Two Areas In Which Parkinsons Disease May Bring About Death
I. Falls
PD patients are at an increased risk of falling and bad falls can lead to death. This usually occurs as a complication of a fall that requires hospitalization, particularly if it involves surgery. While most people do not fracture their hips when they fall, some do, and hip surgery, while routine, is still major surgery. It carries the risk of infection, delirium related to pain medications and anesthesia, heart failure, pneumonia, blood clots in the legs that then go to the lungs, and general weakness from immobility. Hip fractures are probably the main cause for death for those who fall, but people can fracture other bones and require surgery. They may fracture their ribs, which leads to reduced coughing, because of the pain, and an increased risk of lung infections . It is surprisingly uncommon for Parkinsons Disease patients to die from brain injuries related to falls, but it still may occur.
II. Pneumonia
PD patients also may develop pneumonias completely unrelated to difficulties with swallowing, just like their non-PD friends and relatives.
Surgery For People With Parkinsons Disease
Deep brain stimulation surgery is an option to treat Parkinsons disease symptoms, but it is not suitable for everyone. There are strict criteria and guidelines on who can be a candidate for surgery, and this is something that only your doctor and you can decide. Surgery may be considered early or late in the progression of Parkinsons. When performing deep-brain stimulation surgery, the surgeon places an electrode in the part of the brain most effected by Parkinsons disease. Electrical impulses are introduced to the brain, which has the effect of normalising the brains electrical activity reducing the symptoms of Parkinsons disease. The electrical impulse is introduced using a pacemaker-like device called a stimulator. Thalamotomy and pallidotomy are operations where the surgeon makes an incision on part of the brain. These surgeries aim to alleviate some forms of tremor or unusual movement, but they are rarely performed now.
Experience And Expertise In Diagnosis And Care
Parkinsonism is a shorthand description for body movements that have become slow, small, stiff, shaky, and unsteady. Most cases of Parkinsonism develop after age 50 and are caused by neurodegenerative diseases such as Parkinsons disease . Some Parkinsonisms are the result of strokes, medication side effects, or another neurological condition such as normal pressure hydrocephalus.
UT Southwesterns Movement Disorders team has extensive experience in evaluating and treating Parkinsonism, PD, and other related disorders. Our clinical programs provide patients with access to the latest treatment options and information about medications to manage symptoms, as well as other services as needed.
You May Like: Jet Fuel And Parkinson’s
How To Get Palliative Care
If you or a loved one is facing Parkinsons disease, ask your doctor for a referral to palliative carethe earlier the better.
Although living with Parkinsons disease is difficult, your burden may be easier when palliative care is involved. You can receive palliative care in the hospital, at an outpatient clinic and sometimes at home.
Be informed about your condition, its treatment and what you can expect. And if you have received a Parkinsons diagnosis, or if the burden of illness is growing, dont hesitate to ask for a palliative care referral to help you make sense of the situation. With the support of palliative care, you can help ensure that you achieve and sustain the highest quality of life possible.
For more information, visit GetPalliativeCare.org. Take our quiz to find out if palliative care is right for you. And find providers in your area by visiting our Palliative Care Provider Directory.
What Is The Prognosis And Life Expectancy For Parkinson’s Disease
The severity of Parkinson’s disease symptoms and signs vary greatly from person to person, and it is not possible to predict how quickly the disease will progress.
- Parkinson’s disease itself is not a fatal disease, and the average life expectancy is similar to that of people without the disease.
- Secondary complications, such as pneumonia, falling-related injuries, and choking can lead to death.
- Many treatment options can reduce some of the symptoms and prolong the quality of life.
Recommended Reading: What Is The First Symptoms Of Parkinson’s Disease
What Does Kill People With Parkinsons
While no one dies directly from Parkinsons, you may be asking yourself what does typically cause death in Parkinsons patients. The two of the biggest causes of death for people with Parkinsons are Falls and Pneumonia:
Falls Parkinsons patients are typically at an increased risk of falls due to postural instability and other symptoms of Parkinsons. This poses a great risk to those with PD because falls are the leading cause of injury-related deaths among those 65 years or older according to the CDC. It is important to take precautions to limit the risk of falling in your home. This can be done by wearing special grip socks to prevent slipping or installing handrails in high-risk areas like the shower or staircase. In addition, you should talk with your doctor about getting a physical therapy evaluation periodically to strengthen your balance reflexes and help you develop other strategies to keep you safe in the home.
