Showing Up As Your Best Self
Caring for someone with a progressive condition like Parkinsons disease can be challenging. Hallucinations only add to the stress of caregiving, especially if the person youre caring for doesnt have insight into what theyre experiencing.
The more you understand about your loved ones condition, the easier itll be to care for them. Talk to their doctor and read up on Parkinsons disease so youre better equipped to respond when hallucinations occur.
Dont forget to take care of yourself as well. Take regular breaks from caregiving to relax and do the things you enjoy. By tending to your own needs, youll have more energy to devote to your loved one.
Hallucinations According To The Duration Of The Disease
We found that the prevalence of hallucinations of all types and of visual hallucinations in the 3 months preceding inclusion in the study increased with the duration of the disease. Moreover, the duration of Parkinson’s disease was an independent predictor of visual hallucinations in the multivariate analysis. Other studies gave conflicting results on the relationship between hallucinations and disease duration. In a retrospective study of 100 patients, logistic regression analysis also showed an association between `psychosis’ and an increased duration of the disease . An association between the duration of the disease and the occurrence of hallucinations was also found by some investigators but not by others .
Table 1
Parkinsons Disease Psychosis: A Little
One of the lesser-known symptoms of Parkinsons Disease is Parkinsons psychosis. This webpage explains the prevalence, causes and symptoms, treatment options of PD psychosis. More useful to caregivers are sections on potential triggers of psychotic episodes and what caregivers can do about PD psychosis.
Read Also: Cleveland Clinic Parkinson’s Bicycle Study 2017
Risk Factors For Parkinsons Psychosis
Understanding the risk factors for hallucinations and delusions can help you recognize symptoms of Parkinsons psychosis. The following factors may increase the likelihood of experiencing hallucinations and delusions:
- Advancing cognitive impairment, including worsening memory loss
- History of depression
- Sleep disorders and sleep disturbances
- Changes to medications
- Worsening medical conditions outside of Parkinsons
We have noticed that when my father had delusions, it’s been when his general health is not good, or when he has been in the hospital for PD-related issues, a MyParkinsonsTeam member commented.
Questionnaires used in a clinical setting can help assess the risk of developing hallucinations or delusions, or establish that they are occuring. These include:
- PD nonmotor symptom scale
- Parkinson Psychosis Questionnaire
- Scale for Evaluation of Neuropsychiatric Disorders in Parkinsons Disease
Individuals with Parkinsons or their caregivers can speak with a neurologist to understand if any of these tools would be helpful in their particular situation.
Examples Of Delusions In Pd
- Jealousy
- Belief: Your partner is being unfaithful.
- Behavior: Paranoia, agitation, suspiciousness, aggression.
You May Like: On-off Phenomenon
Parkinson’s Disease Psychosis: The What When Why And How
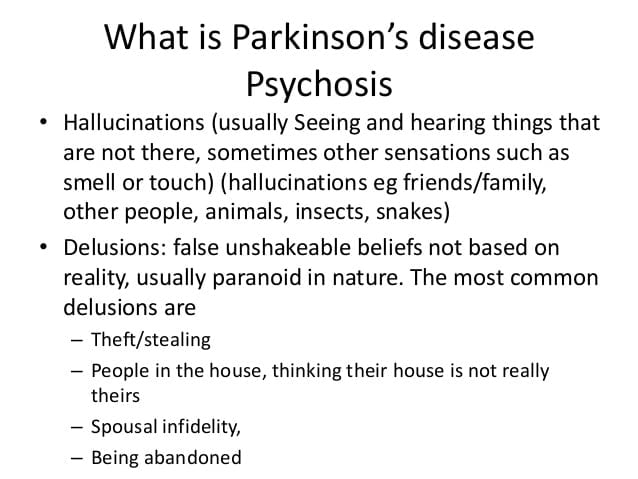
Psychosis is a psychiatric term used in neurology to refer to a spectrum of abnormalities. Parkinsons disease psychosis is where people experience hallucinations or delusions. Hallucinations is seeing, hearing, or smelling things that dont exist. With tactile hallucinations, one can feel a presence that isnt there. Delusions are believing something that is not true, like that a spouse is being unfaithful or caregivers are stealing. In this one-hour talk, movement disorder specialist Christopher Goetz, MD, focuses on hallucinations and spends a little time on delusions.
