If You Are Experiencing Sleep Problems You Should Avoid:
- Alcohol, caffeine and other stimulants such as nicotine
- Heavy late-night meals
- Heavy exercise within six hours of bedtime
- Thoughts or discussions before bedtime about topics that cause anxiety, anger or frustration
- Screen time television, phones, tablets one or two hours before bed.
Certain antidepressants, such as mirtazapine may help with sleep while others the SSRIs can make other sleep symptoms worse. Also, if you are unsure, check with your doctor or pharmacist to ensure alerting medications are being taken in the morning and sedating medications are being taken at night.
If urinary frequency keeps you up at night, be sure your doctor rules out causes other than PD. In addition, there are several medications that can be helpful, including oxybutynin , tolterodine , trospium , tofenacin succinate , darifenacin , mirabegron and phenoperidine fumarate . You may be referred to a bladder specialist .
A Cheaper Quicker Form Of Assessment
Unlike the usual method of assessing the risk of Parkinsons disease, which is called dopamine transporter imaging, the current assessment is inexpensive and easy to apply.
Dopamine transporter imaging, explain Dr. Postuma and colleagues, assesses the integrity of the dopaminergic system, which typically becomes compromised in parkinsonism and Parkinsons disease. However, this test is complex and costly. In contrast, assessing for the risk factors that the current study considers is both quick and cost efficient.
We confirmed a very high risk of in people with REM sleep disorder and found several strong predictors of this progression, notes Dr. Postuma.
As new disease-modifying treatments are being developed for and related diseases, these patients are ideal candidates for neuroprotective trials.
Dr. Ron Postuma
Getting Your Best Sleep With Parkinsons
This 1-hour webinar includes an interview of a person with Parkinsons disease, a movement disorders specialist, and a sleep sciences specialist. They discuss sleep disorders associated with Parkinsons disease, the difference between those that are a symptom the disease or a side-effect of medication, and how to treat them and live your best life with a sleep disorder.
Read Also: Parkinsonism Is Characterized By The Loss Of
You May Like: Parkinson’s Foundation Kansas City
What Are The Rem Sleep Disorder Treatments
Treatment for RBD typically involves a combination of preventative measures, safety measures, and medication that suppresses REM sleep, such as certain antidepressants or antipsychotics. These medications suppress muscle activity during REM sleep, allowing one to act out less frequently and potentially reduce the risk of injury. This suppression may also help alleviate other symptoms associated with REM sleep, such as EDS and memory loss.
Diagnosing And Treating Rbd
If you suspect that you or a loved one might have RBD, a movement disorder neurologist or a sleep physician should conduct an evaluation. The specialist might order a sleep study that would spot abnormal muscle movements during REM sleep. Hallucinations or waking up during a certain stage of sleep is different from REM sleep behavior disorder and might indicate a different condition.
If a diagnosis is confirmed, we recommend the following safety precautions:
-
Lower the bed if possible to prevent falls.
-
Pad the side rails if youre sleeping in a hospital bed.
-
Pad the floor around the bed.
-
Move nightstands away from the bed.
-
Move the bed away from walls or windows.
-
Sleep in separate beds or rooms if necessary .
-
Use a sleeping bag with a zipper to restrict arm and leg movements.
Read Also: Parkinson’s Stiffness In Morning
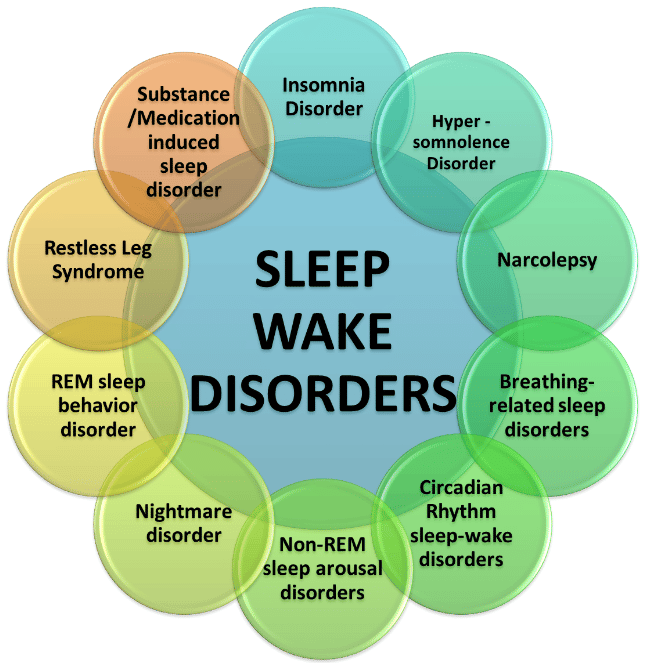
Which Condition Is Most Closely Associated With Rem Behavior Disorder
Parkinsons disease is most closely associated with REM Behavior Disorder. Some studies suggest that an early RBD diagnosis could be a significant predictor of the later development of Parkinson’s disease.
