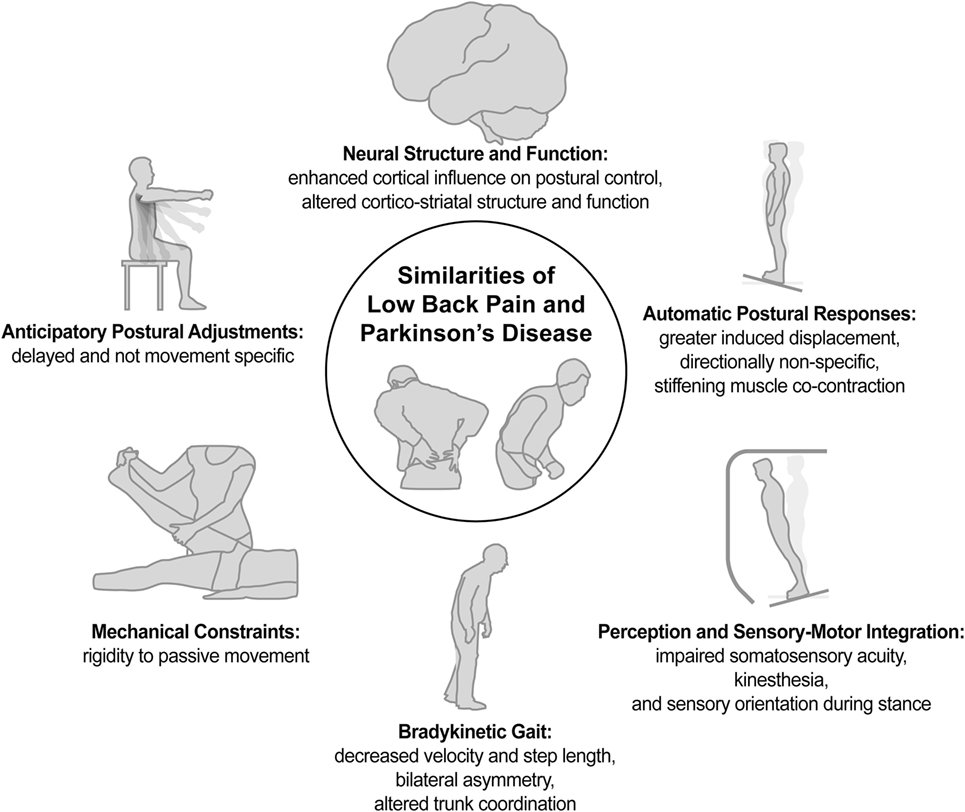
It would seem to me that there are a number of very vicious circles and negative feedback loops between neck stiffness/rigidity/pain and neck immobilization and posture in PD, which not only impact on each other, but also have neurological and physiological implications much more broadly, including on nervous system, blood pressure and breathing. The principal strategy for progressive symptom reduction would therefore be to increase and maintain mobilization of the neck and to improve posture as much as possible, through daily exercises and therapies, and to address any old injuries elsewhere on the body which may be impacting on posture and hence neck strain.
Dr Farias provides a suite of daily exercises which help to reduce these type of neck problems over time, especially designed for, and tailored to the different types of, cervical dystonia. Many people around the world report that doing his exercise classes daily reduces the symptoms and pain of their neck dystonia, and can eventually even lead to a full recovery. This works through a process of neuroplasticity, which re-wires the connections between the muscles and the brain through movement therapy.
Muscle Weakness And Rigidity
As his Parkinsons progresses, Dad complains that his stiffness is slowing him down. The frequency and intensity with which it occurs seem to be increasing. To better understand the disease and how it relates to the body, I decided to explore the research.
In an abstract of a literature review published by the American Journal of Physical Medicine & Rehabilitation, the authors stated that isokinetic muscle strength was decreased in patients with Parkinsons disease and that muscle weakness was not specifically related to tremor or rigidity.
Read Also: Ultrasound Treatment For Parkinson’s Disease
How Is Parkinsons Disease Treated
There is no cure for Parkinsons disease. However, medications and other treatments can help relieve some of your symptoms. Exercise can help your Parkinsons symptoms significantly. In addition, physical therapy, occupational therapy and speech-language therapy can help with walking and balance problems, eating and swallowing challenges and speech problems. Surgery is an option for some patients.
How Will My Doctor Test For Rigidity
At your appointment, your doctor will ask you to keep your limbs as relaxed and loose as possible. Then, they will gently flex and extend your joint, such as your elbow, wrist, or shoulder. If youre experiencing rigidity, your doctor will feel an increased resistance to movement in both directions extension and flexion. A unique aspect of cogwheel rigidity is that the jerky motion occurs at both slow and fast speeds.