What Triggers Psychosis In Parkinsons Disease
Psychosis in Parkinsons disease is believed to be due to long term use of parkinsonian medications especially dopaminergic and anticholinergic drugs . However, significant medication exposure is no longer a pre-requisite in Parkinsons disease psychosis . The continuum hypothesis states that medication-induced psychiatric symptoms in Parkinsons disease starts with sleep disturbances accompanied by vivid dreams, and then develops into hallucinations and delusions, and ends in delirium. However this theory is now being challenged .
Read Also: On And Off Phenomenon
How Commonly Do Parkinsons Disease Patients Develop Psychosis
Psychosis in Parkinsons disease generally comes in two forms: hallucinations or delusions . When hallucinations occur, they are mostly visual . Sometimes, they can be threatening, but this is less common. Auditory hallucinations are rare in Parkinsons disease and if they do occur, they are usually accompanied by visual hallucinations.
Delusions are usually of a common theme, typically of spousal infidelity. Other themes are often paranoid in nature Because they are paranoid in nature, they can be more threatening and more immediate action is often necessary, compared to visual hallucinations . It is not uncommon that patients actually call 9-1-1 or the police to report a burglary or a plot to hurt them.
Unfortunately, psychosis occurs in up to 40% of Parkinsons disease patients . In the early stage of Parkinsons disease psychosis, the patient often still has a clear understanding and retains their insight, but this tends to worsen over time and insight may eventually be lost. At later stages, patients may be confused and have impaired reality testing that is, they are unable to distinguish personal, subjective experiences from the reality of the external world. Psychosis in Parkinsons disease patients frequently occurs initially in the evening, then later on spills into the rest of the day.
Bringing Light To Darker Side Of Parkinsons
Often the hardest part of Parkinsons disease psychosis is the fear of the unknown. As a person with Parkinsons, you may worry about having hallucinations and/or delusions and not being able to do anything about it. As a care partner, you may worry that you wont be able to help your person with Parkinsons feel safe if something does happen.
The good news is you now have information on what Parkinsons disease psychosis is the risk factors to look out for biological and environmental triggers that can bring them on and how to manage them if they show up.
But what about the emotional toll these types of symptoms can place on you over the long-term as the person with Parkinsons or as a care partner?
The diagnosis of a chronic illness in and of itself requires a lot of adjustments. When you add something like Parkinsons disease psychosis into the mix, its important that you also add another level of self-care to your everyday life.
You May Like: Pfnca Wellness Programs
What Is A Hallucination
A hallucination is a perception of something that does not actually exist. This may be visualised, heard, felt, smelled or tasted. Hallucinations are sometimes confused with illusions, which are distortions of a reality rather than something that is purely imagined – as with hallucinations.
Visual hallucinations: In Parkinson’s, hallucinations are most commonly visual and may be in black and white, in colour, still or moving. Often the images involve small animals and children. They may disappear quickly or may last for some time.
Auditory hallucinations: auditory hallucinations are less common. These generally involve hearing voices or other familiar sounds. Auditory hallucinations can also be part of a depressive symptomatology.
Tactile hallucinations: hallucinations may be tactile, that is, you may feel a sensation, like something touching you.
Smell and taste hallucinations: less commonly you may feel that you can taste something you havent eaten, or you may smell something that is not present, such as food cooking or smoke.
Usually hallucinations are not threatening or distressing. If you hallucinate you may be unaware that your perceptions are not real, and sometimes imagined images or sensations can be comforting. But hallucinations can also be distressing and you may feel threatened or frightened and may need reassurance and comfort from those around you.
