Q: Will Medicare And/or Private Insurance Cover The Costs Of Palliative Care
A: I can tell you that our Legacy Care Program is covered and does not affect any other payments made by Medicare and/or private insurances. For any other program, I would advise and strongly suggest that you check with the care-providing agency of choice to confirm coverage.
Tips and Takeaways
- Palliative care is a clinical approach that focuses on improving quality of life for people with complex diseases. It can begin at any point during disease progression and work in conjunction with a treatment plan.
- Palliative care programs for PD provide people with PD and their care partners additional resources and check-ins as the disease becomes more complex and difficult to manage. Multi-disciplinary care is provided with a focus on maximizing communication between the team members.
- Palliative care is different from hospice care. Palliative care refers to all treatments throughout the disease course focused on quality of life. Hospice care on the other hand, is provided to improve the quality of life only when end of life is near.
- Discuss the possibility of a palliative care referral with your movement disorders neurologist. A social worker may also be able to connect you with a palliative care program.
Do you have a question or issue that you would like Dr. Gilbert to explore? Suggest a Topic
Dr. Rebecca Gilbert
APDA Vice President and Chief Scientific Officer
Theme 1desire For A Comprehensive Tool For Future Planning Such As A Roadmap
When initially asked about future planning related to living with PD, patients and care partners recognized the difficulty of knowing what questions to ask or what information is important. In early interviews, as participants considered what would be important to them related to living with PD, the metaphor of a roadmap emerged and was explored in-depth. When considering the future, patients and care partners had several questions related to how their PD would change over time and how quickly it would change . These questions reflected a desire for information that would address their personal experiences compared to an expected PD trajectory and/or the experiences of others. In their own words, patients identified the concept of a roadmap: A roadmap, or even things we should be looking at in end stage, would be helpful . Another patient in standard care described specific questions a roadmap might address, stating,
where the rest stops are, not all symptoms are the same. Where would the be? How much longer is it going to take it for me to get there? Dont we have stuff that we can look forward to? Thats what Im hoping for so that maybe we get control over it. How else would you know?
Stage Two Of Parkinsons
In this stage symptoms may be more noticeable. Tremors maystart to appear and changes in facial expressions. Muscle stiffness might beginor get worse if its already being experienced. This could make walking alittle more difficult and change posture.
Speech difficulties can start to arise too and some everydaytasks such as getting dressed or shopping may become a little tricky tonavigate without help.
Also Check: How To Test Yourself For Parkinson’s
Q: What Typically Prompts A Person Treated At Your Parkinsons Center To Be Referred To The Palliative Care Program
The main criterion is that the person with PD meets the Medicare definition of homebound status . We also consider the distance they live from the Muhammad Ali Parkinson Center the further away a patient lives from our center, the more likely they need additional help. Patients that have limited support from family members or need a multi-disciplinary team approach are also candidates for referral.
Eating Drinking And Parkinson’s Disease
- Don’t rush your meals. Allow the extra time you need to finish your meal. Rest your elbows on the table to provide more motion at your wrist and hand.
- Sit with your knees and hips bent at a 90-degree angle in a straight-back chair.
- Use utensils with built-up, lightweight handles, or use a “spork” — a spoon and fork in one. Use a rocker knife for cutting food.
- Use a non-skid mat to stabilize objects on the table.
- Use a plate guard or plate with a raised lip to prevent food from spilling.
- Use a long straw with a non-spill cup or use a plastic mug with a large handle.
Recommended Reading: Stem Cells For Parkinson’s Disease Therapy
How Is Parkinsons Treated
Parkinsons disease can also be broken down into four stages: diagnosis, maintenance, complex and palliative. In the early stages of Parkinsons disease, medication treatment can be very effective. However as the disease progresses into the complex and palliative stages, the individual may become more restricted despite an ideal medication therapy regime.
