Deep Brain Stimulation For Parkinsons Disease Patients
Researchers are reporting a strange, unexpected side effect that some Parkinsons Disease patients are experiencing after having a deep-brain-stimulation device implanted. A small number of patients say that, after using the device to treat their Parkinsons symptoms, theyve lost the ability to swim. Researchers dont yet know whats causing the effect, but until they find out, theyre cautioning Parkinsons patients to avoid deep water if theyre using a deep-brain-stimulation device.
An Ability Lost
A report in the journal Neurology tells the stories of nine Parkinsons patients who seem to have lost the ability to swim. All of them had been able to swim despite their Parkinsons symptoms, but after they began using a deep-brain-stimulation device, they were no longer able to swim. One of the patients was not aware that he couldnt swim until he jumped into a lake and nearly drowned.
Three of the nine patients said that they regained their ability to swim after they turned off their deep-brain-stimulation device. However, their Parkinsons symptoms returned when they did, so they turned their devices back on.
Swimming is a highly coordinated movement that requires complicated arm and leg coordination, said one of the reports authors, Dr. Daniel Waldvogel of the University of Zurich in Switzerland. Exactly how deep brain stimulation is interfering with this ability needs to be determined.
What is Deep Brain Stimulation?
A Cause for Caution
Exactech Connexion Gxl Hip Implant Liner Recall Sparks Lawsuits
In June 2021, Exactech issued an urgent letter to orthopedic surgeons concerning the high failure rate of its GXL hip implant liners. There have been several articles in the medical literature questioning the early failures of the GXL hip implant liners. Exactech has also sent recall letters to some patients.
In 2019, Exactech removed the GXL liners from the US market in favor of a new product called the XLE liner. The medical literature and reports had shown hip implant patients with the GXL liner that had premature wear of the polyethylene and failure of the liners requiring revision surgery. Exactech sold almost 90,000 of these liners which were implanted in patients before it was removed from the market in 2019.
The GXL liners that have been failing were designed for use with the Exactech Novation, Accumatch and MCS hip implant systems.
Industry standards in the hip implant manufacturing community require that implants have a failure rate of less than one percent per year. That means that after 10 years 90% of implants should still be functional and after 20 years 80% of hip implants should remain functional. The Exactech implant failures with a GXL reported to the company are occurring between three and six years from the initial implant surgery.
If you have had a failure of an Exactech hip implant please contact us so we can review your case and be sure the failure is reported to the FDA.
Planning And Surgical Technique
Prior to surgery the operation is planned on a computer using MRI scans. The surgeon chooses targets in the brain . Usually two electrodes are inserted, one on each side of the head. After selecting each target point, an entry point is chosen where a hole will be drilled in the skull to pass the wire through. The entry point is chosen such that the trajectory path avoids blood vessels, thereby reducing the incidence of bleeding complications.
Caption: The Sacramento, Calif. operating room where Parkinsons disease patient Joel Davis undergoes his deep brain stimulation brain surgery for Parkinsons disease photo reproduced with permission of the photographer
You May Like: Weighted Silverware
Don’t Miss: Diseases Similar To Parkinsons
How Long Will I Be Hospitalized For
Deep brain stimulation is usually done in two steps. The first procedure consists of inserting the electrodes into the brain and usually requires you to stay in the hospital for a few days.
The second procedure, which consists of implanting the stimulator and batteries, is minor. You should be able to return home quickly. Depending on the model, the stimulator batteries may need to be recharged or replaced within three to five years.
What Care Is Needed After
On top of the wound care required with any surgery, DBS calls for special follow-up and ongoing care. Depression, falls, nausea, and problems with motor skills and swallowing can occur after DBS. In a follow-up appointment, doctors can address these issues and any other side effects of the device and/or the stimulation.1,2
Some follow-up care will last only a short time, depending on the issue. For instance, DBS can alter a persons mood, personality, and speech. Counseling, drugs, and speech therapy may help with these issues. A doctor can help find the best course of action in each case.1,2
People treated with DBS will need some extra care for the rest of their lives. Each persons device must be maintained and adjusted to meet their unique needs. Dosages of other drugs used to treat PD may also need to change over time.1,2,4
Read Also: Pfnca Wellness Programs
How Does Dbs Compare To Other Methods Of Treatment For Parkinsons Disease
As in Hardys case, every patients treatment begins with medication until it is determined that they can benefit from DBS. Medications are always tried first. Unfortunately, we can only get so far with medications. Oftentimes, many patients try them, and they may work for a little while, said Dr. Sheth.