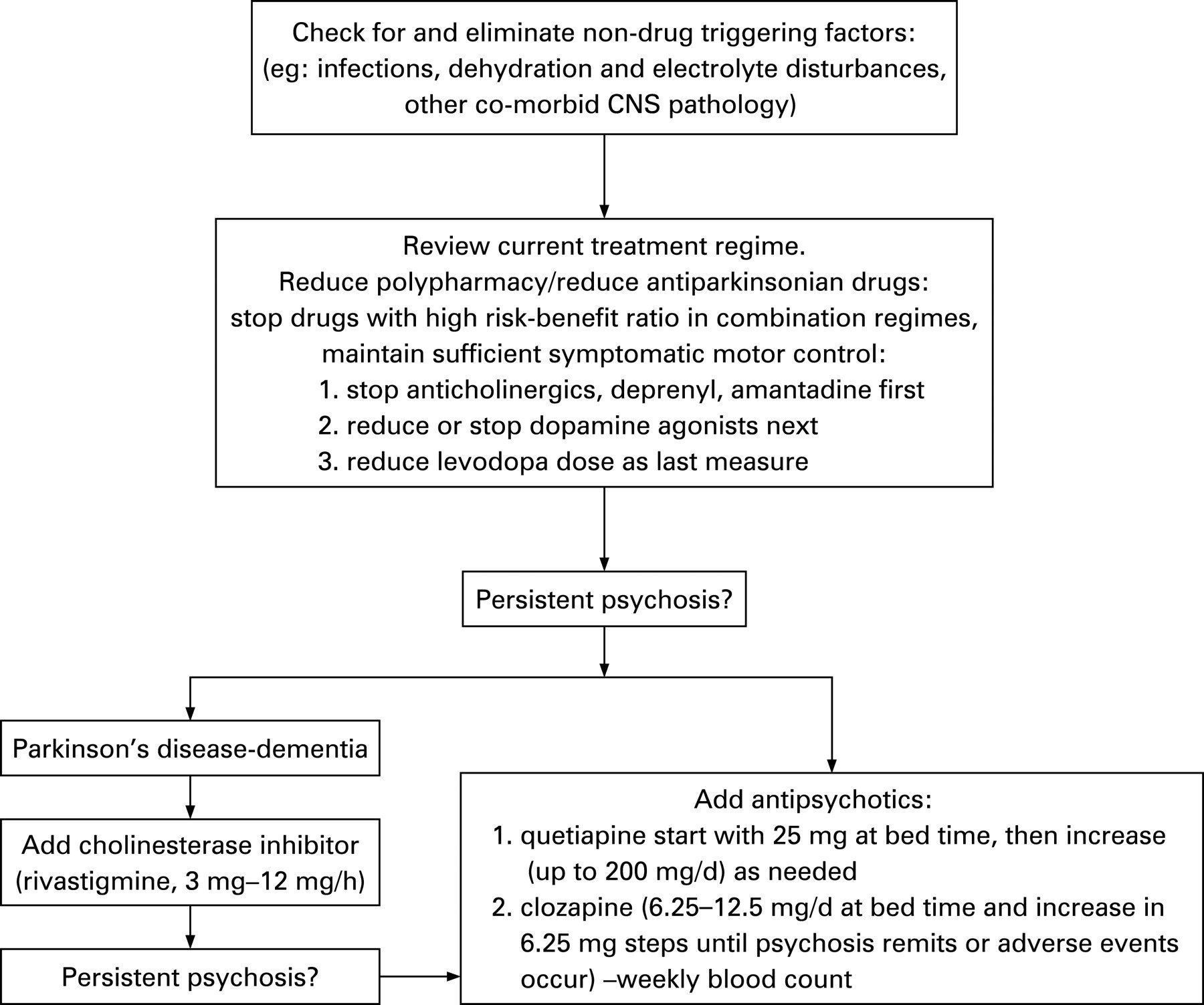
Treatment And Management Of Hallucinations
You should discuss any hallucinations or delusions with your doctor, or Parkinsons nurse if you have one, so that all treatment options can be considered.
In mild cases no specific action may be required and simple reassurance that the images, sensations or sounds are harmless may be all that is needed.
Read Also: Sam Waterston Tremor
How Common Are They
According to the Parkinsons Foundation, about 20% to 30% of people with PD experience psychosis, which includes visual hallucinations. At early stages , hallucinations may occur because of changes in the way the brain transmits information to the visual cortex, says Ritesh Ramdhani, M.D., a neurologist at Northwell Health in New York City. These hallucinations can change as the disease progresses, but they usually start as minor and not distressing.
Delusions From Parkinsons Disease
Delusions affect only about 8 percent of people living with PD. Delusions can be more complex than hallucinations. They may be more difficult to treat.
Delusions often start as confusion that develops into clear ideas that arent based on reality. Examples of the types of delusions people with PD experience include:
- Jealousy or possessiveness. The person believes someone in their life is being unfaithful or disloyal.
- Persecutory. They believe that someone is out to get them or harm them in some way.
- Somatic. They believe they have an injury or other medical problem.
- Guilt. The person with PD has feelings of guilt not based in real behaviors or actions.
- Mixed delusions. They experience multiple types of delusions.
