Rem Sleep Behavior Disorder With Parkinsons Disease Can Be A Nightmare
Acting out dreams could indicate REM sleep behavior disorder. What you should know about the symptoms, diagnosis and treatment.
Certain sleep disorders are common in people with Parkinsons disease.
MORE FROM MICHIGAN: Sign up for our weekly newsletter
One of them REM sleep behavior disorder is a condition characterized by the acting out of dreams that are vivid, intense and violent. People have been known to yell or talk while asleep, carry on conversations or hit themselves or their bed partner. Even if physical damage does not occur, the condition can be frightening for the bed partner to witness.
REM behavior disorder does not necessarily disrupt the quality or quantity of sleep itself. But it is potentially harmful because of the physical movements involved.
Diagnosing Rem Sleep Behavior Disorder
To diagnose this condition, you should talk with a sleep specialist. Your doctor will need to know your medical history and will perform a neurological exam. Your doctor may even refer you to a neurologist for more comprehensive testing.
Your doctor may monitor your sleep patterns by asking you to keep a sleep diary. They may also ask you to fill out the Epworth Sleepiness Scale. This scale can help them determine how your sleep patterns are interfering with your daily life.
You may be asked to perform an overnight sleep study. In this case, you will sleep in a laboratory attached to a heart rate, brain wave, and breathing monitor. These monitors will record your sleep stages, how you move throughout the night, and if you have any other disorders that may be affecting your sleep.
What Types Of Sleep Problems Do People With Parkinsons Disease Have
Parkinsons disease affects every person differently. It also impacts sleep in different ways. People with Parkinsons may have:
- Insomnia, finding it hard to fall asleep.
- Fragmented sleep, waking up many times over the night.
- Excessive daytime sleepiness, finding it hard to stay awake during the day.
- Very vivid dreams, which may cause hallucinations or confusion after waking up.
- Emotional dreams or nightmares, which may make you feel emotionally drained after waking up.
You May Like: Does Vitamin B12 Help Parkinson’s
Rem Sleep Disorder As A Precursor To Parkinsons Disease
Posted:
Dr. Jacques Montplaisir
Every 90 minutes, during periods of sleep marked by rapid eye movements , most people lie paralyzed, breathing and dreaming. As we age, though, some of us lose that paralysis during REM sleep and begin to act out our dreams sometimes violently.
At the Université de Montréal, Dr. Jacques Montplaisir, a psychiatrist and neurobiologist, is investigating the association between REM sleep behaviour disorders and Parkinsons disease. The vast majority of people with the sleep disorder go on to develop either Parkinsons disease or dementia with Lewy bodies, another progressive neurological disease closely associated with Parkinsons. This work is being funded by a one-year, $44,850 Pilot Project Grant from the Parkinson Canada Research Program, supported by the Quebec Research Fund* on Parkinson of Parkinson Quebec.
Up to 80 per cent of these sleep behaviour disorder patients will develop Parkinsons disease or dementia with Lewy bodies within the timeframe of about 10 years, says Montplaisir. Its a very important risk factor for Parkinsons disease.
Using Positron Emission Tomography , Montplaisir and his team will scan the brains and guts of people with the sleep disorder to look for the abnormal transmission of a chemical called acetylcholine. They believe that people with the sleep disorder have a defect that is preventing them from transmitting enough of the chemical.
Find more posts about:
New Pd Subtypes In Development
New classifications of patients with PD may improve both diagnostics and the accuracy of predicted outcomes.
A newly developed system of three subtypes focuses on the severity of key motor and non-motor symptoms and highlights RBD as a relevant non-motor marker.
Thomas Warner MD told Medscape Medical News recently that We have found that it is possible to accurately predict prognosis, disability, and survival of patients with Parkinson’s disease by classifying them into different clinical subtypes at the time of diagnosis.
Warner, senior author of a new study published in January 2019 at JAMA Neurology, defines these subtypes as:
People with PD who also have RBD will likely fall into subtype 2. However, this distinct symptom can help chart a clearer treatment path and prepare you for a more aggressive clinical approach.
Recommended Reading: Judy Woodruff Health Problems
Diagnosis Of Excessive Daytime Sleepiness In Pd
In patients describing the symptoms of EDS, it is very important to determine the level of sleepiness. The Epworth Sleepiness Scale is widely used in the evaluation of EDS. Thus, ESS is a useful scale for the subjective assessment of sleepiness in patients with EDS .The ESS contains eight items, and each item is rated as maximum three points. A higher score means more sleepiness level. In addition, there are objective tests such as multiple sleep latency test and maintenance of wakefulness test for assessment EDS. The MWT is evaluation used as a polysomnographic measurement of EDS. The MSLT is measured after a PSG performed in the night to assess nighttime sleep quality and quantity . One study found that the risk of traffic accidents increased in PD patients with an ESS score greater than 7 .