Other disorders most strongly associated with RBD include dementia with Lewy bodies, Narcolepsy, and multiple system atrophy.
Brain injuries could also contribute to the development of the disease.
Limit Lights In Your Room
Minimize your exposure to artificial lights when preparing for bed. Sleep in a cool, dark place. Avoid bright lights when sleeping. You could keep dim night lights if sleeping in complete darkness is uncomfortable.
Avoid watching television and using mobile devices before bed or lying in bed. These devices emit blue lights that could affect your sleeping habits.
Dont Miss: Social Security Disability Parkinsons
Also Check: How To Check If You Have Parkinson Disease
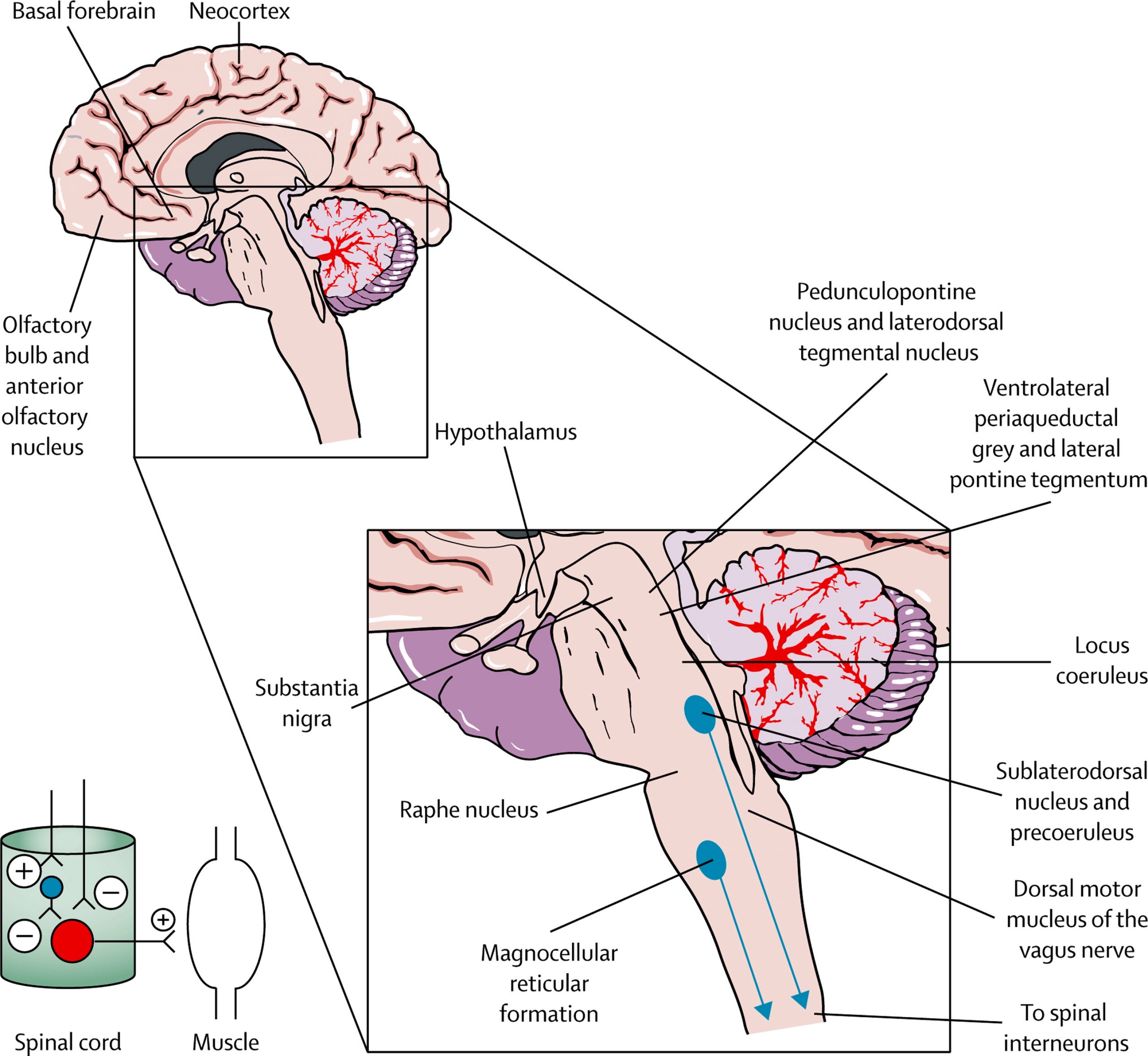
Causes Of Rem Sleep Disorder
The exact cause of RBD is unknown, but it may happen along with degenerative neurological conditions such as Parkinson’s disease, multisystem atrophy , and diffuse Lewy body dementia. In 55% of people, the cause is unknown, and in 45%, itâs linked with alcohol or sedative-hypnotic withdrawal, tricyclic antidepressant , or serotonin reuptake inhibitor use or other types of antidepressants .