Paranoia, jealousy, and persecution are the most commonly reported delusions. They can pose a safety risk to caregivers and to the person with PD themselves.
PD isnt fatal, though complications from the disease can contribute to a shorter expected life span.
Dementia and other psychosis symptoms like hallucinations and delusions do contribute to increased hospitalizations and increased rates of death .
One study from 2010 found that people with PD who experienced delusions, hallucinations, or other psychosis symptoms were about 50 percent more likely to die early than those without these symptoms.
But early prevention of the development of psychosis symptoms may help increase life expectancy in people with PD.
Also Check: Parkinson’s Hallucinations Commercial
How Can You Improve Aggressiveness And Hallucinations In Parkinsons
Hallucinations may spark anger or aggression in a person with Parkinsons disease. Some ways to help include:
- Reassure them, tell them they are safe.
- Speak slowly and calmly.
- Ask questions about the persons feelings.
- Listen to the person, dont interrupt.
- Avoid sudden movements.
- Give the person space and a way out, so they dont feel cornered or threatened.
- Make an emergency plan ahead of time for what you and others in the house will do if the person experiencing hallucinations becomes a danger to themselves, you, or anyone else.
- When it is safe, help the person speak with their healthcare provider about making a plan to address the hallucinations.
Hallucinations And Delusions In Parkinsons Disease
It might be surprising to learn that 20 to 30 percent of people with Parkinsons disease will experience visual hallucinations. While typically not a symptom of PD itself, they can develop as a result to a change in PD medication or as a symptom of an unrelated infection or illness. It is important to know the signs of hallucinations and how to manage them.
Hallucinations and other more severe perceptual changes can be distressing to family often more so than to the person experiencing them. For the well-being of people with PD and caregivers, it is important to identify hallucinations as early as possible and take steps to reduce them.
The following article is based on the latest research and a Parkinsons Foundation Expert Briefings about hallucinations and delusions in Parkinsons hosted by Christopher G. Goetz, MD, Professor of Neurological Sciences, Professor of Pharmacology at Rush University Medical Center, a Parkinsons Foundation Center of Excellence.
Read Also: Parkinson’s Bike Therapy
I Had A Hallucination: What Next
Research has shown that for many people with PD who have them, hallucinations begin after a change in medication, more specifically, an increase in levodopa . Additional factors make a person more likely to experience hallucinations when medications are changed, such as other cognitive problems or memory issues, depression and sleep problems. Dementia|A term used to describe a group of brain disorders that cause a broad complex of symptoms such as disorientation, confusion, memory loss, impaired judgment and alterations in mood and personality.] also increases the risk of hallucinations and delusions when PD medications are changed. Dementia means cognitive changes whether in memory, judgment or attention that interfere with daily life.
One thing that does not affect the risk of hallucinations is your regular dose of levodopa. Rather, studies show that it is a change in dose an increase in a dose that has been stable that sets off hallucinations.
Tip: Experiencing a hallucination does not mean you are going crazy. Many people recognize that their hallucinations are not real. Do not react to these visions or sounds or engage them dismiss them. Bring up the topic with your doctor immediately.
What Causes Psychosis In Parkinsons
Currently, there is not a clear understanding of the exact cause of Parkinsons disease psychosis, although certain brain chemicals and receptors are believed to play a role. In general, the condition is believed to be caused by either one of the following:
Side effect of dopamine therapy:
Although an exact causal relationship has not been established, some believe that this condition may be a side effect of dopaminergic therapy .2Dopaminergic therapy increases dopamine levels, helping improve motor symptoms in patients with Parkinsons disease. However, increasing dopamine levels can also cause chemical and physical changes in the brain that inadvertently lead to symptoms such as hallucinations or delusions.
Natural outcome of the disease:
This condition can be triggered by changes in the brain that occur regardless of taking dopamine enhancing medication. Some of these changes occur naturally as Parkinsons disease progresses.2
Also Check: Judy Woodruff Parkinson’s
Hallucinations And Rem Sleep Disorders In Parkinson’s Disease
At timestamp 1:58 in this recording of Thrive: HAPS 2020 Caregiver Conference, you will find a one hour talk by neurologist Joohi Jimenez-Shahed, MD. In it she delves into what REM sleep behavior disorder is and is not, and the distinctions between hallucinations, delusions, and delirium. Managment options for RBD and hallucinations are included.