Support For People With Parkinsons Disease
Early access to a multidisciplinary support team is important. These teams may include doctors, physiotherapists, occupational therapists, speech therapists, dietitians, social workers and specialist nurses. Members of the team assess the person with Parkinsons disease and identify potential difficulties and possible solutions.There are a limited number of multidisciplinary teams in Victoria that specialise in Parkinsons disease management. But generalist teams are becoming more aware of how to help people with Parkinsons disease.
Recommended Reading: Cuales Son Los Sintomas Del Parkinson
How To Manage Symptoms At The End Of Life
At the end of life, good practice is to plan for any potential symptoms that may arise. The most common symptoms anticipated are pain, dyspnoea, nausea and vomiting, agitation, anxiety, delirium and noisy respiratory secretions.18 For patients with PD particular considerations should be given to the more commonly used medicines, specifically anticholinergics and antidopaminergics. These are usually prescribed for treatment of respiratory secretions and nausea and vomiting. Alternatives are available for respiratory secretions, and include glycopyrronium, in preference to hyoscine hydrobromide. Although this is an anticholinergic, only a small proportion crosses the blood brain barrier.
For nausea and vomiting, ondansetron,19 cyclizine, domperidone have all been suggested in PD.20 However, ondansetron has been shown to be inferior to domperidone in the pre-treatment of apomorphine.21 Cyclizine has anticholinergic properties and may exacerbate confusion, especially when comorbid psychosis or cognitive impairment are present. Levomepromazine, although it has antidopaminergic effects, has been shown to be effective for nausea with rotigotine in a case report.22
Agitation, dyspnoea and pain can all be managed with the same anticipatory medications as recommended.20 Specifically relating to PD, several case reports have supported the intraoperative use of midazolam, during sedation, for tremor and dyskinesias,23,24 as well as for agitation at the end of life.20
What Makes Pd Hard To Predict
Parkinsonâs comes with two main buckets of possible symptoms. One affects your ability to move and leads to motor issues like tremors and rigid muscles. The other bucket has non-motor symptoms, like pain, loss of smell, and dementia.
You may not get all the symptoms. And you canât predict how bad theyâll be, or how fast theyâll get worse. One person may have slight tremors but severe dementia. Another might have major tremors but no issues with thinking or memory. And someone else may have severe symptoms all around.
On top of that, the drugs that treat Parkinsonâs work better for some people than others. All that adds up to a disease thatâs very hard to predict.
You May Like: Psilocybin And Parkinson’s Disease
What Are The Important Points Regarding Duodopa At The End Of Life
Duodopa is a continuous infusion of dopaminergic medication administered as a gel into the gut, pumped via a percutaneously inserted gastrostomy tube . There is a requirement for care of the stoma and PEG tube together with functioning of the pump by the patient or carer.41 It reduces the time in motor off periods in advanced PD and quality of life.42 There is evidence of effective treatment up until death from within a case series.43
What Are The Symptoms
PSP affects movement, control of walking and balance, speech, swallowing, eye movements and vision, mood and behavior, and thinking. The pattern of signs and symptoms can be quite different from person to person. The most frequent first symptom of PSP is a loss of balance while walking. Individuals may have abrupt and unexplained falls without loss of consciousness, a stiff and awkward gait, or slow movement.
As the disease progresses, most people will begin to develop a blurring of vision and problems controlling eye movement. These symptoms may include:
- Slow eye movements.
Read Also: Vibram Shoes For Parkinson’s Patients
Incidence Of Parkinsons Disease
Its estimated that approximately four people per 1,000 in Australia have Parkinsons disease, with the incidence increasing to one in 100 over the age of 60. In Australia, there are approximately 80,000 people living with Parkinsons disease, with one in five of these people being diagnosed before the age of 50. In Victoria, more than 2,225 people are newly diagnosed with Parkinsons every year.
