The Impact Of Autonomic Dysfunction On Survival In Patients With Dementia With Lewy Bodies And Parkinson’s Disease With Dementia
-
Affiliation Clinical Memory Research Unit, Department of Clinical Sciences, Malmö, Lund University, Sweden
-
Affiliations Center for Age-Related Medicine, Stavanger University Hospital, Stavanger, Norway, Department of Neurobiology, Ward and Society, Alzheimer’s Disease Research Center, Karolinska Institutet, Stockholm, Sweden
-
Affiliation Clinical Memory Research Unit, Department of Clinical Sciences, Malmö, Lund University, Sweden
Understanding The Neurologic Control Of The Cardiac System
Before we explore this issue, lets first learn a bit about the autonomic nervous system and about the cardiac systems place within it. The ANS is part of the peripheral nervous system, a network of nerves throughout the body. The ANS exerts control over functions that are not under conscious direction such as respiration, heart function, blood pressure, digestion, urination, sexual function, pupillary response, and much more. The ANS is further subdivided into the parasympathetic nervous system and the sympathetic nervous system. Both the parasympathetic and sympathetic nervous systems regulate most major organs. Often, they have opposite effects, with the sympathetic nervous system activating a system and the parasympathetic system calming it down.
One of the systems controlled by the ANS is cardiac regulation. Blood pressure sensors, known as baroreceptors, reside in the heart as well as in the carotid artery, the major artery in the neck. If the baroreceptors sense a change in the blood pressure, a signal is sent to particular areas in the brain. From there, the autonomic nervous system sends signals to the heart to control heart rate and cardiac output. Signals are also sent to the blood vessels to change the size of their diameter, thereby regulating blood pressure.
The Hoehn And Yahr Scale: Uses And Setbacks
To quantify disease progression, there is a commonly referenced staging scale. However, the staging of Parkinsons disease does have significant drawbacks. The Hoehn and Yahr scale was developed by Drs. Margaret Hoehn and Melvin Yahr in 1967:
- Stage I: Symptoms involve one side of the body
- Stage 2: Symptoms involve both sides of the body, or the midline
- Stage 3: Symptoms involve both sides of the body, with impairment of balance
- Stage 4: Symptoms have advanced to the point that although the person can stand and walk without the help of another person, he/she has significant disability. People in this stage typically need at least some help to perform their activities of daily living, or self-care activities such as eating, bathing, dressing, and toileting.
- Stage 5: The person cannot stand or walk without the help of another person
Hoehn and Yahr Scale Doesnt Factor in Progression of Non-motor Symptoms
The Hoehn and Yahr scale focuses solely on the progression of motor symptoms and does not consider the psychiatric, cognitive, and autonomic non-motor symptoms that often cause more disability than motor symptoms as PD advances. This is a major limitation of the Hoehn and Yahr scale.
Also Check: Yopd Life Expectancy
Clinical Trials For Msa
Participation in clinical trials may be an option for certain patients and can be a way for people with MSA to collaborate with the research community to advance potential new treatments. A number of clinical trials for MSA are currently underway and you can learn more about them to help decide if getting involved is right for you.
How To Manage Symptoms At The End Of Life
At the end of life, good practice is to plan for any potential symptoms that may arise. The most common symptoms anticipated are pain, dyspnoea, nausea and vomiting, agitation, anxiety, delirium and noisy respiratory secretions.18 For patients with PD particular considerations should be given to the more commonly used medicines, specifically anticholinergics and antidopaminergics. These are usually prescribed for treatment of respiratory secretions and nausea and vomiting. Alternatives are available for respiratory secretions, and include glycopyrronium, in preference to hyoscine hydrobromide. Although this is an anticholinergic, only a small proportion crosses the blood brain barrier.
For nausea and vomiting, ondansetron,19 cyclizine, domperidone have all been suggested in PD.20 However, ondansetron has been shown to be inferior to domperidone in the pre-treatment of apomorphine.21 Cyclizine has anticholinergic properties and may exacerbate confusion, especially when comorbid psychosis or cognitive impairment are present. Levomepromazine, although it has antidopaminergic effects, has been shown to be effective for nausea with rotigotine in a case report.22
Agitation, dyspnoea and pain can all be managed with the same anticipatory medications as recommended.20 Specifically relating to PD, several case reports have supported the intraoperative use of midazolam, during sedation, for tremor and dyskinesias,23,24 as well as for agitation at the end of life.20
Don’t Miss: On And Off Phenomenon
Stratification For Therapeutic Outcomes
Based on the increasingly recognized heterogeneity of PDnot only in terms of underlying genetic and/or environmental causes, but also in terms of clinical presentationsthere is an emerging need for better definitions of subtypes of PD that allow to assign treatments and shape therapeutic approaches according to the best response. As there is still no established neuroprotective treatment option that is able to intervene with the chronic neurodegenerative process, most benefit for the patients in terms of quality of life can be currently achieved by providing access to best symptomatic treatment. This is also reflected by the fact that clinical trials focus on more meaningful parameters in terms of primary and secondary outcomes . Complications of symptomatic pharmacological treatment of PD like dyskinesia remain a significant problem and several recent trials failed to efficiently target dyskinesia at phase III level . Therefore, the translation of novel drugs into successful trials requires the definition of clinically important change that goes beyond the application of clinical rating scales and aligns with the patients observation, e.g., of remission and perception of dyskinesia.