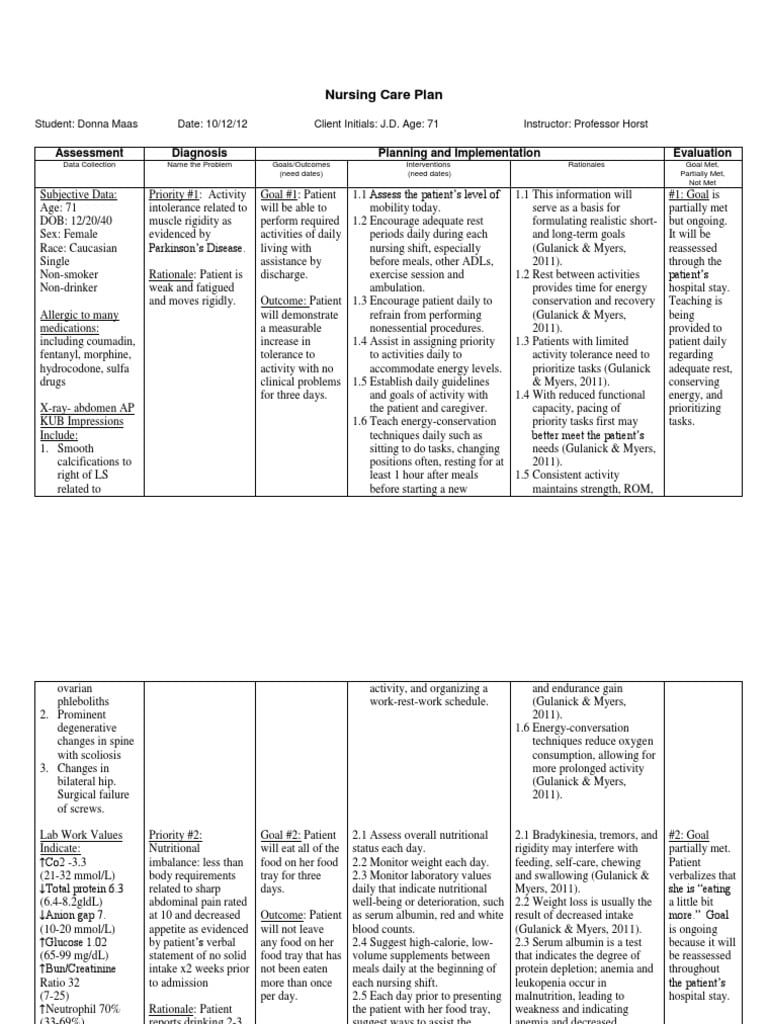
There is no ideal medicinal treatment for Parkinsons. Therapy will be tailored to the individual, their symptoms, disease progression, lifestyle and physical tolerance. However most medication prescribed to someone with Parkinsons will fit into one of these categories:
- Levodopa dopamine replacement therapy
- Dopamine agonists mimic the action of dopamine
- COMT inhibitors these are used in conjunction with Levodopa and blocks the COMT enzyme to prevent levodopa breaking down in the intestine so more of it will reach the brain
- Anticholinergic block the effect of acetylcholine to rebalance its levels with dopamine
- Amantadine has anticholinergic properties and improves dopamine transmission
- MAO type B inhibitors prevent the metabolism of dopamine within the brain
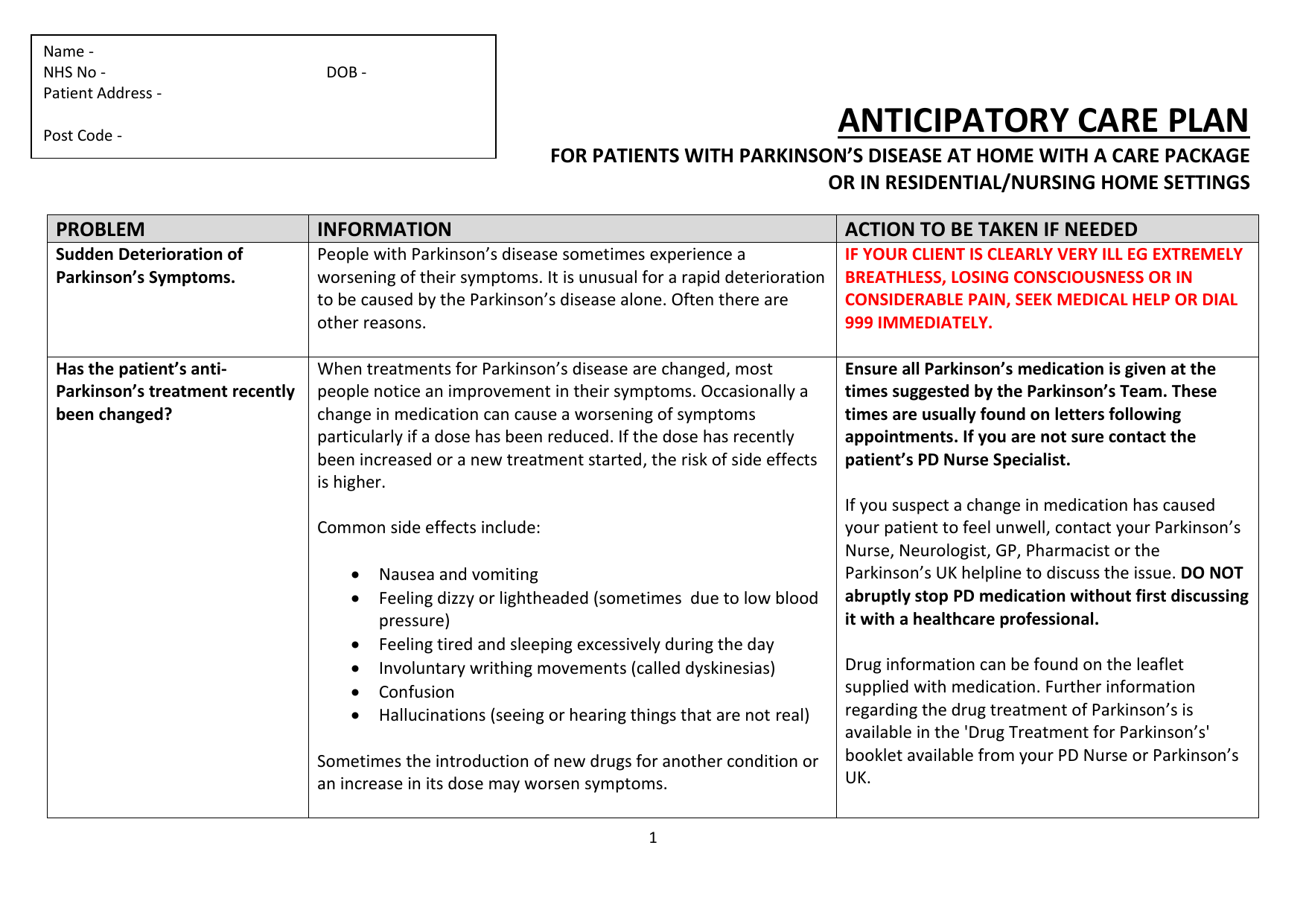
As the disease progresses, medication management for the individual will need to change. However one important factor which must be taken into consideration regarding medications is time. These medications need to be taken on time: if they are taken late, they can severely impair the movements of the person with Parkinsons.
Theme : Personal Definitions Of Acp Vary In The Context Of Pd
Patients and care partners affected by PD described a variety of personal definitions of ACP. These personal definitions or viewpoints were often shaped by their experience of PD or by other ACP or end-of-life experiences prior to PD diagnosis. The existence of these working definitions of ACP influenced their prior engagement in ACP, current willingness to discuss ACP, and were sometimes inaccurate or incomplete definitions of ACP compared to a traditional medical definition.