Medicines For Parkinsons Disease
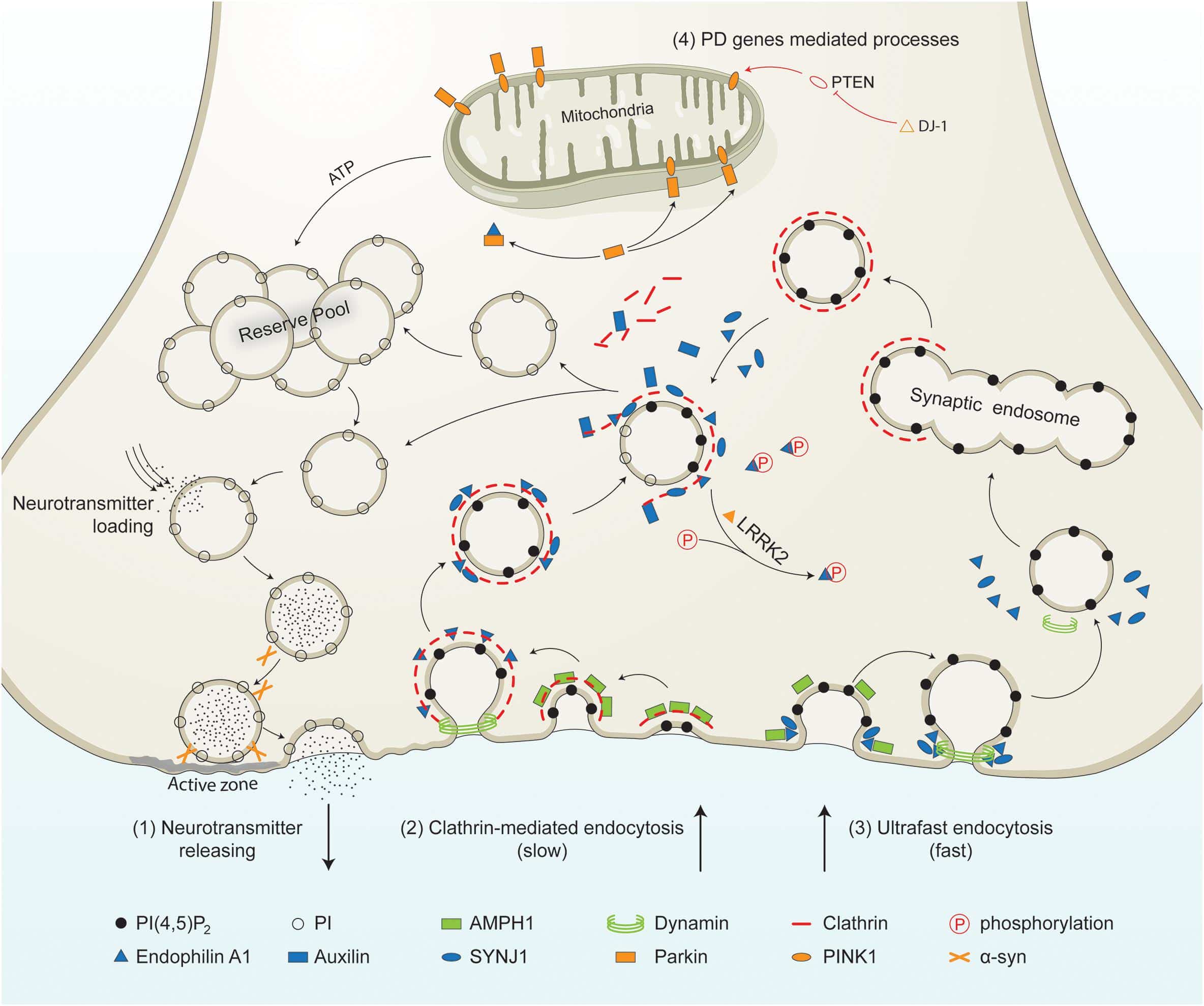
Medicines can help treat the symptoms of Parkinsons by:
- Increasing the level of dopamine in the brain
- Having an effect on other brain chemicals, such as neurotransmitters, which transfer information between brain cells
- Helping control non-movement symptoms
The main therapy for Parkinsons is levodopa. Nerve cells use levodopa to make dopamine to replenish the brains dwindling supply. Usually, people take levodopa along with another medication called carbidopa. Carbidopa prevents or reduces some of the side effects of levodopa therapy such as nausea, vomiting, low blood pressure, and restlessness and reduces the amount of levodopa needed to improve symptoms.