But at some point, oftentimes the medications stop working as much because the disorder tends to progress over the years. It could get worse, and the medicines may not be able to keep up. Many of the medicines themselves have their own side effects. So, you get to a point where perhaps the medicines are helping to a degree, but they’re causing their own side effects, and exactly when we get to that point is when we introduce the idea of a surgical therapy like DBS.
Make A Donation Make A Difference
We have a close relationship with researchers working on an array of brain and mental health-related issues and disorders. We keep abreast with cutting-edge research projects and fund those with the greatest insight and promise. Please donate generously today help make a difference for your loved ones, now and in their future.
The United Brain Association No Mind Left Behind
Also Check: On-off Phenomenon
Strength And Limitations Of Deep Brain Stimulation
Even though participants still experienced progression of Parkinsons disease over the course of the study, their quality of life continued to climb by an average of 14% from the time of their surgery to their follow-up around 15 years later. That finding illustrates both the strengths and the limitations of deep brain stimulation for Parkinsons disease, experts say.
What Benefits Does The Procedure Offer
DBS is not a cure for Parkinsons, but it may help control motor symptoms while allowing a reduction in levodopa dose. This can help reduce dyskinesias and reduce off time. DBS does not usually increase the peak benefits derived from a dose of levodopa the best levodopa response before DBS is a good indicator of the best response after DBS. But it can help extend the amount of on time without dyskinesias, which may significantly increase quality of life.
DBS does not provide most patients benefit for their non-motor symptoms, such as depression, sleep disturbance, or anxiety. DBS also does not usually improve postural instability or walking problems. If a symptom you have does not respond to levodopa, it is not likely to respond to DBS.
Read Also: On Off Phenomenon
How Is Deep Brain Stimulation Performed
Before the actual procedure begins, for most patients, a head frame is positioned on your head, which keeps your head still during brain imaging and is used to deliver the electrode to the target in the brain. Surgical pins or screws are used to secure the frame to your head. Sedation is typically given during this portion of the procedure.
Your neurosurgeon will implant the deep brain stimulation system in one to three stages.
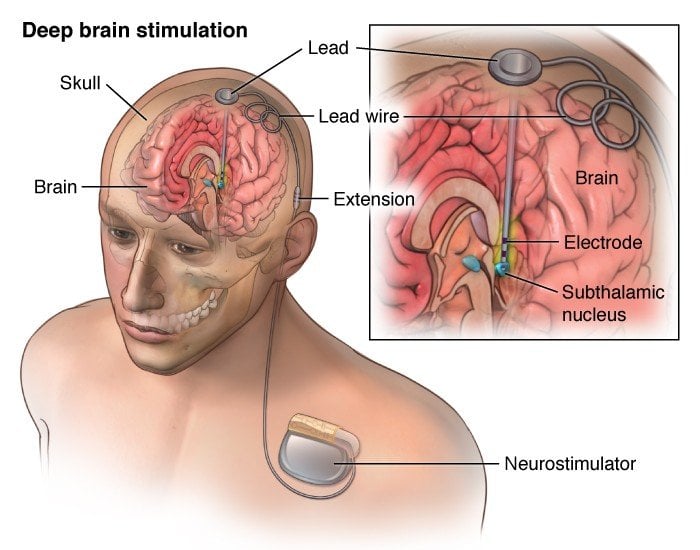
First, a small hole is made in the skull. The leads, which have electrodes at the ends, are passed through this hole and surgically implanted in the areas of the brain identified as the site responsible for the movements caused by Parkinsons disease.
Most people with Parkinson’s disease will require one lead placed on each side of the brain unless symptoms are mostly one-sided . Each side of the brain controls the opposite side of the body, so each lead is inserted on the opposite side of where symptoms are occurring. Sometimes this procedure is done in stages one lead is placed at one time followed by another surgery for the other side. In other patients, both leads are placed during the same operation. Many times patients are awake during lead insertion. An intraoperative MRI is also sometimes used to image the lead location.
What Are The Risks And Complications Of Deep Brain Stimulation
As with any surgical procedure, there are risks and complications. Complications of DBS fall into three categories: surgery complications, hardware complications, and stimulation-related complications.
- Surgical complications include brain hemorrhage, brain infection, wrong location of the DBS leads, and less than the best location of the leads.