Also Check: Parkinson’s Disease And Cough Medicine
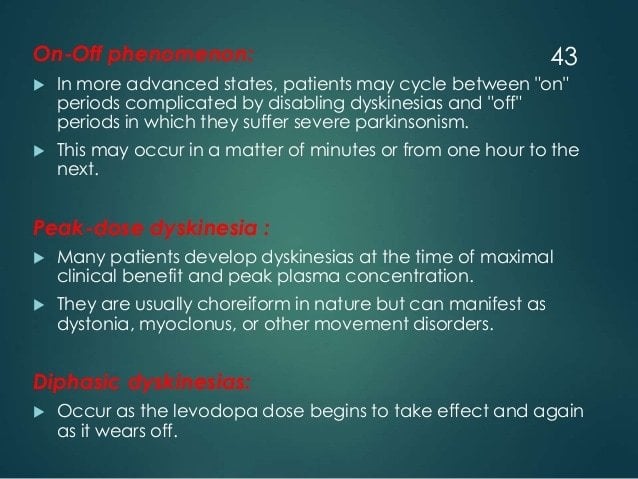
Fluctuations Of Pain Experiences In Pd
Patterns of NMS fluctuations are heterogeneous and complex. Psychic NMS seem to fluctuate more frequently and severely than nonpsychic symptoms. A recent study of ten frequent NMS in advanced PD using VAS rating scales in motor-defined on- and off-states, as well as self-ratings at home, confirmed previous suspicions that increased pain in off-states and pain fluctuations correlate with a low health-related quality of life. Pain as NMS was more frequent in the off-state more precisely, it was three to four times more common during the off-state than during the on-state.
Pain Stress And Biomarkers Of Stress
Stress and pain are often closely linked. Each has an impact on the other, creating a vicious cycle that sets the stage for chronic pain and chronic stress. Therefore, stress management should be a component in pain therapy.
The Merriam-Webster Encyclopedia® defines the term stress as a physical, chemical, or emotional factor that causes bodily or mental tension and may be a factor in disease causation. The result of stress can be explained as physical or mental tension resulting from factors that tend to alter an existing equilibrium.
You May Like: How Long Parkinson Patients Live
Mental Status And Social Networks
As previously mentioned, depression and pain are significant clinical problems that are comorbid with PD. Marital status, as well as other social networks, interferes with these conditions. The patientspouse relationship, which indicates physical and emotional support, may have a mitigating effect on patient outcomes of depression prevalence and pain interference. Single PD patients seem to have greater pain interference scores than cohabiting PD patients.
Who Should I See To Discuss My Parkinsons Pain
Your first point of contact should be your primary doctor. Whether that means your family doctor, neurologist, or Movement Disorder Specialist , start by asking them how to manage your pain. They may prescribe you one of the medications listed above, offer suggestions about altering your lifestyle, or refer you to a pain specialist.
Pain management specialists are physicians with specialized training in the field of evaluating, diagnosing, and treating pain so, speaking to one of these specialists might be helpful for you. Be sure to get a referral from your primary care doctor, though, to ensure you are visiting a physician who understands the complexity of treating Parkinsons-specific pain.
Health and wellness providers like physical therapists, acupuncturists, and massage therapists can also be valuable members of your care team. Be willing to try new things and approach alternative therapies with an open mind, as no ones path with Parkinsons pain is the same. What works for someone else may not work for you and vice versa. Consider visiting different specialists to find a treatment plan that works best for you.
Don’t Miss: Vascular Parkinsonism And Cognitive Impairment
Stages Of Parkinsons Symptoms
Parkinsons symptoms can be divided into three categories or phases: pre-motor, motor, and cognitive. These phases dont necessarily happen in chronological order, and not all Parkinsons patients will experience all symptoms.
The premotor phase is the phase of Parkinsons in which non-motor symptoms are present. These symptoms include:
- loss of smell
- torso
- legs
There are two main categories of tremor: resting tremor, and action tremor. Resting tremor occurs when muscles are relaxed, like when your hands are sitting in your lap, and lessen during sleep or when the body part is in use. Action tremors occur with the voluntary movements of a muscle.
Tremors typically affect only one side of the body but may affect both sides as the disease progresses. Fatigue, stress, and intense emotion may worsen tremors.
Make Commercial Breaks Movement Breaks
If youre watching TV, stand up and march while you swing your arms during the commercials. To increase your muscular strength, lift soup cans or a do a few downward dogs.
Moving more every day is easier said than done. Remember, even small changes can make a big difference. Pat yourself on the back for all of the movement activities you do each day. Every victory counts!
Recommended Reading: Nad Therapy For Parkinson’s Disease
Increased Urination Urgency And Frequency
Bladder problems are a common occurrence in people with Parkinsons, occurring in 30-40 percent of people with the disease. The most common urinary symptom is a frequent and urgent need to urinate even when the bladder is empty, as well as trouble delaying urination.