What Is Parkinsons Disease Psychosis
Parkinsons disease psychosis is a non-motor symptom of Parkinsons disease that causes patients to experience hallucinations and/or delusions.More than half of all patients with Parkinsons disease eventually develop symptoms over the course of their disease.1
Diagnosing and treating this condition can be complex. The condition relates to both neurology and psychiatry . For this reason, Parkinsons disease psychosis is considered a neuropsychiatric condition, since it deals with mental health symptoms caused by a disease of the nervous system .
Introducing an easier way to track your symptoms and manage your care.
Dont want to download the app? Use the non-mobile version here.
Recommended Reading: Parkinson’s Double Vision
How To Talk To Someone With Hallucinations Or Delusions
- It is usually not helpful to argue with someone who is experiencing a hallucination or delusion. Avoid trying to reason. Keep calm and be reassuring.
- You can say you do not see what your loved one is seeing, but some people find it more calming to acknowledge what the person is seeing to reduce stress. For example, if the person sees a cat in the room, it may be best to say, “I will take the cat out” rather than argue that there is no cat.
Page reviewed by Dr. Chauncey Spears, Movement Disorders Fellow at the University of Florida, a Parkinsons Foundation Center of Excellence.
Network Changes And Thalamic Drivers
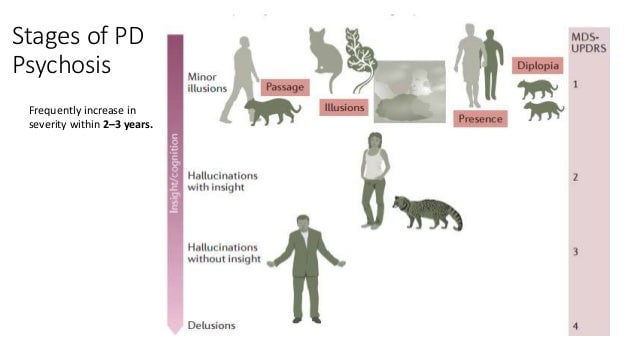
Visual hallucinations have fascinated neurologists and neuroscientists for many years, with their tantalisingly rich and often narrative detail. Due to their transient nature, they have been challenging to investigate, with no clear mechanism found, but many theories have been proposed. Previous models for visual hallucinations considered them as cortical release phenomena, where spontaneous activity occurs in the absence of visual stimuli. Alternative models suggested that hallucinations arise due to incorrect binding of objects into visual scenes.
Advances in computational modelling and network neuroscience have opened up approaches to understanding the brain in new ways. Recent models suggest that Parkinsons hallucinations could arise due to a shift in dominance of difference networks. Specifically, there is thought to be a breakdown in those networks directed to attention and perception, and overactivity of the default mode network ,, a large-scale network that becomes activated during rest, and in day dreaming and mind-wandering. Indeed abnormal levels of default mode network activation are seen in patients with Parkinsons hallucinations.
Adapted from Zarkali A, Adams RA, Psarras S, Leyland LA, Rees G, Weil RS. Increased weighting on prior knowledge in Lewy body-associated visual hallucinations. Brain Commun. 2019 1:fcz007. doi:10.1093/braincomms/fcz007
Recommended Reading: Sam Waterston Parkinson’s
Comparison Of Hallucinators And Non
The patients with isolated minor hallucinations were compared with the patients with no hallucinations . The only significant difference was a higher CES-D score in the group with minor hallucinations . When the presence of depression was determined using the cut-off values of the CES-D, depression was more frequent in the patients with minor hallucinations than in the patients without any hallucinations , but this difference did not reach significance.
The patients with formed visual hallucinations are compared with the non-hallucinators in Table 5. Patients with visual hallucinations differed in a number of respects: they were older, had a longer duration of disease, had a more severe motor state, had more depressive symptoms, and were more likely to have cognitive impairment, day-time somnolence and a history of ocular pathology. They were less likely to receive anticholinergics or selegiline and received a higher daily dose of levodopa, but the levodopa-equivalent dose did not differ significantly between the two groups. Visual hallucinations were recorded in 70% of the patients with dementia versus 10% of non-demented patients , and in 55% of the patients with severe cognitive disorders versus 8% of the patients with absent or moderate cognitive impairment .
The patients with hallucinations of any type were compared with the patients with no hallucinations. The results were identical to those of the preceding analysis, except for the degrees of significance .