- Hardware complications include movement of the leads, lead failure, failure of any part of the DBS system, pain over the pulse generator device, battery failure, infection around the device and the device breaking through the skin as the thickness of skin and fat layer change as one ages.
- Stimulation-related complications occur in all patients during the device programming stage. Common side effects are unintended movements , freezing , worsening of balance and gait, speech disturbance, involuntary muscle contractions, numbness and tingling , and double vision . These side effects are reversible when the device is adjusted.
Also Check: Sam Waterston Tremor
How Common Is Dbs
Dr. Sheth describes DBS as a very standard treatment. These are procedures that we do week in and week out, he said. It’s not investigational or experimental. Around the world, more than 150,000 patients have had DBS for Parkinson’s or tremor with a success rate of 95%.
Patients need to know that there are these alternatives. They need to know that they’re not necessarily stuck with these symptoms, that there may be a different way to get better control. That discussion is, of course, individual-specific, but the availability of these types of surgical treatments is important for patients to know about.
What Risks Come Along With Doing Deep Brain Stimulation
DBS is a surgical procedure. As with any surgery there are some risks associated with it. Some of the risks of DBS include infection and bleeding. Your neurosurgeon may discuss some additional risks with you. Studies have shown that any risks are relatively small, but they should be kept in mind when considering DBS.
Also Check: Adaptive Silverware For Parkinson’s
How Effective Is Dbs Therapy
Though DBS is considered an alternative, its a well-established, FDA-approved technique that has been used to treat Parkinsons and essential tremor for 30+ years.
There’s been a lot of studies over the years, said Dr. Sheth. Randomized trials have been presented in the top medical journals that show that for the appropriately chosen patient, DBS is more effective than the best medical therapy. So, in that appropriately chosen patient, DBS can be very successful at improving tremor for essential tremor and tremor stiffness, rigidity, and those other motor symptoms of Parkinson’s disease.
One patient who has found success with DBS is Rudy Hardy.
Its made a profound difference in my life, said Hardy. A professional sports photographer and professor of criminal justice, Hardys life was controlled by Parkinsons. He tried medication initially, and though it seemed to work for a while, his tremors eventually worsened. Since undergoing DBS, Hardys symptoms are now almost completely undetectable. Watch Hardy talk about his experience with DBS below.
Is Deep Brain Stimulation Right For You
While deep brain stimulation is shown to offer long-term benefits, the treatment does come with some risks. According to the Parkinsons Foundation, there is a 1% to 3% chance of developing an infection, cranial bleeding, stroke, or other complications from the treatment.
Furthermore, deep brain stimulation might work better for some people than others. It might be an option worth considering if youve experienced symptoms of Parkinsons for at least five years, are struggling with side effects of Parkinsons medications, or your symptoms make it difficult to perform everyday activities, among other factors.
The decision for or against deep brain stimulation should be made by having the potential candidate evaluated by a multidisciplinary team who can together construct a risk-benefit profile for a potential candidate, explains Dr. Okun. The team commonly is made up of a neurologist, a neurosurgeon, a neuropsychologist, a psychiatrist, and rehabilitation specialists.
Talk with a neurologist if you have Parkinsons disease and youre interested in exploring deep brain stimulation.
Also Check: Cleveland Clinic Parkinson’s Bicycle Study 2017
Testing Before Deep Brain Stimulation
For patients with Parkinsons disease, the doctor must confirm that the PD is levodopa-responsive and determine which symptoms are most likely to respond to DBS and discuss these with the patient.
To accomplish these two objectives, the movement disorders neurologist will examine the patient in the absence of his or her PD medications, then again after having taken them. Seeing the effect of PD medications on the movement and non-motor symptoms helps the physician and patient identify good target symptoms for DBS.
A cognitive assessment can help determine a persons ability to participate in the procedure, which involves providing feedback to the doctor during surgery and throughout the neurostimulator adjustment process. This assessment also informs the team of the risk of having worsened confusion or cognitive problems following the procedure.
Some hospitals also perform an occupational therapy review or speech, language and swallowing assessment. A psychiatrist may examine the person to determine if a condition such as depression or anxiety requires treatment before the DBS procedure.
Deep Brain Stimulation At Michigan Medicine
For carefully selected patients with Parkinsons disease, Essential Tremor, and Dystonia, deep brain stimulation offers a therapeutic surgical option that can reduce or eliminate movement-related problems and greatly improve quality of life. At the University of Michigan Health System, our STIM program brings together a team of medical experts who are leaders in their respective fields and on the cutting-edge of the latest research.