Rapid Eye Movement Sleep Behavior Disorder
Rapid eye movement sleep behavior disorder is a parasomnia that arises out of REM sleep and leads to a loss of paralysis of skeletal muscles where patients may exhibit dream enactment behavior . These behaviors during sleep may range from mild muscle twitches to vocalizations to violent and complex motor behaviors. This can lead to falling out of bed, self-injury, or injury to bed partners . In fact, bed partners may be the first to note these types of complex behaviors during sleep, as patients themselves are unaware of most episodes . The prevalence of RBD is estimated to be 0.51% of the general population, but up to 50% in the PD population . A diagnosis of probable RBD can be made clinically based on the presence of nocturnal behaviors associated with vivid or violent dreams . A definitive diagnosis requires polysomnography confirmation of abnormal tonic elevation and/or bursts of muscle tone measured by electromyography , termed loss of REM atonia . The underlying mechanism leading to loss of REM atonia in PD is likely mediated by accumulation of alpha-synuclein in pontine nuclei such as the sublaterodorsal nucleus and ventral medial medulla, which send inhibitory projections to the spinal motor neurons during REM sleep . For a number of patients with PD, the symptoms of RBD precede motor manifestations and a formal diagnosis of PD by a median time of 10 years, providing an opportunity for early diagnosis and neuroprotective interventions .
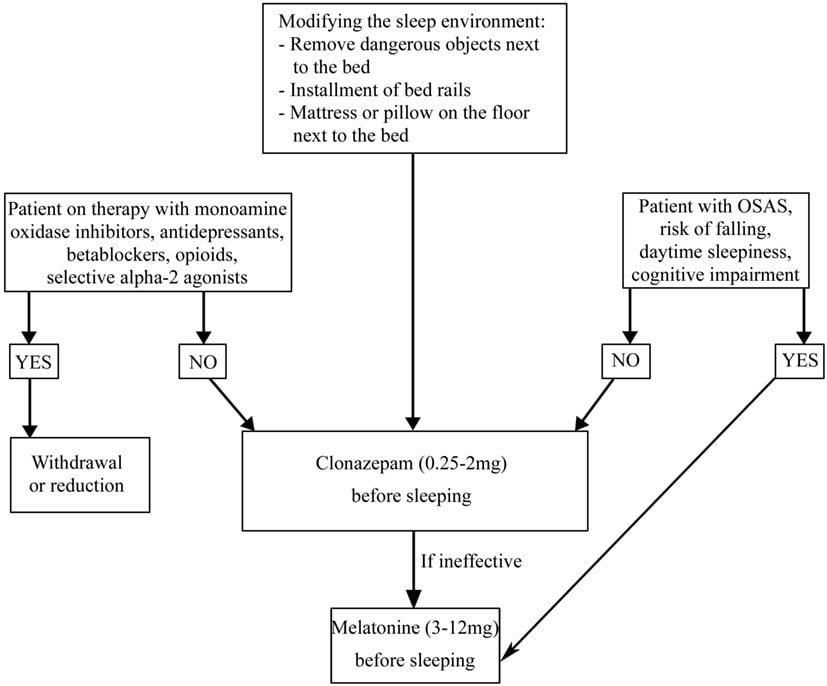
Fig. 2
Read Also: Prayers For Parkinson’s Disease
Insomnia And Nonmotor Symptoms Of Pd
Depression and anxiety affect between 30 and 60% of PD patients and appear to result from neurotransmitter changes as the disease progresses . Although early research suggested that decreases in dopamine and norepinephrine were involved in the development of depression in PD, recent literature suggests that serotonin plays a more prominent role . The presence of poor sleep and mood disturbances appears to have a reciprocal relationship, with the presence of one appearing to worsen the other . One study evaluated 98 patients with and without PD using the Insomnia Severity Index and Beck Depression Inventory to measure the impact of insomnia on depression . Total sleep time in patients with PD appeared to have a greater correlation with depression severity than that in controls which could reflect a synergistic effect of depression and PD on sleep duration .
