Billy Connolly Discusses Parkinsons And Cancer Diagnoses
We use your sign-up to provide content in ways you’ve consented to and to improve our understanding of you. This may include adverts from us and 3rd parties based on our understanding. You can unsubscribe at any time. More info
Parkinson’s disease symptoms mainly relate to movement because the condition results in a loss of nerve cells in the part of the brain responsible for producing a chemical called dopamine. Dopamine acts as a messenger between the parts of the brain and nervous system that help control and coordinate body movements. One area of the body that can be affected is the feet. If stiffness in the feet occurs often, it could be a sign of something more serious.
Pain Presentation And Assessment In Pd
Most epidemiological data are based on questionnaires which were not specifically validated for PD patients so that results have to be interpreted with caution. The Kings Parkinsons disease pain scale is to date the only questionnaire that is specifically calibrated and validated for PD and is highly recommended to qualitatively and quantitatively assess pain and to ascribe the pain pathophysiologically. The scale contains seven different pain domains comprising musculoskeletal pain, chronic pain , fluctuation-related pain, nocturnal pain, oro-facial pain, discolouration or oedema/swelling and radicular pain as well as 14 sub-categories . This assessment tool is based on the pain classification according to Ford but also considers pain types of other classifications such as motor fluctuations or visceral pain .
In addition, there are some specific pain syndromes in PD which have to be kept in mind, including the so-called coat-hanger pain that occurs in cases of pronounced orthostatic dysregulation and although it is more frequent in multisystem atrophy it can occur also in PD and is often associated with strong headache and neck pain . Furthermore, pain due to constipation which is frequent in PD can cause abdominal pain.
Treatment Depends On Properly Identifying The Type
If pain is bilateral always assume it is central pain pain due to PD. In my experience Azilect works great for this type of pain. Other medications which can be employed for this pain as well.
Massage therapy works for all types of leg pain-my favorite therapy but can be costly. Water therapy may also work for all types except central pain. Physical therapy can alleviate dystonia pain, as well as musculoskeletal and radicular pain.
If pain is due to dystonia related to levodopa intake, find out when it occurs—end of dose or at peak dose. Typically adjusting medication doses will resolve problem. However, if dystonia is an initial symptom of PD, initiating treatment with levodopa will resolve. If medication adjustment does not work well for levodopa induced dystonia, another treatment option is DBS . Pain due to dystonia independent of cause can also respond well to Botox injections, as well as centrally acting muscle relaxants. To avoid and alleviate pain caused by stiff muscles, a great treatment option is activity in the form of stretching exercises—any number of activities will do such as tai-chi or yoga. For me when I start having radicular pain shooting down my leg it is time to up my levodopa dosage.
If you are having leg pain make sure to discuss it with your physician.
Read Also: Amino Acids And Parkinson’s
Pain In Restless Legs Syndrome And Pd
PD patients who receive increasing dopaminergic doses over their disease course could show an increased prevalence of restless legs syndrome . First, for the treatment of painful RLS, the compensation of iron deficiency, defined as an iron storage value of less than 5075g/l, is recommended . Iron should be applied preferentially intravenously, because efficacy of oral application has not been adequately evaluated and iron given orally can deteriorate constipation and interacts gastrointestinally with levodopa and COMT inhibitors . Of note, drugs that potentially reinforce RLS such as mirtazapine, SSRI or neuroleptics, should be discontinued.
In general, painful RLS in PD should be treated according to the guidelines for idiopathic RLS recommending low-dose dopamine agonists before night-time as first choice treatment, gabapentine and pregabaline as second line options, and oycodone/naloxone as escalation therapy . In PD, the non-ergoline derivates pramipexole, ropinirole and rotigotine should be preferentially used. Because rotigotine has shown positive effects on PD-associated pain beyond the RLS, it might be preferentially used in painful RLS in PD patients .
Carbamazepine and valproic acid were considered likely efficacious in idiopathic RLS but are not suggested in PD due to potential side effects.
How To Deal With The 6 Common Causes Of Leg Pain In Pd

Severe leg pain is a common complaint from people with PD. Lately, it is understood that central pain is common to Parkinsons disease, and can even be the first sign of PD, usually bilaterally. This blog post lists six causes of lower limb pain, and the importance of treating it. Treatments depend on properly identifying the source of pain. Some treatment suggestions are included.
Read Also: Medications For Parkinson’s Disease And Side Effects
How Is Pain Treated For People With Parkinsons
No matter the cause, pain is often complex. When a person with Parkinsons experiences intense pain, especially in combination with other symptoms of Parkinsons, managing it can be challenging. There are, however, several ways you can adjust your medication regimen, exercise schedule, and lifestyle to reduce your pain and improve your quality of life.
Medications
There are various kinds of medications used to treat pain, especially for people with Parkinsons. In a recent webinar, Dr. Janis Miyasaki described how physicians approach pharmacological treatment of pain for people with Parkinsons:
The principle is to start with what is called the pain ladder. You always start with the least intensive, least side effect-giving treatment.Janis Miyasaki, MD
Step one
The first step of the pain ladder is hot and cold treatments along with stretching and flexibility exercises. People who experience rigidity and stiffness can sometimes alleviate pain using heating pads to loosen their muscles, then improve mobility by stretching, then address any residual pain with ice packs.