Trouble emptying the bladder is a less common feature of Parkinsons urinary dysfunction. It may be caused by difficulty in relaxing the urethral sphincter muscles that allow the bladder to empty.
Revisiting Pain In Pdthe 50 Shades Of Pain Experienced By Parkinsons Patients
Pain is a quality of life issue for people with Parkinsons disease and can be under treated by doctors who may assume that is worsens as the disease progresses, although for some pain is an initial symptom of PD. This article helps focus your physicians attention in the right direction to accurately diagnose your pain.
Read Also: Social Security Blue Book Parkinson’s
Lifestyle Changes For Muscle Atrophy
Along with medication making some positive changes in the lifestyle can be of great help in coping up with the physical limitations in movement. Instead of blaming god and others for the problem, it is better to adapt with the condition and look for ways to improve. One very common problem, which almost all the people suffering from Parkinsons disease face is getting up and sit in the chair. However, having a lifted chair or customizable chair can be of great help to cope with this physical limitation similarly, making a use of physical support tool while walking can help in maintaining balance and avoiding any fall or injury.
Also Read:
Difficulty Swallowing Or Eating
Parkinsons affects the muscles in the face, mouth, and throat that control speaking and swallowing. Dysphagia, or difficulty swallowing, is a symptom of Parkinsons that can lead to trouble eating.
It can lead to malnutrition, dehydration, or aspiration which happens when food or saliva goes down the wrong pipe and is inhaled into the lungs. Aspiration can lead to aspiration pneumonia, the leading cause of death in Parkinsons.
Also Check: Working Out With Parkinson’s
Development Of A New Approach
Different classifications have been employed for the distinction between PDrelated and PDunrelated pain syndromes, but motor fluctuations and the response to dopaminergic medication were not usually taken into account, except in the most recent approaches., We here provide an original questionnaire for pain assessment in PD. It can be used in addition, or as an alternative, to the questionnaire currently being developed by the nonmotor study group of the International Parkinson and Movement Disorder Society.,
Our approach is based on a threestep approach: establish a relationship with PD on the basis of a temporal association between the onset of pain and PD symptoms, whereas other causes of pain are excluded determine whether pain depends on motor fluctuations and determine whether pain depends on the antiparkinsonian treatment. At the end of this threestep approach, pain could be classified as a PDrelated or nonPDrelated pain. Finally, concerning PDrelated pain, the type of pain is categorized as one of three main syndromes, . The proposed algorithm was converted into a pain questionnaire named MarburgSao PauloCréteil Questionnaire for Pain in Parkinson’s disease .
The fluctuation with the dopaminergic state may give an additional hint for an association between pain and PD in moreadvanced cases. Thus, the effects of any antiparkinsonian treatment on pain should be systematically included in the diagnostic algorithm, as recently proposed.
Can Parkinsons Disease Be Prevented
Unfortunately, no. Parkinsons disease is long-term disease that worsens over time. Although there is no way to prevent or cure the disease , medications may significantly relieve your symptoms. In some patients especially those with later-stage disease, surgery to improve symptoms may be an option.
Don’t Miss: Plan Of Care For Parkinson’s Disease
What Are The Different Stages Of Parkinsons Disease
Each person with Parkinsons disease experiences symptoms in in their own unique way. Not everyone experiences all symptoms of Parkinsons disease. You may not experience symptoms in the same order as others. Some people may have mild symptoms others may have intense symptoms. How quickly symptoms worsen also varies from individual to individual and is difficult to impossible to predict at the outset.
In general, the disease progresses from early stage to mid-stage to mid-late-stage to advanced stage. This is what typically occurs during each of these stages:
Early stage
Early symptoms of Parkinsons disease are usually mild and typically occur slowly and do not interfere with daily activities. Sometimes early symptoms are not easy to detect or you may think early symptoms are simply normal signs of aging. You may have fatigue or a general sense of uneasiness. You may feel a slight tremor or have difficulty standing.
Often, a family member or friend notices some of the subtle signs before you do. They may notice things like body stiffness or lack of normal movement slow or small handwriting, lack of expression in your face, or difficulty getting out of a chair.
Mid stage
Mid-late stage
Standing and walking are becoming more difficult and may require assistance with a walker. You may need full time help to continue to live at home.
Advanced stage
How Is Pain Diagnosed Assessed And Treated
Diagnosing and treating pain in people with Parkinsons can be difficult and often, common ways of reducing pain, such taking painkillers or doing regular, gentle exercise may not help.
Usually, your doctor or Parkinsons nurse specialist will be able to help you to manage the more common types of pain, such as shoulder pain and headaches. Certain other types of pain, however, such as pain caused by involuntary movements or burning mouth, may need the help of your Parkinsons specialist.