Fig. 1
Treatment flow chart for insomnia in Parkinsons disease . Motor symptoms from PD such as tremor, dystonia, and rigidity can contribute to insomnia. The treatment of nocturnal symptoms typically employs long-acting forms of antiparkinsonian medication to last through a night of sleep. Nocturia is a symptom of PD that can significantly disrupt sleep and may be treated with behavioral modification and medications with low side effect profiles. Mood disturbances commonly contribute to insomnia and may be treated with a combination of nonpharmacologic measures and antidepressant medication
Rem Sleep Behavior Disorder
REM stands for rapid eye movement. This is the stage of sleep when dreams take place. People with REM sleep behavior disorder act out their dreams, which can be violent. RBD is one of the early warning signs of Parkinsons. Healthy people with RBD have a higher risk of developing Parkinsons. RBD can be treated with the drug clonazepam .
Don’t Miss: Parkinson Bicycle Cleveland Clinic
Treatment Of Excessive Daytime Sleepiness In Pd
The first step in the treatment of EDS should be the correction of underlying conditions . For example, it may be useful to treat the conditions that disturb sleep quality at night or to arrange medications that cause daytime sleep episodes. After that, pharmacological treatment options for EDS should be considered. Nonpharmacological treatment approaches can be performed in the treatment of mild to moderate EDS cases . Modafinil is widely used for the symptomatic treatment of EDS, which appears to stimulate catecholamine production . Common side effects of modafinil are insomnia, headache, dry mouth, dizziness, nausea, nervousness, and depression . A review has reported that sodium oxybate and methylphenidate have inadequate evidence that they are effective in the treatment of EDS in PD . Amantadine and selegiline are reported to have an alerting effect . Thus, amantadine and selegiline may be preferentially used in PD patients with EDS.
Parkinsons Disease Sleep Disorders: Treatment And Tips
If youre experiencing sleep problems in Parkinsons disease, your doctor may suggest changing or altering your medication. Some medications act as stimulants and can keep you awake. Others may wear off at night and cause a worsening of PD symptoms. If this happens, your doctor may suggest switching you to a drug thats delivered to your body continuously, such as skin patches or levodopa infusions.
If changing your medication doesnt help, you may be referred to a specialized sleep clinic. You may also need certain breathing equipment during the night if your sleep apnea is severe.
There is plenty you can do to improve your sleep health. Here are some tips to overcoming sleep disturbances in Parkinsons disease:
- Dont drink water for a couple of hours before bed
- Create a relaxing night-time routine that doesnt involve talking about heavy topics before sleep, watching TV or eating a heavy meal before you lie down
- Enjoy a warm bath in the evening before you go to bed
- Do something relaxing before sleep, such as reading or listening to an audiobook
- Get plenty of fresh air and exercise throughout the day, though you should avoid activity at least 2 hours before bed
- If possible, make sure your bedroom temperature is between 60-65 degrees Fahrenheit
- Reduce noise and light in the bedroom
Don’t Miss: Pfnca Wellness Programs
Dream Enactment In Rem Sleep
RBD is different. It only occurs during REM sleep. One remarkable phenomenon that occurs in REM sleep is the bodys natural paralysis from the chin down . During REM sleep, one should not be able to move any muscles. Dream enactment behavior, then, implies a major neurological disconnect between the brain and body during sleep.
Also intriguing – people with RBD can be very much aware of their dream content as they act it out. They may describe it as being awake and asleep simultaneously. Unlike sleepwalkers, once awakened, people with RBD can recall vivid details of their dreams.
Unfortunately, RBD can be aggressive, violent and nightmarish, leading to injuries to both the sleeper and anyone else nearby. It can even lead to property damage.
You may recall that actor Alan Alda recently shared his PD diagnosis. The problem which inspired his journey to diagnosis was dream enactment behavior, which he said preceded other PD motor symptoms like tremor.
Comic Mike Birbiglias autobiographical film, Sleepwalk With Me, recounts his RBD onset, which occurred during his first comedy tour. He was inspired to tell his story after bursting through a second-story hotel window while acting out a dream.
Conflict Of Interest Statement
GL received honoraria for participation in clinical trial as sub-investigator from UCB Pharma PC received honoraria for speaking engagements or consulting activities from Allergan Italia, Lundbeck Italy, UCB Pharma S.p.A, Chiesi Farmaceutici, AbbVie srl, Eli Lilly and Company, Zambon FP received honoraria for speaking engagements or consulting activities from Sanofi and Bial. The other authors declare no conflict of interest.
Recommended Reading: Weighted Silverware
How Is Daytime Sleepiness Treated
Consider making certain lifestyle modifications, such as:
- Establish good sleep hygiene, including a set bedtime and wake-up time.
- Get exposure to adequate light during the day and darkness at night.
- Remember indoor lighting may not be sufficient to promote a normal circadian rhythm.
- Avoid sedentary activities during the day.
- Participate in activities outside the home. They may help provide stimulation to prevent daytime dozing.