People living with Parkinsons disease should never stop taking levodopa without telling their doctor. Suddenly stopping the drug may have serious side effects, like being unable to move or having difficulty breathing.
The doctor may prescribe other medicines to treat Parkinsons symptoms, including:
- Dopamine agonists to stimulate the production of dopamine in the brain
- Enzyme inhibitors to increase the amount of dopamine by slowing down the enzymes that break down dopamine in the brain
- Amantadine to help reduce involuntary movements
- Anticholinergic drugs to reduce tremors and muscle rigidity
You May Like: What Diseases Are Similar To Parkinson’s
Can A Patients Ability To Make Decisions In The Last Days Of Life Be Impaired And How Is This Managed
In a North American study of 47 carers of idiopathic PD patients in the last months of life most described the goal of care as comfort, and almost half of the patients were described as unable to make any decisions in the last month of life. 10
When presenting, the patient may already be unable to communicate their symptoms and care preferences due to cognitive impairment and confusion. Also, there might be a physical difficulty in communication from severe rigidity. Care should be taken in considering the presence and consequent treatment of an intercurrent illness, and whether dopaminergic medication is exacerbating confusion due to hallucinations and/or psychosis.27
Continued attempts at verbal and non-verbal communication should be made throughout given the often fluctuating symptoms associated with PD and possible improvement in the intercurrent illness. In the absence of a next of kin or other person who is able to inform the clinical team, decisions should be made on a best interest basis as recommended in end of life care guidance.30
Hospice Eligibility For Parkinsons Disease
Due to the progressive nature of Parkinsons disease, it can be challenging for families to know when their loved one is eligible for the support of hospice care. If a loved one has been diagnosed with six months or less to live or if they have experienced a decline in their ability to move, speak, or participate in the activities of daily living without caregiver assistance, it is time to speak with a hospice professional about next steps.
Read Also: Best Edibles For Parkinson’s
Parkinson’s Disease Diet And Nutrition
Maintaining Your Weight With Parkinson’s Disease
Malnutrition and weight maintenance is often an issue for people with Parkinson’s disease. Here are some tips to help you maintain a healthy weight.
- Weigh yourself once or twice a week, unless your doctor recommends weighing yourself often. If you are taking diuretics or steroids, such as prednisone, you should weigh yourself daily.
- If you have an unexplained weight gain or loss , contact your doctor. He or she may want to modify your food or fluid intake to help manage your condition.
- Avoid low-fat or low-calorie products. . Use whole milk, whole milk cheese, and yogurt.
Myth : Aside From Medication There Isnt Much You Can Do
Fact: This it is what it is theres nothing I can do to help myself myth is counterproductive. There is a lot you can do chiefly, keeping as active as you can. A recent study found that patients with Parkinsons who took part in weekly, hourlong exercise sessions were able to do more in their daily lives than those who did not.
Recommended Reading: Parkinson’s And Immune System
Conditions That Mimic Shuffling Gait Seen In Parkinsons:
Please read the article on shuffling gait. It describes 5 causes of shuffling of gait.
The most crucial mimic to remember is Normal Pressure Hydrocephalus .
The person with NPH feels like he is stuck to the ground. This is a magnetic gait. It is easy to mistake this for Parkinsons disease.
For example, see this video posted by the Hydrocephalus Association of America on youtube:
NPH can be treated by implanting a small shunt pipe. This shunt drains excess water around the brain into the abdomen.
Read Also: Non Shaking Parkinsons Disease
Palliative Care As An Option
If your loved one is not eligible for hospice, the good news is that they can still receive palliative care. This type of care focuses on alleviating symptoms, discomfort, and stress associated with any illness, including PD.
The main difference between palliative care and hospice is that palliative care can be given along with standard treatments, including therapies intended to prolong life.