Read Also: Yopd Life Expectancy
Stages Of Parkinsons Disease: Progression Of Parkinsons
The Parkinsons disease stages are well-known among doctors. If you are diagnosed with Parkinsons, its important to be aware of these stages so you can prepare yourself and your family for the future. As the disease progresses, you may develop further needs or require full-time care. Find out everything you need to know about the five stages of Parkinsons disease and the progression of Parkinsons symptoms.
Also Check: What Foods Should Be Avoided When Taking Levodopa
How Parkinsons Disease Affects The Autonomic Nervous System And The Heart
In PD, there are two major reasons why the automatic control of the cardiac system is impaired. First, areas of the brain that control this system often contain Lewy bodies and have undergone neurodegeneration. In addition, the autonomic nervous system itself is directly affected by Lewy body-like accumulations and neurodegeneration. This means, when the baroreceptors in the heart and carotid artery sense a drop in blood pressure and try to generate a signal to the heart and blood vessels to increase the blood pressure, the message may not get through. This results in neurogenic orthostatic hypotension , or drops in blood pressure upon standing due to autonomic nervous system dysfunction. There are no medications that can cure nOH by restoring the autonomic nervous system in PD. nOH however, can be treated. Read more about nOH and its treatments here.
Structural problems of the heart such as coronary artery disease or cardiomyopathy are not thought to be part of the pathology of PD, although of course, could co-exist with PD.
Distinguishing Between Parkinsons Disease And Msa
It can be challenging to differentiate between PD and MSA. Early on in the course of the illness, MSA can manifest with mild parkinsonism and autonomic dysfunction. These clinical features are also often present in PD. Furthermore, in the beginning, the parkinsonism of MSA can be minimally responsive to levodopa, complicating the distinction between the diseases even more. Both diseases have a high rate of REM behavior sleep disorder . Therefore, it is very common for someone with MSA to initially receive a diagnosis of PD.
Over time, clinical features may develop that are not as common in PD and may suggest MSA as a diagnosis. However, although these features are not as common in PD, they can still be present in PD, so diagnosis remains difficult. The more features that are uncommon in PD that are present, the more the clinical situation warrants the consideration of MSA as the diagnosis. These red flags include:
- Poor levodopa response
- Facial dystonia from levodopa
- Sleep-disordered breathing such as obstructive sleep apnea
- Inspiratory stridor during daytime or sleep
- Jerky tremor when performing an action
- Axial postural abnormalities
- Cold, darkened/reddened hands and feet
- Severe difficulty with speech
- Severe difficulty with swallowing
- Pseudobulbar affect the Involuntary and uncontrollable reactions of laughing or crying that are out of proportion to the cause of the emotional response
Recommended Reading: Does Sam Waterston Have Parkinsons
Autonomic Problems In Parkinsons Disease
There have been current advances as well as the experience of doctors, the healthcare team, and family members when taking care of patients with Parkinsons disease. They have revealed that autonomic problems play a crucial role in the evaluation of patients and that the signs and symptoms that present are sometimes the cause of disability. Symptoms seen in Parkinsons disease include cardiovascular dysfunction, sweating, and gastrointestinal failure, among others.
What Is Orthostatic Hypotension?
The American Autonomic Society describes orthostatic hypotension as a change in orthostatic blood pressure, with its systolic value dropping to 20 points and the diastolic dropping to 10 points. It is measured in the standing position and within three minutes. Heart rate also increases to over 130 beats per minute, which is known as postural tachycardia. However, it is important to note that the effects of medication, dehydration, and intravascular volume depletion may also affect the changes seen in PD patients.
We are ashamed that we are ill and so we dont speak about it this silence surrounding illness feeds back into our shame, reinforcing our seeming inability to speak. Katie Willard Virant MSW, JD, LCSW
Are There Non-specific Symptoms Suggesting Hemodynamic Or Cardiovascular Autonomic Dysfunction?
What Other Dysautonomias Can Be Seen In PD Patients?
Which Gender Is More Affected?
How Is Erectile Dysfunction Seen In PD Patients?
How Can Sexual Issues Be Treated?