- Get physical exercise appropriate to your level of functioning, which may also promote daytime wakefulness. Strenuous exercise, however, should be avoided six hours before sleep.
- Do NOT drive while sleepy if you experience excessive daytime sleepiness. Motor vehicle accidents increase during periods of drowsiness and may be associated with sudden onset of sleep .
- Talk to your doctor about possibly decreasing the dosage of dopamine agonists if you experience daytime sleepiness or sleep attacks.
- Talk to your doctor about decreasing stimulants like caffeine, modafinil and methylphenidate .
How Can I Reduce The Consequences Of This Sleep Disorder
Treatment usually involves a combination of medication and a change in sleeping habits.
Before you see a doctor, you can use strategies to reduce the impact of these dreams on you and your partners safety. Here are some of these strategies:
- Make sure there are no sharp objects near the bed
- Place the bed against the wall or put pillows to prevent falls
- Consider installing safety rails on the bed
- Place sharp objects and furniture away from the bed
- Move the bed away from windows
- Sleep in separate rooms if your behaviour becomes too much of an inconvenience
An occupational therapists advice can also provide you with several concrete solutions to make your sleep environment safer and prevent injuries.
Recommended Reading: On-off Phenomenon
Search Strategy And Selection Criteria
This study used the search generators available in each database to search all relevant literature up to January 1, 2020 in the MEDLINE/PubMed, Embase, Cochrane, and CMB databases. The search method was based on the following terms: Parkinson’s disease and synonyms and rapid eye movement sleep behavior disorder and related terms the search commonly used acronyms for these phrases, and duplicate studies were excluded.
Patient Presentation And Diagnosis
Of those that seek medical advice, patients will usually present to their GP in the instance of self- or bedpartner injury due to their dream-enacting behaviors. In the authors’ experience, this is often a significant barrier to accessing help, with many patients, and GPs, not recognizing RBD as a medical problem. This is reflected by the diagnostic delay seen in RBD, cited between 7 and 9 years on average .
When RBD is suspected outside of the setting of a designated sleep clinic, simple screening questionnaires, such as the single-question RBD1Q , or the more detailed RBDSQ , may be used to prompt further assessment or onward referral.
Whilst these questionnaires hold some value when screening for the disorder, they do not inherently encompass the diagnostic criteria, and the cut-off points used are somewhat contentious . Thus, these scales are yet to be used as a standardized clinical resource.
Figure 2. Flow chart summarizing the process of RBD diagnosis.
Where indicated from the history and clinical examination, further investigations e.g., brain MRI, may be required to diagnose secondary RBD and inform treatment. The utility of DaTSCAN for diagnosing RBD secondary to -synucleinopathy is often limited at this stage and is not recommended .
Table 1. Diagnostic criteria for REM sleep behavior disorder .
Read Also: Similar To Parkinsons
What Are The Risk Factors For Rem Sleep Behavior Disorder
REM sleep behavior disorder primarily affects men over 60 years of age, with about 80% of cases being diagnosed with Parkinson’s disease however, the following factors may also increase the risk of developing the disorder.
- Gender: Males are more likely to develop RBD than females at a risk ratio of 9 to 1.
- Age: REM Sleep Behavior Disorder is most often diagnosed after the age of 50.
- Family History: Having a family history of narcolepsy, Parkinson’s disease or other neurological disorders may indicate an increased risk for RBD.
What Are The Complications Of Rem Sleep Behavior Disorder
Complications of RBD include accidental injury to oneself or their sleeping partner, later development of a neurological disorder such as Parkinson’s disease or Dementia with Lewy Bodies, and Excessive Daytime Sleepiness .
- Accidental Injury Accidental injury to self or bed partner occurs because the sleeper is acting out their dreams and cannot distinguish between reality and dream. Someone sleepwalking will be somewhat limited in their ability to act out physically however, this may not be the case with someone experiencing REM Sleep Behavior Disorder. The lack of muscle inhibition allows the sleeper to hit as hard as they may while awake or jump just as far as they might normally.
- Development of Neurological Disorder Because RBD is associated with the development of other neurological disorders such as Parkinson’s disease or Dementia with Lewy Bodies, many people experience some form of memory loss while awake. They may find themselves more confused, tired, or otherwise more forgetful than they would like to admit. However, this progression is more likely to occur in later stages of co-morbid diseases such as Parkinson’s disease.
- Excessive Daytime Sleepiness Excessive Daytime Sleepiness is one of the top complaints among people with RBD. This is because of the lack of quality sleep experienced while dreaming during REM sleep and common co-morbid sleep conditions like narcolepsy.
Don’t Miss: What Foods Should Be Avoided When Taking Levodopa