Recommended Reading: Parkinson’s Disease Linked To Pesticides
Palliative Care Management Of Non
Patients with PD can develop non-motor manifestations, categorized into autonomic dysfunction, cognitive impairment, neuropsychiatric disorders, and sleep disturbances. At the end-stage of PD, non-motor symptoms become more common and can become the most prominent medical problem, leading to increasing decline in quality of life both for patient as well as increasing caregiver burden . Non-motor symptoms occur in up to 50% of PD patients especially in association with the medication off state and may become worse by anti-PD medications . Almost one third of patients reports their non-motor symptoms to be at least as debilitating as their motor symptoms .
All patients with motor fluctuations face at least one non-motor problem during the off phase . In end-stage of PD, dementia, psychosis, and falls become more complex to manage than the motor complications as a result, managing non-motor aspects is important to increase quality of life and decrease the burden of illness . Chaudhuri and co-workers, using a new 30-item non-motor symptom screening questionnaire , found noticeably high scores among PD patients for impaired taste/smell, impaired swallowing, weight loss, constipation, urinary urgency, forgetfulness, dribbling, sadness, hallucinations, anxiety, sexual dysfunction, falling, reduced concentration, daytime sleepiness, vivid dreams, and sweating .
Is Parkinsons Fatal
Can you die from Parkinsons disease? The simple answer to this question is no, Parkinsons is not fatal. However, many people have experiences of their loved one progressing and getting worse with their Parkinsons symptoms before passing away. So does Parkinsons play any role in death, and if not, why does it seem to many people who have lost loved ones that Parkinsons was the cause of their loved ones death?
Don’t Miss: Is Fatigue A Symptom Of Parkinson’s
What You Can Do