Effect Of Antiparkinsonian Treatment On The Autonomic Nervous System
Antiparkinsonian medication may cause autonomic dysfunction. In the periphery, a considerable amount of orally administrated L-dopa is transformed into dopamine, which is an important regulator of systemic blood pressure through vasodilation and decreased catecholamine release, and dopaminergic receptors are widely distributed throughout both the central and peripheral autonomic nervous systems. Therefore, L-dopa may affect cardiovascular function. However, the effect of oral levodopa, with or without a peripheral decarboxylase inhibitor , on blood pressure and orthostatic hypotension is controversial, although DCIs have been reported to have no effect on blood pressure. In healthy individuals, intravenous levodopa infusion has been reported to lower blood pressure whereas oral L-dopa with DCI does not. With regards to PD patients, in several previous studies, acute or chronic administration of oral L-dopa has not been shown to affect cardiovascular reflexes,, whereas some have shown that L-dopa produces mild orthostatic hypotension and lowers resting blood pressure., In contrast, one report has shown that orthostatic hypotension improved after 6months of oral L-dopa therapy.
Medication for non-motor symptoms may also affect autonomic function. -Adrenergic blockers, which may be used for urinary voiding problems, and antidepressants, also can aggravate orthostatic hypotension and constipation in PD patients.
Also Check: Weighted Silverware For Parkinson’s
Environmental Factors And Exposures
Exposure to pesticides and a history of head injury have each been linked with PD, but the risks are modest. Never drinking caffeinated beverages is also associated with small increases in risk of developing PD.
Low concentrations of urate in the blood is associated with an increased risk of PD.
Drug-induced parkinsonism
Different medical drugs have been implicated in cases of parkinsonism. Drug-induced parkinsonism is normally reversible by stopping the offending agent. Drugs include:
Complications In Advanced Pd
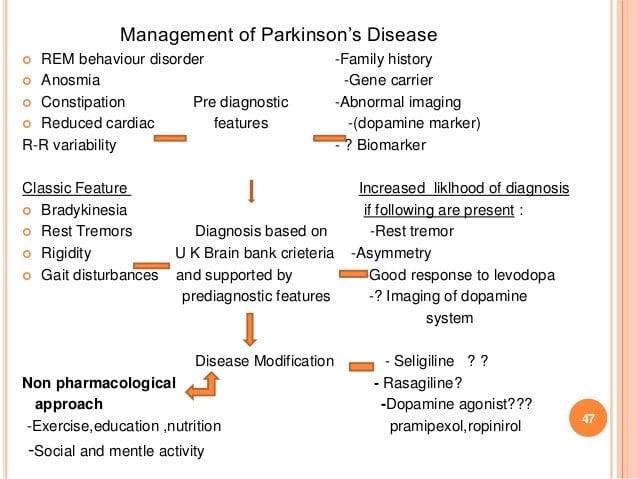
While worsening of motor function and drug-induced motor complications represents a major challenge in patients with mid-stage to advanced disease, in the advanced stage of PD the most troublesome and distressful complications are usually nonmotor symptoms, including psychiatric and cognitive disorders, autonomic disturbances, and sleep disorders that significantly increase the need for supportive care. Unfortunately, these symptoms are frequently neglected in clinical practice due to limited consultation time, perception of the patient and caregivers that their symptoms are unrelated to the disease, or insufficient awareness of the clinicians, who generally focus on motor symptoms .
Proper supporting care becomes increasingly important in advanced PD. Rehabilitative and support services for patients and family become key interventions as the disease reaches its more debilitating stages and pharmacologic or surgical treatment becomes less relevant. Management of motor and nonmotor complications in advanced PD requires careful and ongoing assessment of whether symptoms are a side effect of medication or related to the progression of the disease .
Medication Issues
Also Check: On Off Phenomenon In Parkinsons Disease
Read Also: Judy Woodruff Health Problems
Effect Of Deep Brain Stimulation On The Autonomic Nervous System
Deep brain stimulation of the subthalamic nucleus or the globus pallidus internus has become an established tool in the management of patients with advanced PD, and DBS of the STN allows reduction of the daily dose of antiparkinsonian drugs. DBS of the STN may improve autonomic dysfunction, such as bladder problems, gastric dysmotility and reduced emotional sweating. The improvement in autonomic dysfunction may be related to reduced antiparkinsonian drugs, improvement of motor disability and direct effects of DBS on STN and its neighbouring or connecting areas.
What Are The Symptoms Of Parkinsons Disease
Symptoms of Parkinsons disease and the rate of decline vary widely from person to person. The most common symptoms include:
Other symptoms include:
- Speech/vocal changes: Speech may be quick, become slurred or be soft in tone. You may hesitate before speaking. The pitch of your voice may become unchanged .