RBD often happens several years before the development of these neurodegenerative diseases. In one study, 38% of people diagnosed with RBD developed Parkinson’s disease within an average of 12 to 13 years after RBD symptoms began. Also, RBD is seen in 69% of those with Parkinson’s disease and multisystem atrophy. The relationship between RBD and Parkinson disease is complex not everyone with RBD will develop Parkinson’s disease.
Show Sources
Possible Signs Of Rbd
- You experience dream enactment behaviors.
- Your loved one appears to be acting out their dreams.
- You or a loved one awakens to find that injuries or damage have been sustained during sleep.
In any of these cases, please consult your physician. The good news? RBD may be treated successfully with clonazepam and melatonin.
You may also wish to safety-proof your sleeping place by padding corners of furniture, installing a bed rail, and putting dangerous items out of easy reach.
Take heart, however not everyone who experiences RBD goes on to develop PD.
You May Like: Laser Cane For Parkinson’s
Sleep Disorders In Parkinsons Disease
In this 17-minute lecture Dr Gary Leo discuses sleep challenges caused by the neurochemical changes, medications and mood disturbances of Parkinsons disease, and normal changes of aging. He discusses possible causes and treatment options of sleep maintenance insomnia, REM Sleep Behavior Disorder, daytime sleepiness, sleep apnea, and restless leg syndrome, ending with some tips for good sleep.
Idiopathic Rapid Eye Movement Sleep Behavior Disorder
iRBD, which occurs without neurodegenerative disease, was first described in 1986, with similar phenomenological reports being presented in the 1970s. It is characterized by central nervous system dysfunction during sleep and wakefulness with cortical activity impairment, neuropsychological changes, and autonomic dysfunction1313. Fantini ML, Ferini-Strambi L, Montplaisir J. Idiopathic REM sleep behavior disorder: Toward a better nosologic definition. Neurology. 2005 Mar 64:780-6. https://doi.org/10.1212/01.WNL.0000152878.79429.00.
Also Check: Fitness Counts Parkinson’s Disease
Symptoms And Diagnostic Considerations
Rapid Eye Movement Sleep Behavior Disorder is a non-familial sleep disorder, characterized by the loss of the inherent muscle atonia observed during normal REM sleep. This phenomenon is often referred to as REM Sleep without Atonia . Whilst isolated RSWA is frequently an incidental finding in sleep studies, it forms the substrate of the dream enactment behavior which defines RBD. Here, individuals experience vivid dreams which they act out during sleep.
It is important to remember that dream enactment and limb movements during sleep can occur in the healthy population, often in the context of heightened emotional states . The same symptoms may also be experienced during withdrawal from sedatives or alcohol. In non-pathological dream enactment, individuals typically respond to dream content during the transition from REM sleep to the awake state and while maintaining REM atonia during much of the REM period. In contrast, RBD individuals will maintain REM sleep during and immediately after most of their dream enactments. As acute dream enactment is generally self-limiting, the chronicity of symptoms is a key distinguishing factor, and forms part of the diagnostic criteria for RBD .
Cortical Thinning At Baseline
The PD-pRBD group revealed a significant thinner cortex in the bilateral inferior temporal cortex compared with the PD-noRBD group . There were no group differences in volumes of subcortical structures . We did not find significant correlations between the mean thickness of the inferior temporal cortex and clinical variables at baseline.
Fig. 1: Cross-sectional cortical thickness differences.
PD patients with probable RBD revealed a significant thinner cortex in the bilateral inferior temporal cortex compared with the PD patients without RBD . The color scale bar shows the p-values. Lh, left hemisphere Rh, right hemisphere.