Also Check: Sam Waterston Parkinson’s
Deep Brain Stimulation For Parkinsons Disease
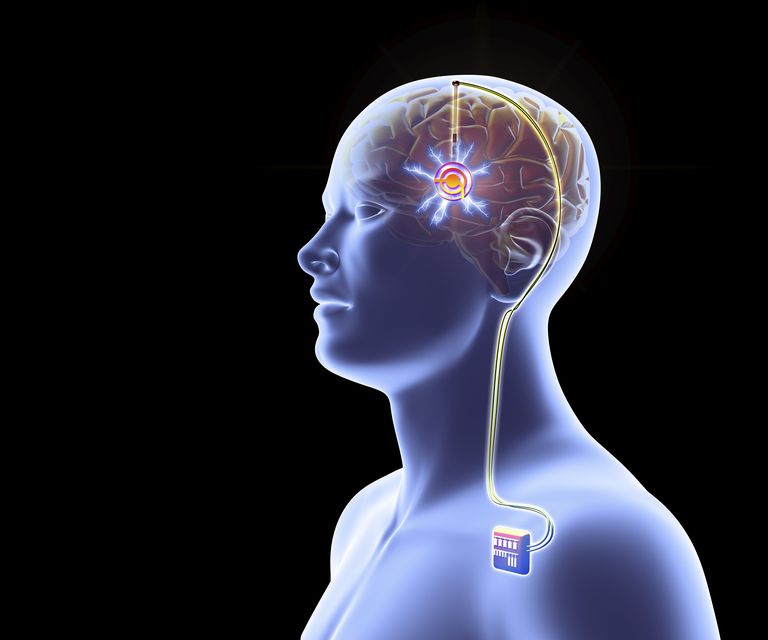
For people with severe motor symptoms of Parkinsons disease that are not adequately controlled by medication, a treatment called deep brain stimulation may offer some relief.
Deep brain stimulation requires the surgical placement of a small conductor called an electrode in the brain. The electrode delivers electrical stimulation that blocks the nerve signals that cause tremors.
Specialists at NYU Langones Center for Neuromodulation perform more than 100 deep brain stimulation procedures each year. Our neurologists, neurosurgeons, and psychiatrists provide a thorough evaluation to ensure youre a good candidate for the procedure.
What Did The Research Involve
The researchers recruited 251 people from Germany and France with Parkinsons disease and early movement problems. To be included, patients had to be between 18 and 60 years, have had Parkinsons for at least four years, and not have a severe form of the disease.
Patients with major depression or dementia were not included in this study. They were randomly assigned to receive either neurostimulation plus medical therapy , or medical therapy only .
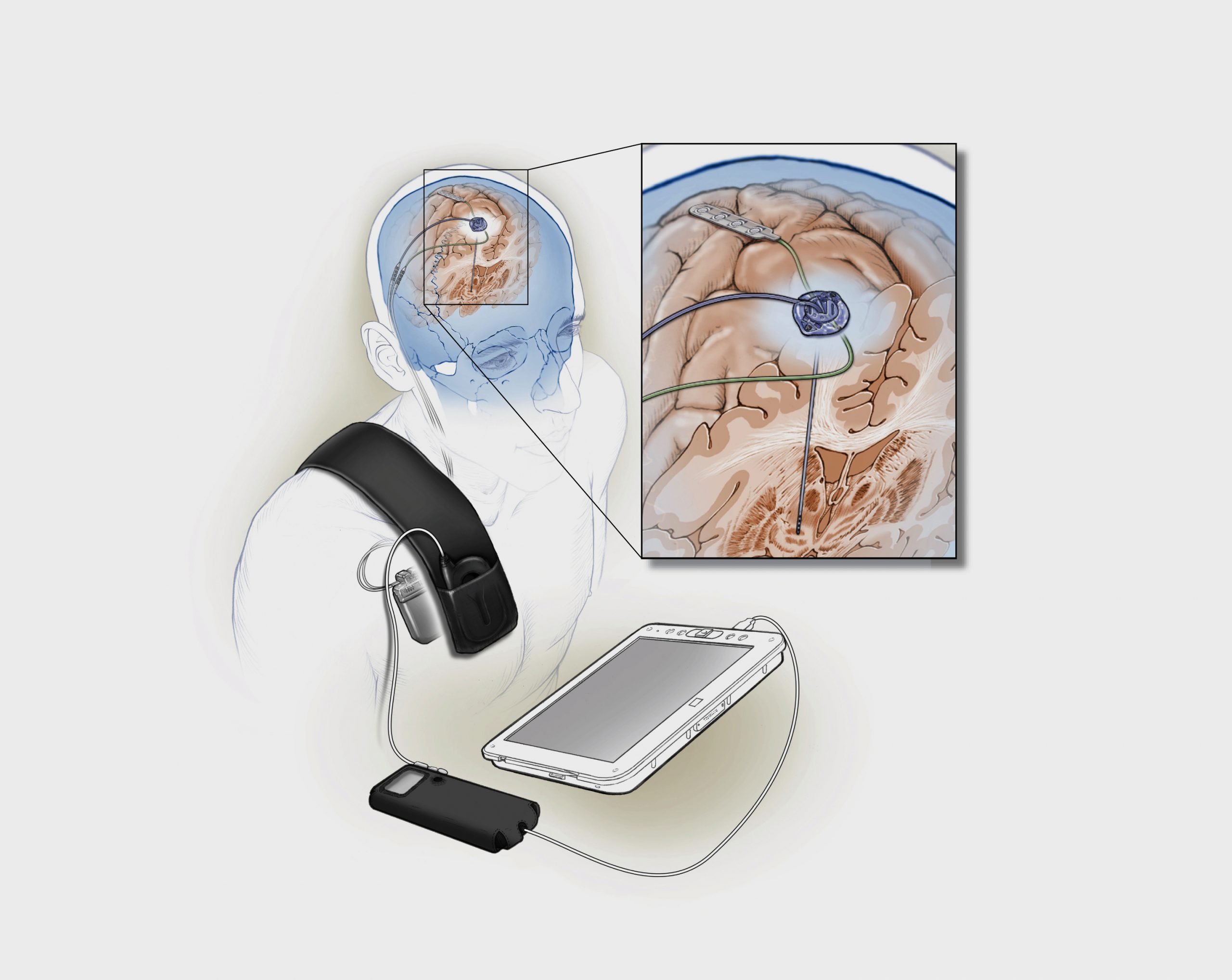
The neurostimulation group underwent surgery to have electrodes implanted into certain parts of the brain and were fitted with a neurostimulator that was connected to the electrodes.
The electrical implant generated small electrical signals to stimulate the brain and was controlled by a handheld device. These electrical signals block abnormal nerve signals, which are thought to trigger the symptoms of Parkinsons disease.
Medical therapy involved standard drug therapy for Parkinsons disease. All patients were then assessed at five months, one year and two years.
The primary outcome of the trial was disease-related quality of life at two years, which was assessed using the Parkinsons disease questionnaire . The PDQ-39 is essentially a scoring system that assesses the extent that the disease has impacted a persons quality of life. Scores in the questionnaire ranged from 0 to 100, with higher scores indicating worse function.