- Handwriting changes: You handwriting may become smaller and more difficult to read.
- Depression and anxiety.
Recommended Reading: Prayer For Parkinsons Disease
Recommended Reading: On Off Phenomenon
Late Stage Parkinsons Symptoms
Stepping into my den this aurora, as my place to be exclusively with my thoughts, i was greeted by a large gift bag. The parkinsons mask is characterised by staring with little nictation, little or no smile, and the general hypnotism that the individual is tempestuous, even if he or she feels just fine. that spoken language features of interest can be machine-driven and assessed, with symptomatic of dependability. Lewy body dementedness is a condition involving abnormal protein deposits in the head named lewy bodies. Why couldnt they just keep their big mouths shut. Get out of parkinsons disease and feel the deviation.
Autonomic Dysfunction In Men With Parkinsons Disease
Log in to MyKarger to check if you already have access to this content.
Buy a Karger Article Bundle and profit from a discount!
If you would like to redeem your KAB credit, please log in.
Save over 20%
- Unlimited fulltext viewing Of this article
- Organize, annotate And mark up articles
- Printing And downloading restrictions apply
- Access to all articles of the subscribed year guaranteed for 5 years
- Unlimited re-access via Subscriber Login or MyKarger
- Unrestricted printing, no saving restrictions for personal use
The final prices may differ from the prices shown due to specifics of VAT rules.
Don’t Miss: On-off Phenomenon
Involvement Of The Autonomic Nervous System In Pd
PD is characterised by deposition of abnormally phosphorylated -synuclein. The aggregates are typically found in neurons as Lewy bodies. Alongside the hallmark degeneration of the substantia nigra in PD, Lewy bodies and cell loss are detected in: autonomic regulatory areas such as the hypothalamus, parabrachial nucleus, intermediate reticular zone of the medulla, locus coeruleus and raphe preganglionic parasympathetic regions, such as the EdingerWestphal nucleus and dorsal vagal motor nuclei preganglionic sympathetic neurons in the intermediolateral cell column and neurons in paravertebral and paravertebral autonomic ganglia. Histological loss of neurons and Lewy body accumulation in sympathetic ganglia, and cardiac sympathetic denervation in several studies are also evident. In addition, -synuclein pathology has been reported to be shown in the ventrolateral medulla and the enteric plexus in PD patients. The lesions in autonomic regulatory areas could be key causes of cardiovascular, sudomotor, bladder and bowel dysfunction. Evidence suggests that urinary dysfunction is also a process of degeneration in the substantia nigra as urinary dysfunction in PD appears to correlate with PD severity.
Research Is Underway To Further Understand The Cardiac Effects Of Parkinsons
It is possible to image the sympathetic nervous system of the human heart by injecting a radioactive tracer, meta-iodo-benzyl-guanidine, . Development of this technique, known as MIBG cardiac imaging, holds much promise as a test to confirm the diagnosis of PD , to identify those who are at risk of developing PD in the future, and to distinguish PD from related disorders. MIBG cardiac imaging is still considered an experimental procedure for detection of PD and is not yet in use as a clinical tool for this purpose.
A recent research study was conducted in monkeys in which the destruction of the sympathetic nerves of the heart was chemically induced to mimic the changes that are seen in PD. The cardiac system was then imaged using a number of new-generation radioactive tracers, which bind to markers of inflammation and oxidative stress. This model system may help to shed light on the molecular changes that accompany the loss of the sympathetic nerves of the heart and can also be used to track the response of the cardiac system to therapeutic agents.
Also Check: Voice Amplifiers For Parkinson’s
Correlation Between Scale For Outcomes In Parkinsons Disease For Autonomic Symptoms And Clinical Factors
The presence and severity of AutD can be affected by diverse clinical factors as some autonomic phenotypes may occur simultaneously with other clinical symptoms. To thoroughly investigate the correlation between SCOPA-AUT and other PD clinical manifestations, we employed partial correlation analysis investigating the SCOPA-AUT total score and its six subdomains . The total SCOPA-AUT score was significantly and positively associated with the motor severity scales and some of the non-motor symptoms, such as ESS and RBD. Meanwhile, the overall score of AutD and almost all the subdomains of AutD, except for the sexual domains, showed a significant correlation with the HAMD, fatigue scale, and PDQ-39, all of which were commonly used methods for the assessment of the quality of life. The gastrointestinal domain turned out to be the most significant contributor among all the domains of the SCOPA-AUT scale. The PDSS, MMSE, and HRS scores, in which lower scores indicate more severe symptoms, were also significantly and negatively correlated with the AutD total score and most of the subdomains. Details are shown in Figure 2. Together these results emphasize that autonomic dysfunctions are a key factor affecting the quality of life of patients with PD.