Step two
Step three
Step four
Step five
Other medical interventions
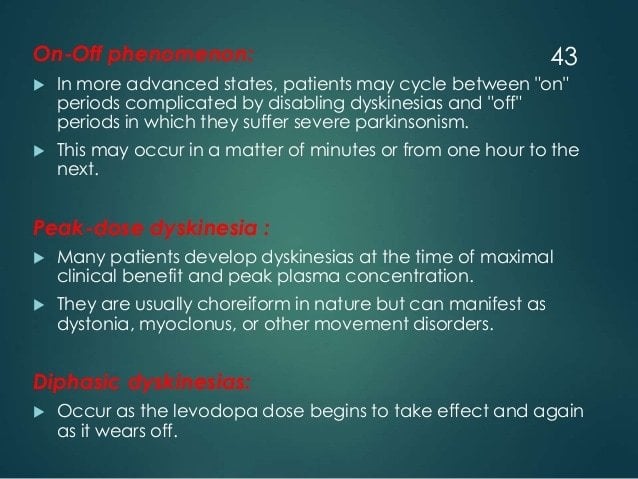
Pain Due To Fluctuations Dyskinesia Or Dystonia
To reduce potentially pain provoking motor fluctuations and dyskinesias, the optimization of therapy aiming to smoothen dopaminergic plasma level is recommended. The use of prolonged acting dopamine agonists or substances reducing the dopamine degradation such as MAO-B or COMT inhibitors are thought to reduce painful motor fluctuations during day- and night-time as well as early-morning akinesia. PD patients with motor fluctuations, who received the finally not approved partial dopamine D2 agonist Pardoprunox as adjunct therapy to levodopa, showed in a post-hoc analysis of a RCT a greater decrease in VAS pain scores compared to placebo . Amantadine might be helpful for painful dyskinesia, but data is missing.
A second substance with a potential specific effect on pain might be safinamide. In a post-hoc analysis based on pooled data of two large RCTs, safinamide applied as add-on therapy to levodopa treatment was associated with less consumption of pain medication compared to placebo and a significant reduction of pain in two of three sub-items of the PDQ-39 scale reflecting musculoskeletal and neuropathic pain . Noteworthy, in the safinamide group a slightly higher percentage of patients had additional pain medication at study baseline. In summary, this limited benefit needs to be confirmed by dedicated future studies.
Read Also: Parkinson’s And Immune System
Who Should I See To Discuss My Parkinsons Pain
Your first point of contact should be your primary doctor. Whether that means your family doctor, neurologist, or Movement Disorder Specialist , start by asking them how to manage your pain. They may prescribe you one of the medications listed above, offer suggestions about altering your lifestyle, or refer you to a pain specialist.
Pain management specialists are physicians with specialized training in the field of evaluating, diagnosing, and treating pain so, speaking to one of these specialists might be helpful for you. Be sure to get a referral from your primary care doctor, though, to ensure you are visiting a physician who understands the complexity of treating Parkinsons-specific pain.
Health and wellness providers like physical therapists, acupuncturists, and massage therapists can also be valuable members of your care team. Be willing to try new things and approach alternative therapies with an open mind, as no ones path with Parkinsons pain is the same. What works for someone else may not work for you and vice versa. Consider visiting different specialists to find a treatment plan that works best for you.
Leg Pain And Parkinson’s
Interestingly enough, one of my early symptoms of the disease was deep searing pain in my left leg, the type of pain my grandma had complained about many times. Initially this type of pain was worst in the morning as well as at night, making me think is was some sort of fasciitis. However not only did typical anti-inflammatories and muscle relaxants not alleviate my pain but pain worsened over time to a constant burning pain that felt as if someone was tearing the muscle and pouring hot oil on it. The pain was so excruciating it was permeating into all aspects of my life. I was constantly in need of deep tissue massage asking my husband to massage my legs just as my grandmother had asked of us time and time again. This helped only temporarily.
Which brings me to the four types of leg pain in PD.
You May Like: What Is The Prognosis For Parkinson’s Disease
What Drug Treatments Are Commonly Prescribed For Pain
Dopamine agonists are often the neurologists first weapon to alleviate Parkinsons-related pain. Levodopa is used to treat many types of pain due to Parkinsons because it treats the motor symptoms such as rigidity and dystonia that are causing them. Other medicines called analgesics can also be used to treat pain. When talking with your doctor, it is critical to let her know about all of the medications you are taking including over the counter drugs, herbs, vitamins and mineral supplements. Without complete information, your doctor may prescribe a drug that could have serious adverse effects.