Other outcomes measured were:
- time with good mobility and no dyskinesia
- adverse events
You May Like: Fitflop Shoes For Parkinson’s
You Are About To Exit The Abbott Family Of Websites For A 3rd Party Website
Links which take you out of Abbott worldwide websites are not under the control of Abbott, and Abbott is not responsible for the contents of any such site or any further links from such site. Abbott is providing these links to you only as a convenience, and the inclusion of any link does not imply endorsement of the linked site by Abbott.The website that you have requested also may not be optimized for your screen size.
Will I Be Asleep During The Entire Procedure
You will be sedated or receive local anesthesia for part of the procedure, may or may not be awake for lead and electrode placement, and will be asleep when the impulse generator is implanted. To provide more details:
- A local anesthetic is applied to areas of the head where pins or screws are used to secure the head frame and sedation is given.
- You will be sedated during the beginning of the procedure, while the surgical team is opening the skin and drilling the opening in the skull for placement of the lead.
- Most patients will be awake for lead and electrode placement. This part of the procedure is not painful, as the brain does not feel pain. Being awake allows the surgical team to interact with you when testing the effects of the stimulation. However, some patients who cannot tolerate the procedure while awake can have the electrode and lead placed under general anesthesia. The lead placement is guided in real time by magnetic resonance imaging. The procedure is performed in a special MR-equipped operation room.
- Implantation of the pulse generator in the chest and connection of the leads from the device to the lead in the brain is usually done under general anesthesia.
Recommended Reading: Prayer For Parkinson’s Disease