What Is A Hallucination
A hallucination is a perception of something that does not actually exist. This may be visualised, heard, felt, smelled or tasted. Hallucinations are sometimes confused with illusions, which are distortions of a reality rather than something that is purely imagined – as with hallucinations.
Visual hallucinations: In Parkinson’s, hallucinations are most commonly visual and may be in black and white, in colour, still or moving. Often the images involve small animals and children. They may disappear quickly or may last for some time.
Auditory hallucinations: auditory hallucinations are less common. These generally involve hearing voices or other familiar sounds. Auditory hallucinations can also be part of a depressive symptomatology.
Tactile hallucinations: hallucinations may be tactile, that is, you may feel a sensation, like something touching you.
Smell and taste hallucinations: less commonly you may feel that you can taste something you havent eaten, or you may smell something that is not present, such as food cooking or smoke.
Usually hallucinations are not threatening or distressing. If you hallucinate you may be unaware that your perceptions are not real, and sometimes imagined images or sensations can be comforting. But hallucinations can also be distressing and you may feel threatened or frightened and may need reassurance and comfort from those around you.
Hallucinations In Parkinsons Disease
Hallucinations are seeing, hearing, or feeling something that is not actually there. Most hallucinations experienced in PD are visual, although some people experience auditory, tactile , or olfactory hallucinations. Hallucinations occur when the person is awakenot sleeping or dreamingand can occur at any time of day or night. They can be frightening, for the patient experiencing them as well as their caregiver. Generally, hallucinations are repetitive and last for a short duration.1,3
What Are Parkinsons Hallucinations
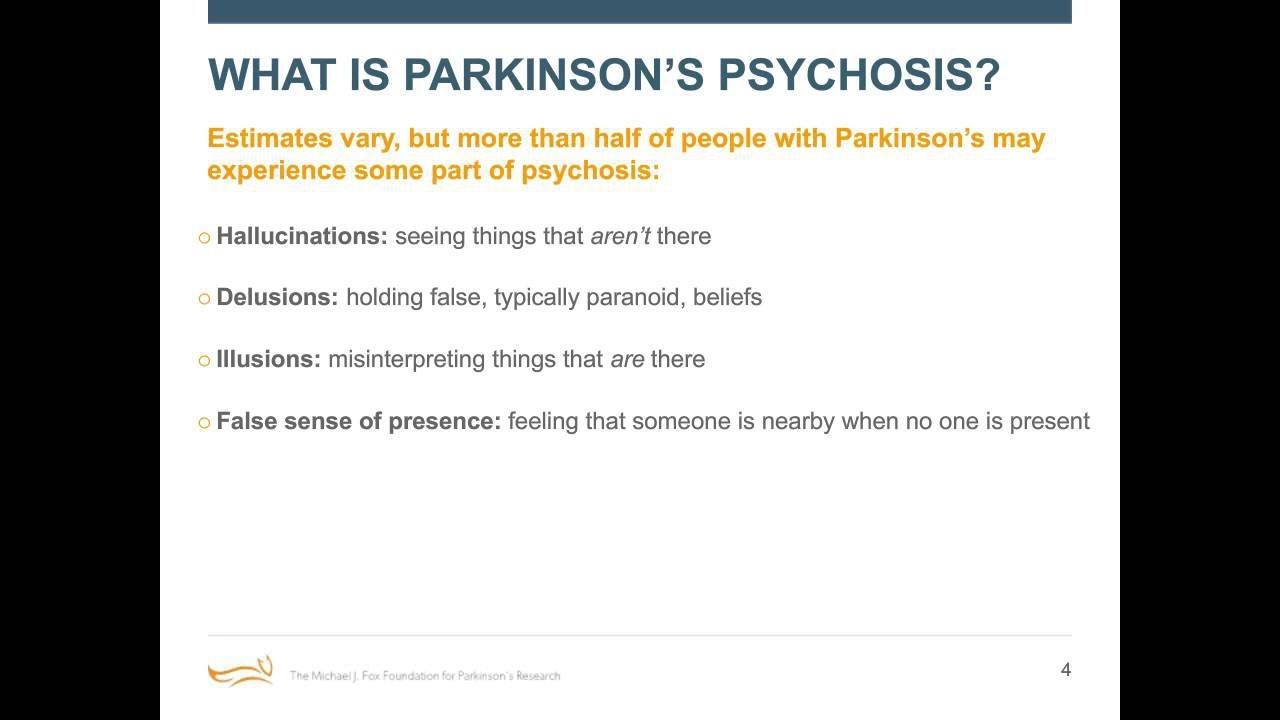
Symptoms of psychosis occur in up to 50% of people with Parkinsons disease.