Specific Pain Syndromes In Pd
Orthostatic hypotension can cause headache or neck pain . If necessary, antihypertensive co-medication should be adjusted in accordance with recently given recommendations . Additional measures are physical exercises, fluid intake, wearing of compression stockings class two, and administration of substances such as midodrine, fludrocortisone or, in severe cases, L-threo-3,4-dihydroxyphenylserine . Camptocormia is often accompanied with pain. Prior to therapy the cause has to be differentiated . In addition to the use of pain killers, the focus is on physiotherapy. There is no specific pain medication recommended currently.
Migraine is reported less often in PD, and often associated with depression and sleep disturbances . Therefore the therapy has to focus on the comorbidities as well. The usual medication for migraine can be used, but due to an increased risk for orthostatic hypotension in PD, caution should be exercised with beta blockers .
Read Also: Parkinson’s Coughing At Night
Ankle Stretches For Parkinsons
Seated Option: Ankle ABCs
*Use your ankle for the motion, not your knee or hip.
Standing Option: Split Stance Weight Shifting
How Do I Stop My Feet And Ankles From Hurting
Resting your feet wherever possible by not running, walking or standing for too long can help to avoid any more inflammation. Wearing comfortable shoes with good arch support will also reduce the strain on your feet. Painkillers such as paracetamol and ibuprofen can help to control the pain.
Read Also: Can Parkinson’s Tremors Come And Go
Want More Practical Articles Like This
Much more can be found in our Every Victory Counts® manual. Its packed with up-to-date information about everything Parkinsons. It also includes a worksheet and resource section to help you put what youve learned into action. Request your copy of the Every Victory Counts manual by clicking the button below.
Types Of Parkinson’s Pain
Most of the time, discomfort in muscles and joints is secondary to the motor features of Parkinsons lack of spontaneous movement, rigidity, and abnormalities of posture what is known as musculoskeletal pain. The most commonly painful sites are the back, legs, and shoulders and it is usually more predominant on the side more affected by parkinsonism.
But there are many other categories of pain associated with Parkinsons disease. Radicular or neuropathic pain is experienced as a sharp pain that can start in the neck or lower back with radiation to arm or leg respectively and is often associated with numbness or tingling, or a sensation of coolness in the affected limb. It is usually secondary to a pinched nerve due to something like a slipped disc.
Dystonia related pain occurs as its name suggests, at times of dystonia most often experienced in the foot, neck or face and arm at different points in the dosing schedule, particularly the off phase when there is not enough dopamine replacement but can uncommonly also occur at peak-dose times. It can be one of the most painful symptoms those with Parkinsons can face.
Akathisia pain is experienced as restlessness, a subjective inner urge to move, an inability to stay still and the inherent feelings of discomfort that it brings. It is primarily experienced in the lower limbs and can often be relieved by walking around.
Read Also: Is Parkinson’s A Form Of Cancer
Pain In Parkinson’s Disease
Doctors categorize pain as nociceptive, which refers to pain from tissue damage, or as neuropathic, which refers to pain that arises from the nerves. Some pain is both nociceptive and neuropathic. Most people with PD experience nociceptive pain.
This type of pain is generally localized to a specific area of the body. The most common areas for people with PD to experience pain are the neck, upper back, and the extremities . Neuropathic pain is less common in PD, although it may be caused by akathisia, an extreme restlessness.1
The pain caused by PD can generally be classified by one of five causes:
Calf Stretches For Parkinsons
Seated Option: Calf Stretch with Strap
Standing Option: Wall Push-offs x 20
*To increase the intensity of the stretch, back away from the wall until you reach a distance where you feel a strong stretch in your calves when youre leaning forward against the wall. Be sure to keep your heels down throughout the exercise.
Don’t Miss: Parkinson’s Disease And Essential Tremor
Management Of Pain In Parkinsons Disease
Issue title: Special Issue: Clinical management of Parkinsons disease: Essentials and new developments
Guest editors: Bastiaan R. Bloem and Patrik Brundin
Article type: Review Article
Authors: Buhmann, Carstena * | Kassubek, Janb | Jost, Wolfgang H.c
Affiliations: Department of Neurology, University Medical Center Hamburg-Eppendorf, Hamburg, Germany | Department of Neurology, University of Ulm, Ulm, Germany | Parkinson-Klinik Ortenau, Wolfach, Germany
Correspondence: Correspondence to: Prof. Dr. Carsten Buhmann, Department of Neurology, University Medical Center Hamburg-Eppendorf, Martinistrasse 52, 20246 Hamburg, Germany. Tel.: +49 40 7410 52771 Fax: +49 40 7410 45780 E-mail: .
Keywords: Parkinsons disease, pain, therapy, analgetics, pathophysiology, non-motor symptoms
DOI: 10.3233/JPD-202069
Journal: Journal of Parkinson’s Disease, vol. 10, no. s1, pp. S37-S48, 2020
Abstract
Toe Stretches For Parkinsons
Seated Option: Fingers Between Toes
*Cant get into the figure-4 position or reach your feet? Check out the Yoga Toes a helpful toe-stretching tool.
Standing Option: Toe Lifts
Also Check: Medical Marijuana And Parkinson’s Disease