Don’t Miss: Food For Parkinson’s Disease
Somnolence And Excessive Daytime Sleepiness
Somnolence and EDS occur commonly in PD. Etiologies of somnolence in PD include reversal of the sleepwake cycle, the disease process itself, disrupted sleep due to a variety of motor and nonmotor causes, and the use of dopamine agonists and other antiparkinsonian medications. Several studies have found that dopamine agonists are more likely to cause somnolence than levodopa. The soporific effects of the commonly used dopamine agonists appear to be similar as assessed by Epworth Sleepiness Scale scores.36
EDS occurs in PD patients, and is usually associated with dopamine agonist use. EDS may occur with use of other PD medications, including levodopa/carbidopa. However, EDS as measured by the ESS does not always correspond to shortened sleep latency as quantified by the Multiple Sleep Latency Test .10 In addition, nocturnal sleep disturbance as measured by polysomnogram may not account for the severity of daytime sleepiness in PD patients with EDS.10
Recommended Reading: Reishi Mushroom Parkinsons Disease
Patients Depression Often Carries Over To Care Partners
Anxiety is a common nonmotor symptom of Parkinsons, occurring in nearly half of patients at some point in their lives. It can lead to worse emotional well-being, impaired daily functioning, and quality of life declines, all of which can contribute to burdens on patients and their caregivers.
While risk factors for developing anxiety have been proposed, only a couple longitudinal analyses have been done and the predictors arent well established.
Understanding predictors of anxiety symptoms in may help us to identify patients at risk for anxiety disorders, the researchers wrote, noting symptom burden could be reduced by interventions that targeted modifiable predictors of anxiety.
Also Check: Thyroid And Parkinson’s Disease
What Is Rem Sleep
- REM sleep typically begins 90 minutes after you go to sleep. Usually, the initial REM stage lasts for ten minutes. Your latter REM stages all get longer, with the last one needing to last up to an hour. Your breathing and heart rate pick up.
- Since your brain is more active during REM sleep, you have a vivid dream. REM is crucial because it activates the part of the brain that aids in learning and is linked to an increase in protein production.
- Compared to adults, newborns might spend up to 50% of their sleep time in the rapid eye movement stage.
Rbd Prognosis And Communicating The Risks
The prognosis for RBD depends largely upon the subtype. Patients diagnosed with RBD secondary to medication have the most promising prognosis of RBD resolution once the causative medication is withdrawn. However, it has been shown that RBD may persist following cessation of SSRIs , and it is therefore possible that in some cases the medication simply unmasked an already underlying pathology, triggering early clinical presentation . For RBD secondary to defined lesion e.g., inflammatory plaques, the main symptoms of RBD can be controlled relatively reliably using a combination of pharmacological and behavioral treatments. As these patient’s present with chronic but stable neural tissue damage, their RBD symptoms are unlikely to change over time.
For patients with RBD presenting as part of a clinically-defined neurodegenerative condition, such as PD, MSA, or DLB, the management of their sleep disorder should form part of their holistic care. Generally, the presence of RBD marks a less-favorable disease phenotype. In PD, for example, the presence of concomitant RBD is associated with a greater non-motor burden and a more adverse prognosis . There have been no studies of whether the symptomatic treatment of RBD impacts long-term outcomes in these patients.
You May Like: Is Rigidity A Symptom Of Parkinson’s
Patient Presentation And Diagnosis
Of those that seek medical advice, patients will usually present to their GP in the instance of self- or bedpartner injury due to their dream-enacting behaviors. In the authors’ experience, this is often a significant barrier to accessing help, with many patients, and GPs, not recognizing RBD as a medical problem. This is reflected by the diagnostic delay seen in RBD, cited between 7 and 9 years on average .
When RBD is suspected outside of the setting of a designated sleep clinic, simple screening questionnaires, such as the single-question RBD1Q , or the more detailed RBDSQ , may be used to prompt further assessment or onward referral.
Whilst these questionnaires hold some value when screening for the disorder, they do not inherently encompass the diagnostic criteria, and the cut-off points used are somewhat contentious . Thus, these scales are yet to be used as a standardized clinical resource.
Figure 2. Flow chart summarizing the process of RBD diagnosis.
Where indicated from the history and clinical examination, further investigations e.g., brain MRI, may be required to diagnose secondary RBD and inform treatment. The utility of DaTSCAN for diagnosing RBD secondary to -synucleinopathy is often limited at this stage and is not recommended .