One personal definition of ACP was that it should be a part of routine care. Participants with this view of ACP often described engaging in ACP prior to their PD diagnosis because they had witnessed or were involved in someone else’s end-of-life experience. Some participants who had ACP conversations before the time of PD diagnosis described the necessity and benefits of engaging in ACP on a routine basis. Others held personal definitions of ACP that acknowledged the potential for future PD-related changes these individuals often chose to focus on ways to maximize their current quality of life given the uncertainties about future decline. For example, this view of ACP led to planning trips or enjoying activities that contributed to personal fulfillment. The emphasis on quality of life plans was often associated with engaging in ACP discussions and decisions about future medical care planning and documentation as part of routine medical care.
Also Check: Emotional Symptoms Of Parkinson’s
Theme : Patient Relationship And Health Care System Barriers Exist To Engaging In Acp
At the patient and care partner level, relational issues between the patient and partner or family were another barrier. Both patients and care partners separately described the challenges of desiring to talk about future medical care planning but facing resistance from the other person. Others were concerned about protecting the emotional well-being of their partner, family members, or young children. For individuals who described this barrier, having care partners who were willing to play an active role in ACP and having interdisciplinary team-based approaches helped to navigate the tensions between a patient and care partner.
Finally, there were also health care systemlevel barriers, including patients’ lack of trust that ACP preferences would be honored by clinicians or the health care system. Participants were concerned that regardless of prior documentation regarding ACP preferences for future medical care, their actual end-of-life situation was too dependent on the decisions of hospitals or clinicians. This perceived barrier was common among patients and care partners receiving standard care, though it also concerned PC arm participants.
Theme 2care Partner Preferences For Specific Future Planning
Care partners also desired a comprehensive tool to help navigate future planning. In many cases, care partners were able to specifically describe their need for practical guidance to navigate the PD journey. A care partner from the palliative care arm described,
Knowledge is power, so you need to know how to prepare yourself if you can. One of the things that I would like to know more about is the caregiving later. I was talking to a social worker that said there are real problems down the road financially if you have to go into assisted living, and I need to know more about that to prepare financially.
Table 2 shows questions that both patients and care partners from both standard care and the palliative care arm had about the future. Common questions included what to expect, how to gauge PD-related severity, how to plan for future needs, and who to ask for support. In some cases, questions from care partners incorporated concrete options and related considerations or limitations because they were already thinking far down the road, while patients often felt like they were trying to adjust to current physical and cognitive changes due to PD. When patients were open to discussing future planning, they could identify the change or challenge that would need to be addressed but sometimes were not able to articulate multiple options and decisions.
Table 2
Read Also: Parkinson’s Disease Brain Changes
How Do I Get Organized
Caring for someone with Parkinsons disease means keeping lots of medical records, medical and family contact lists, financial documents and other information organized and handy. To avoid getting overwhelmed, below are some tips on what information to gather and how to keep it all organized.
Consider creating a binder with the following main document categories: Medical, Family, Insurance/Property and Finance. Even though you can now manage nearly everything online, it can be useful to have a physical copy of everything in one place. Wherever you choose to maintain your records, make sure that a close family member or friend knows where to find them in case they are needed.
And remember, its not all about the person with Parkinsons. Make sure to keep your records organized, too!
What Are The Symptoms Of Parkinson’s
The main motor symptoms of Parkinsons are:
- tremor
- slowness of movement
- problems with balance.
However, the condition doesnt only affect movement. People living with the condition can experience a range of non-motor symptoms that can often have a greater impact on their lives than movement difficulties.
Non-motor symptoms include:
- urinary urgency, frequency
- pain.
These non-motor symptoms are present at all stages of the condition but they can become more severe in the later stages of Parkinsons and have a major impact on quality of life.