Parkinsons disease psychosis is considered a neuropsychiatric condition. This means it involves neurology and psychiatry . While the psychosis involves mental health symptoms, they are caused by Parkinsons disease, which is a disease of the nervous system.
Psychosis in Parkinsons disease comes in two forms:
- Hallucinations: Sensory experiences that are not really happening
- Delusions: False beliefs not based on reality
These symptoms can be debilitating and scary for the people experiencing them. They can interfere with a persons ability to care for themselves and to relate to other people.
Psychotic symptoms in Parkinsons disease are associated with increased caregiver distress, risk of hospitalization and nursing home placement, and healthcare costs.
A study suggests the presence of hallucinations and delusions in people with Parkinsons disease is a predictor of mortality .
Don’t Miss: On Off Phenomenon In Parkinson’s Disease
Risk Factors For Parkinsons Hallucinations
Not much is known about what causes hallucinations with Parkinsons disease. Because people living with Parkinsons disease also are at risk of vision impairment, these problems may contribute to the occurrence of hallucinations. Older people and those with advanced stages of Parkinsons also tend to have a higher risk of hallucinations.
Hallucinations can be a side effect of a medication or caused by an infection. In these cases, the hallucinations are related to Parkinsons but not caused by the disease itself.
Predictive Factors And Pathophysiology
Minor hallucinations/illusions
Patients with isolated minor hallucinations/illusions differed from patients without hallucinations only by the presence of more depressive symptoms on the CES-D rating scale, suggesting that depressive symptoms are a facilitating factor. Indeed, depression may sometimes trigger or aggravate hallucinations associated with deafness or ocular pathology . However, when we analysed depression according to CES-D cut-off scores, the difference between the Parkinson’s disease patients with minor hallucinations/illusions and those with no hallucinations was not significant. Interestingly, hallucinations involving the deceased spouse have been reported in up to half of widowed persons, with a higher frequency in the elderly . In the present study, the `presence’ was that of a deceased relative in only three cases bereavement cannot therefore explain the bulk of the cases.
Dopaminergic agents and other treatments
In the present study, non-hallucinators were more likely to be on anticholinergics or selegiline than patients with hallucinations. A similar paradoxical, negative association between anticholinergics and hallucinations was found by Sanchez-Ramos and colleagues . This reflects the recommendation whereby the use of these drugs in patients with cognitive impairment is avoided because of the well-known risk of cognitive worsening and/or hallucinations in this population.
Cognitive impairment
Sleepwake disturbances
Motor status
Depression
Recommended Reading: Young Onset Parkinson’s Symptoms
What Should I Do Once The Hallucination Passes
After the hallucination passes, you can try to talk through the experience together. If the person has insight, it may be easier for them to understand and talk about what just happened.
Write down what happened during the hallucination. Note the time of day and what the person was doing when it started.
Taking notes each time it happens can help you identify the triggers. It could be related to the timing of medication, and your loved one might feel a sense of relief and control in knowing that pattern.
Ask what you can do to stop it from happening again. This might include adjusting their medication dosage or adding an atypical antipsychotic drug to their medication regimen.
Additional Drugs May Be Helpful
In addition to reducing your PD dosages, or removing certain meds from your treatment, there may also be additional drugs to try. If we reach a point where weve optimized medications and cant reduce any further because otherwise we would have more motor dysfunction, there are other medications we can add on to specifically address psychosis, explains Dr. Pan. There are three main options, she says, including Nuplazid , which the FDA approved for psychosis in PD in 2016, plus antipsychotics Clozaril and Seroquel . Your doctor can determine whats best for you.
Read Also: How To Improve Balance In Parkinson’s Disease
Other Symptoms Of Parkinsons Disease
There are numerous Parkinsons disease symptoms, some related to movement and some unrelated. In addition to hallucinations and delusions, people may experience other non-motor symptoms, such as poor sleep and vision problems, which often contribute to the development of hallucinations.
Other non-motor Parkinsons disease symptoms include:
How To Care For Someone Who Experiences Hallucinations
If the person you care for experiences a hallucination, there are a few things youll want to do in the moment and others youll want to do when the moment passes.
The most important thing to remember is to never try and talk the person with Parkinsons out of their hallucination. They are actively experiencing it and by trying to talk them out of it, they may either feel like they arent being heard or that their experience is being diminished.
What matters in the moment is their safety and your reassurance that theyre going to be okay. You might calmly say, I understand that youre seeing X. Im not having that experience, and I just want you to know that everything is going to be okay, theres nothing dangerous happening here and youre safe.