Table 1. Diagnostic criteria for REM sleep behavior disorder .
Diagnosis And Treatment Of Parkinsons Sleep Problems
Parkinsons disease is chronic and progressive, meaning it tends to get worse over time. However, there are treatment options that can help manage symptoms and allow patients to get more restful sleep.
The simplest way to start sleeping better with Parkinsons disease is by adopting healthy sleep habits. Sleep hygiene tips for Parkinsons disease sufferers include:
- Sticking to regular bedtimes
- Following a consistent bedtime routine with soothing activities such as listening to music or reading a calming book
- Getting regular exercise, preferably early in the day
- Getting adequate exposure to light, whether outdoors or through light therapy
- Avoiding long naps and naps late in the day
- Creating a cool, dark, and comfortable sleeping environment
- Restricting bedtime activities to sex and sleep only
- Turning off screens an hour before bedtime
- Reducing liquid intake before bedtime
- Avoiding caffeine, alcohol, and tobacco
- Eating a healthy diet and avoiding large meals at night
Light therapy, exercise, and deep brain stimulation have been successfully used to improve overall sleep quality and to treat specific conditions, such as REM sleep behavior disorder, in patients with Parkinsons disease. Cognitive behavioral therapy for insomnia has proven effective at reducing insomnia in healthy adults, although further research is needed on the effects of CBT in patients with Parkinsons disease.
- Was this article helpful?
Don’t Miss: What Can You Do To Help Parkinson’s Disease
Rem Sleep Behavior Disorder
REM stands for rapid eye movement. This is the stage of sleep when dreams take place. People with REM sleep behavior disorder act out their dreams, which can be violent. RBD is one of the early warning signs of Parkinsons. Healthy people with RBD have a higher risk of developing Parkinsons. RBD can be treated with the drug clonazepam .
Dont Miss: Parkinson Bicycle Cleveland Clinic
What Is Rem Disorder
- Rapid Eye Movement REM sleep behavior disorder is a sleep disorder in which you physically act out to evade, often unpleasant dreams with vocal sounds and sudden, often violent arm and leg movements during REM sleep.
- It is also called a dream enacting behavior.
- You normally don’t move during REM sleep, a normal state of sleep that occurs many times during night.
- About 20% of your sleep is spent in REM sleep, the usual time for dreaming which occurs primarily during the second-half of the night.
Don’t Miss: Drugs Used To Treat Parkinson’s Disease
How Does Parkinsons Disease Cause Sleep Problems
Researchers have yet to uncover every nuance of the Parkinsons and sleep connection. So far, medical experts believe several causes may contribute:
- Chemical changes in the brain: Ongoing research shows that Parkinsons disease may disrupt sleep-wake cycles. Changes to certain brain chemicals may cause people with Parkinsons to get less sleep.
- Medication: Some drugs that treat Parkinsons disease may make it harder to fall or stay asleep. A medication may also disrupt your sleep patterns by making you drowsy during the day .
- Mental health challenges: People with Parkinsons commonly deal with mood disorders, such as anxiety or depression. Any mood disorder may keep you up at night or make you sleep less soundly.
- Parkinsons symptoms: Pain, waking up at night to pee or other Parkinsons symptoms can make restful sleep harder to come by. Sleep apnea can also disrupt sleep.
Dont Miss: Clinical Manifestations Of Parkinsons Disease
Complications Of Rem Sleep Disorder
Due to the potentially violent nature of their movements, individuals with REM sleep behavior disorder can put themselves and anyone they share their bed with at risk of physical injury. Depending on the nature of the dream and their bedroom environment, these injuries can be life-threatening. Up to 90 percent of spouses of those with REM sleep disorder report having sleep issues and over 60 percent have experienced a physical injury.
Even when the potential for physical injury has been reduced, the disruption of sleep to the individual or their sleep partner can still be severe enough to cause relationship problems. However, nearly two-thirds of couples continue sleeping together despite the risk of disturbed sleep.
Also Check: Signs Of Parkinson’s Disease
Conflict Of Interest Statement
GL received honoraria for participation in clinical trial as sub-investigator from UCB Pharma PC received honoraria for speaking engagements or consulting activities from Allergan Italia, Lundbeck Italy, UCB Pharma S.p.A, Chiesi Farmaceutici, AbbVie srl, Eli Lilly and Company, Zambon FP received honoraria for speaking engagements or consulting activities from Sanofi and Bial. The other authors declare no conflict of interest.