As of 2021, there is no definite cure for Parkinsons disease. There is also no definite known cause. Its likely due to a combination of an individuals susceptibility and environmental factors. Most cases of Parkinsons disease happen without a genetic link.
According to research published in 2012, only report having a family member with the disease. Many toxins are suspected and have been studied, but no single substance can be reliably linked to Parkinsons.
However, research is ongoing. Its estimated that
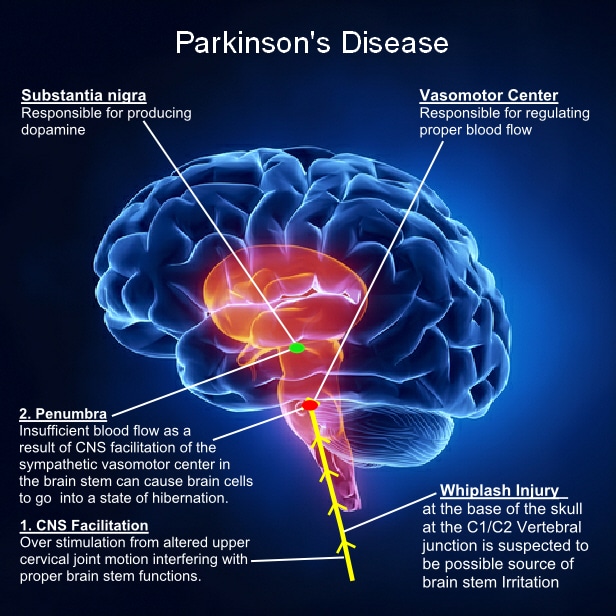
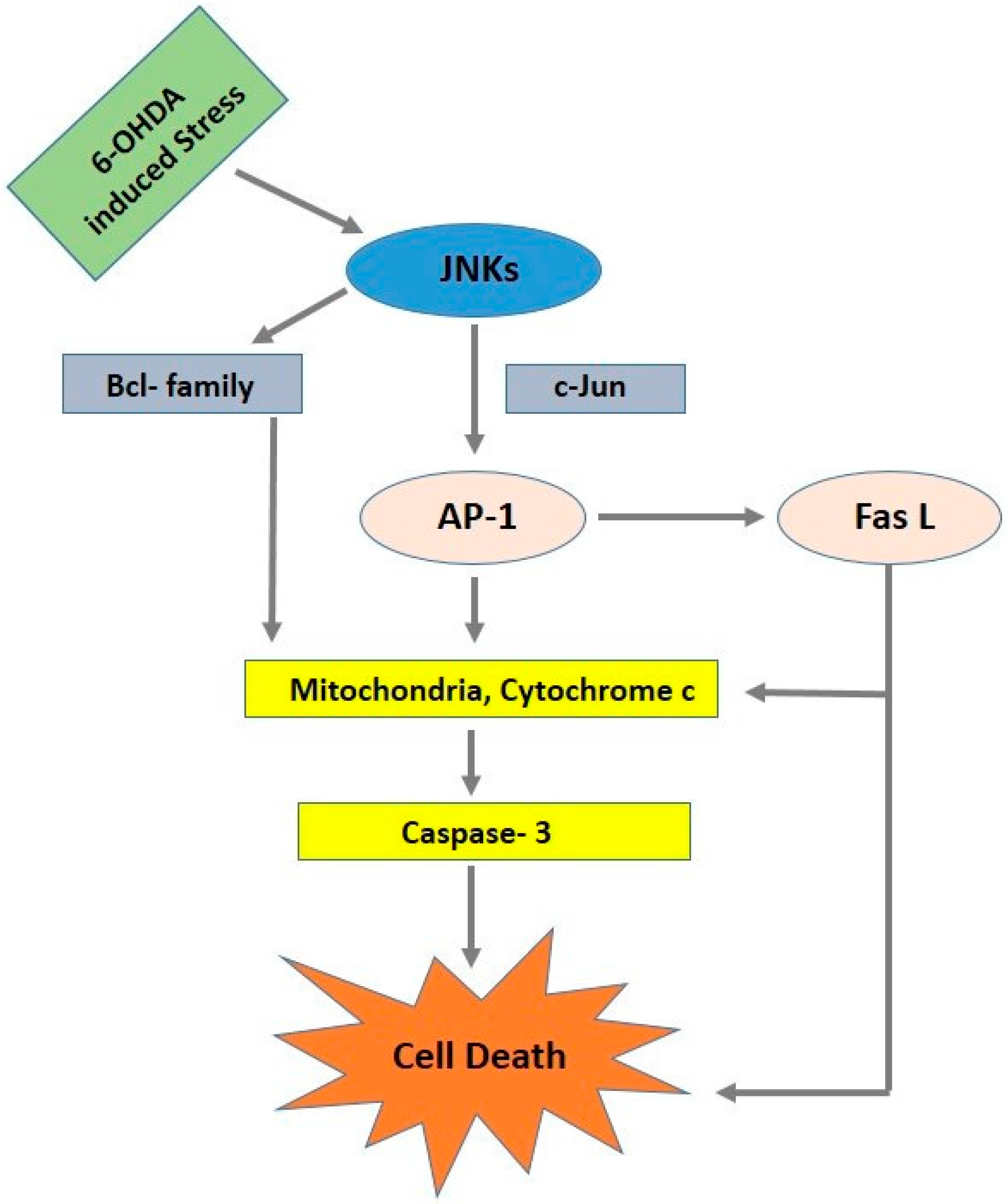
What Causes The Condition
First described in 1917 by James Parkinson as the shaking palsy, PD is characterized by a loss of neurons in the substantia nigra portion of the brain. A buildup of the protein alpha-synuclein causes dopamine producing cells to fail and die. There is no known specific cause of PD but it is considered to be a combination of genetic and environmental factors just like PSP.
Also Check: Boxers With Parkinson’s Disease
When To Seek Hospice Care
When you or your loved one have a life expectancy of six months or less, you become eligible for hospice care a type of comfort care provided at the end of life for someone living with end-stage Parkinsons disease. Hospice provides extra support so your loved one can live as comfortably as possible.
If you have experienced a significant decline in your ability to move, speak, or participate in activities of daily living without caregiver assistance, its time to speak with a hospice professional.
Read more: What is hospice care?
Some of the things that determine whether your loved one with end-stage Parkinsons is eligible for hospice include: difficulty breathing, bed bound, unintelligible speech, inability to eat or drink sufficiently, and/or complications including pneumonia or sepsis.
If you live in South Jersey, our nurse care coordinator can answer your questions and decide if your loved one is ready for hospice care. Call us 24/7 at 229-8183.