Other strategies Dr. Joanne Hamilton, PhD, ABPP-CN of Advanced Neurobehavioral Health of Southern California, shared with us are to:
Here are a few actions you can take once the hallucination has passed:
Don’t Miss: Parkinson’s Disease Therapeutic Regimen
Section Header Managing Psychosis With Medication
Dont keep hallucinations or delusions a secret from your doctor. Medications — or changes to the medications you take — can help manage Parkinsons psychosis.
Streamlining your meds. The first thing your doctor may want to do is stop or lower your Parkinsons medication dose. They may boost dopamine levels in your brain. That improves motor symptoms but can also cause changes in your emotions or the way you act.
Antipsychotics. These medications balance your brain chemicals. Only a few are considered safe for people with Parkinsons disease. These include quetiapine and clozapine .
Pimavanserin . Another antipsychotic, this first-in-class drug was approved by the FDA in 2016 to treat hallucinations and delusions in Parkinsons disease linked with psychosis.
If you see a doctor who isnt part of your usual care team — say, in the emergency room or an urgent care setting — tell them you have Parkinsons disease and what medications you take for it.
They Are Agitated Irritable Or Accusatory
Paranoid hallucinations, and the fears they induce, can make a person with Parkinsons related psychosis hostile. One common example: There can be delusions of sexual jealousy where they feel like their partner is having an affair, even though theyre not, says Barrett. This can be very frustrating for partners who are also caregivers.
Don’t Miss: Home Exercise For Parkinson Disease
Parkinsons Disease Psychosis: Hallucinations Delusions And Paranoia
As part of Parkinsons Disease and its treatment, hallucinations, illusions, delusions, suspiciousness and paranoid behaviors occur in over 50% of patients. In this 1-hour webinar Dr. Christopher Goetz suggests lifestyle changes, medication adjustments and a recently FDA approved drug to specifically treat psychosis in Parkinsons Disease.
Parkinsons Disease Psychosis: A Little
One of the lesser-known symptoms of Parkinsons Disease is Parkinsons psychosis. This webpage explains the prevalence, causes and symptoms, treatment options of PD psychosis. More useful to caregivers are sections on potential triggers of psychotic episodes and what caregivers can do about PD psychosis.
Read Also: Hoarse Voice Parkinson’s Disease
Recognizing Symptoms Of Delusions
People with Parkinsons delusions frequently believe they are being mistreated. As a result, people experience paranoia, mistrust, anger, and anxiety. Jealousy delusions usually a belief that a spouse is being unfaithful are very common. Persecutory delusions the false belief that someone is cheating or conspiring against you are also common. Persecutory delusions are often directed at someone the person with Parkinsons interacts with regularly, like a spouse, family member, or caregiver.
Caregivers on MyParkinsonsTeam share their experiences with jealousy and persecutory delusions:
- Husband still thinks I’m slipping out at night, which I understand is the number one delusion for a spouse!
- He is saying I am lying to him and he is showing signs of being paranoid.
- They provoke severe anxiety in my husband and sometimes he believes men are after him. He can become distrustful of me and his health care aide, whom he likes very much. These bad episodes can last one hour or six hours.
- My mom tells me I don’t feed her or I make her eat things that she doesn’t like.
Some delusions are more general confusions of reality. As one caregiver described, He mixes reality and old memories and TV programs and fantasy to create a different kind of reality. Another caregiver shared, He is POSITIVE we are not where we are, that he has two cats, etc.
Common Causes Of Hallucinations
Hallucinations most often result from:
- Schizophrenia. More than 70% of people with this illness get visual hallucinations, and 60%-90% hear voices. But some may also smell and taste things that aren’t there.
- Parkinson’s disease. Up to half of people who have this condition sometimes see things that aren’t there.
- Alzheimer’s disease. and other forms of dementia, especially Lewy body dementia. They cause changes in the brain that can bring on hallucinations. It may be more likely to happen when your disease is advanced.
- Migraines. About a third of people with this kind of headache also have an “aura,” a type of visual hallucination. It can look like a multicolored crescent of light.
- Brain tumor. Depending on where it is, it can cause different types of hallucinations. If it’s in an area that has to do with vision, you may see things that aren’t real. You might also see spots or shapes of light. Tumors in some parts of the brain can cause hallucinations of smell and taste.
- Charles Bonnet syndrome. This condition causes people with vision problems like macular degeneration, glaucoma, or cataracts to see things. At first, you may not realize it’s a hallucination, but eventually, you figure out that what you’re seeing isn’t real.
- Epilepsy. The seizures that go along with this disorder can make you more likely to have hallucinations. The type you get depends on which part of your brain the seizure affects.