Completing a Kings Parkinsons Disease Pain Questionnaire and showing it to your heath-care professional will help them to understand the pain you are suffering from1. Completing the 24-hour Hauser2 diary, a home diary designed to assess your motor symptoms, over the same period of time, would further help your doctor or Parkinsons nurse to better understand the pain you are experiencing and to treat it more quickly.
To ensure Parkinsons pain is assessed and diagnosed efficiently, a specific scale has been designed. Kings Parkinsons Pain Scale 1 is a validated scale which covers the common types of Parkinsons related pain. Your Parkinsons specialist might use this scale to help understand the type of Parkinsons pain you have even better and assess what needs to be done to help you further.
References:
You May Like: Does Weed Help With Parkinson’s
Examples Of Pain Scales
Visual analog scale
A visual analog scale measures a continuum of a chosen present characteristic. For example, the experienced pain that a patient feels extends over a continuum from no pain to an extreme intensity of pain. This range of perceived pain appears continuous for the patient. Pain does not appear as an ordinary scale with jumps between the values, such as discrete, moderate, or severe. Word descriptors are only used in both ends of the line, which is usually 100 mm in length. This valuation is very subjective and best used within an individual and not between groups of individuals at the same time point. Most experts argue that a VAS at best can produce data of ordinal type. This is important to consider in the statistical analysis of VAS data. Rank ordering of scores rather than the exact values might be the best way to handle patient registrations on the 100 mm line.
Brief Pain Inventory
The Brief Pain Inventory was initially created for the purpose of measuring pain in cancer patients. It measures pain relief, pain quality, and patient perception of the cause of pain in terms of pain intensity and pain interference .
What Can I Do On A Regular Basis To Manage My Pain
Remember, youre your best advocate as you understands how your pain feels. Understanding and communicating the kind of pain youre experiencing can greatly inform your treatment plan and will allow your doctors to address the type and severity of your specific pain. Keep your care team informed about activities that cause pain or the times of day your pain is worst so they can help fine-tune your care plan. Do you notice the pain starting to creep in at a certain point after you take your medication? Do you feel fine when you bike but experience pain when you jog? Did you start experiencing this pain before or after your Parkinsons diagnosis? Taking stock of these sorts of questions can be helpful as you work with your care team to effectively treat your pain.
Incorporating approved medications and following the pain ladder can also help you find the right pain management solution, as can taking steps in your everyday life to be an active participant in your own pain management. Regular stretching, heat and cold treatments, exercise, yoga, and dance can all help reduce your pain, and they are all steps that you can take on your own. Making adjustments to your home and workspace, such as minimizing places where fall risks are likely, using an ergonomically designed desk, sleeping in a comfortable bed, and wearing clothes and shoes that dont exacerbate pain, can help you establish a more pain-free daily routine.
Recommended Reading: Parkinson’s And Immune System
Is Accurately Targeted Treatment Possible
Single targeted surgery enables Parkinsons Syndrome Sufferers to be precisely treated with the minimum of damage to tissues, reduced patient risk and enhanced long-term outcome and more essentially without the use of General Anaesthesia. This treatment, which is called Foraminoplasty because it is carried out in the gaps or Foramen between the vertebrae, allows the nerve to thoroughly liberated and the overriding joints or pointed fracture margins to be removed. This is only possible by the use of Endoscopic Minimally Invasive Spine Surgery where the full length of the exiting nerve can be explored and the points of irritation clearly demonstrated. In the breadth of presentations arising from Degenerative Disc Disease and Failed Back Surgery or Failed Chronic Pain management, Endoscopic Lumbar Decompression & Foraminoplasty achieved a successful enduring positive outcome in 80% of cases.
Nerves And Nervous System
The vagus nerve is not the only important nerve which passes through the neck. According to the polyvagal research of Dr Stephen Porges, five of the cranial nerves form the parasympathetic ventral vagus complex, responsible for Social Engagement functions. Interestingly, this vagal complex includes the accessory nerve, that innervates the neck muscles used to turn the head. In his early paper on polyvagal theory, Dr Porges writes:
“Thus, more specialized functions such as head rotation to orient sensory receptors toward the source of stimulation, mastication to ingest food, and salivation to initiate gustatory and digestive processes are integrated into the vagal system.”
“In mammals, the part of the brain where these nerves originate controls the complex coordination of pharynx, soft palate, larynx, and esophagus. Of special note to psychophysiological processes the carotid body, containing peripheral chemosensitive receptors sensitive to oxygen and carbon dioxide levels”
“In addition, the accessory nerve provides fibers originating in the cervical spinal cord that innervate the positioning of the neck. The critical carotid arteries, internal jugular veins, and vagus nerves run deep in these muscles.”
“Thus, this complex also has the ability to orient visceral receptors via somatic muscles , to coordinate structures related to ingestion and expulsion, and to regulate facial expression and emotion.”
Also Check: How To Care For Someone With Parkinson’s Disease