Also Check: Parkinson’s Foundation Miami Florida
Managing Hallucinations And Delusions
Get medical advice. In mild cases simple monitoring may be all that is required. In more severe cases changes in medications may be necessary.Rule out other causes such as eyesight issues or infections.Talk to your family and or carers to help them understand how you are feeling. It can help them to be more patient and supportive with you too.Try not to worry.Reassure yourself that these symptoms may be a side effect of Parkinsons medication.Seek counselling. People with Parkinsons, carers and family members may need support, counselling and specific advice. Medicare covers 6 – 12 sessions with a psychologist to provide a range of strategies to help.
Support for you
Bringing Light To Darker Side Of Parkinsons
Often the hardest part of Parkinsons disease psychosis is the fear of the unknown. As a person with Parkinsons, you may worry about having hallucinations and/or delusions and not being able to do anything about it. As a care partner, you may worry that you wont be able to help your person with Parkinsons feel safe if something does happen.
The good news is you now have information on what Parkinsons disease psychosis is the risk factors to look out for biological and environmental triggers that can bring them on and how to manage them if they show up.
But what about the emotional toll these types of symptoms can place on you over the long-term as the person with Parkinsons or as a care partner?
The diagnosis of a chronic illness in and of itself requires a lot of adjustments. When you add something like Parkinsons disease psychosis into the mix, its important that you also add another level of self-care to your everyday life.
Don’t Miss: Parkinson’s Disease Causes Symptoms And Treatment
How Is Psychosis Managed
The urgency of treatment will depend on the type and characteristics of psychosis. Sometimes, when the hallucinations are mild and benign, and insight is retained, it is best that the Parkinson regimen be kept as is. However, when a patient is experiencing more threatening paranoid delusions, then more aggressive treatment is warranted .
The management of psychosis includes:
- Follow us on or on .
Psychosis: A Mind Guide To Parkinsons
Can be downloaded as a PDF or ordered the Parkinson’s Foundation online store. This 40-page booklet is a thorough guide to all aspects of Parkinsons psychosis, including symptoms, causes, treatment options, coping strategies for both the family and person experiencing the psychosis, and a chapter on tips for caregivers.
You May Like: Does Parkinson’s Affect Your Voice
Diagnosis And Treatment Of Hallucinations
First, your doctor needs to find out what’s causing your hallucinations. They’ll ask about your medical history and do a physical exam. Then they’ll ask about your symptoms.
They may need to do tests to help figure out the problem. For instance, an EEG, or electroencephalogram, checks for unusual patterns of electrical activity in your brain. It could show if your hallucinations are due to seizures.
You might get an MRI, or magnetic resonance imaging, which uses powerful magnets and radio waves to make pictures of the inside of your body. It can find out if a brain tumor or something else, like an area that’s had a small stroke, could be to blame.
Your doctor will treat the condition that’s causing the hallucinations. This can include things like:
- Medication for schizophrenia or dementias like Alzheimer’s disease
- Antiseizure drugs to treat epilepsy
Olfactory Tactile And Gustatory Hallucinations
People with Parkinsons disease can also experience olfactory , tactile , and gustatory hallucinations. These types of hallucinations are less common than visual and auditory hallucinations.
Smelling cigarette smoke is an olfactory hallucination several members of MyParkinsonsTeam describe:
- I have, over the past few months, been having the issue of smelling smoke occasionally when there is none. Its subtle and will last for about an hour.
- I can smell cigarette smoke smelled it all day today and there is no one anywhere who smokes.
- Its nice to hear I’m not alone in this. Its just my hubby and me and neither of us smoke, nor does anyone we know, unless my cat is secretly lighting one up without my knowledge. LOL!
Also Check: Does Amy Klobuchar Have Parkinson’s
How Commonly Do Parkinsons Disease Patients Develop Psychosis
Psychosis in Parkinsons disease generally comes in two forms: hallucinations or delusions . When hallucinations occur, they are mostly visual . Sometimes, they can be threatening, but this is less common. Auditory hallucinations are rare in Parkinsons disease and if they do occur, they are usually accompanied by visual hallucinations.
Delusions are usually of a common theme, typically of spousal infidelity. Other themes are often paranoid in nature Because they are paranoid in nature, they can be more threatening and more immediate action is often necessary, compared to visual hallucinations . It is not uncommon that patients actually call 9-1-1 or the police to report a burglary or a plot to hurt them.
Unfortunately, psychosis occurs in up to 40% of Parkinsons disease patients . In the early stage of Parkinsons disease psychosis, the patient often still has a clear understanding and retains their insight, but this tends to worsen over time and insight may eventually be lost. At later stages, patients may be confused and have impaired reality testing that is, they are unable to distinguish personal, subjective experiences from the reality of the external world. Psychosis in Parkinsons disease patients frequently occurs initially in the evening, then later on spills into the rest of the day.