Parkinsons gets worse over time and it can be difficult to predict how quickly the condition will progress. For most people, it can take years for the condition to progress to a point where it can cause major problems. For others, Parkinsons may progress more quickly.
Also Check: Can A Blood Test Detect Parkinson’s
Training And Coaching Of Parkinsons Disease Nurse Specialists
Before the start of the study, we will organize a single training session with all participating PDNSs . The goal of this meeting is to acquire commitment to the study and uniformity in workflow by reviewing the Nursing care in Parkinsons disease guideline to explain the study specifics and to discuss practical issues related to the study intervention. In addition, PDNSs will be closely coached in order to optimize the intervention and adherence to the guideline. Every month, an experienced PD nurse from Radboudumc will have an individual intervention session with each PDNS, mainly to discuss difficult cases and to optimize the intervention and its uniformity. Finally, we will organize a video meeting every 3 months with all PDNSs to maintain their commitment, support each other, discuss difficulties related to the study, and give each other advice .
Importantly, for the purpose of this study, we will implement an increase in nursing staff capacity for participating nurses. This will allow us to study the real impact of current usual care, which would not be achieved by adding a new set of specifically trained research nurses to the existing PDNS staff. The PDNSs are all graduated nurses with a certificate in Parkinsons nursing. Furthermore, they have achieved a standard of competence as described in the Nursing care in Parkinsons disease guideline .
Ethics Approval And Consent To Participate
This study will be conducted in accordance with the good clinical practice guidelines promulgated by the International Conference on Harmonization, the principles of the Declaration of Helsinki, and the Medical Research Involving Human Subjects Act. The NICE-PD study protocol and communication materials have been approved by the local ethics committee . The study is registered with the ClinicalTrials.gov registry . The trial results will be reported according to the Consolidated Standards of Reporting Trials 2010 guidelines .
When a patient meets the inclusion criteria, informed consent will be obtained by the research team after the team explains the procedures and requirements of the study, how subjects confidentiality will be maintained, and any potential hazards/risks. Each patient will sign an informed consent form in person at the baseline visit before baseline assessment takes place. The researcher will sign the informed consent immediately after the patient has signed it. The researcher provides a copy of the signed informed consent form to each participant and keeps a copy in the participants study file.
When important changes are made to the study protocol , the principal investigator will notify relevant parties about these changes, and a copy of the revised protocol will be sent to these parties . Furthermore, the updated protocol will be included in the trial registry.
Recommended Reading: Medicinal Plants For Parkinson’s Disease
Screening For The Early Symptoms And Signs Of Pdd
PD impacts people in different ways. Not everyone will experience all the symptoms of PD at the same time or follow the same pattern. But PCPs should be familiar with the common symptoms or typical patterns of progression in PD that are defined in stages . PCPs should also know the risk factors that make PD patients more likely to experience dementia because the clinical symptoms of both syndromes can overlap to a high degree. PCPs should always consider seeking reversible medical conditions that can affect mental function in PD patients. A flowsheet for screening generated here should help PCPs and their team to achieve this goal during a patients routine annual wellness visit or general visit.
| Items | |
|---|---|
| recognize this is a risk factor | |
| Stage of PD | severity of motor impairment from PD, another risk factor for PDD |
| cognitive functions | search cognitive function stage including attention, executive, and visuospatial functions |
| Dementia Screen Indicator | screening possible high-risk patients. If it is negative, follow up periodically. If it is positive, further investigation is needed. |
| Geriatric Depression Scale | search for mood disorders |
| PHQ-9 screen for depression | further evaluation of depression |
| to stage mental dysfunction, better specificity and sensitivity |
Develop A Support Group
Caring for a loved one can be deeply satisfying. Its a chance for your family to draw together as you face the challenges of Parkinsons disease head-on.
However, providing emotional and physical care for someone with an illness can become stressful and, at times, overwhelming. Balancing your personal life with caregiving can be difficult. Many caregivers will face periods of feeling guilty, angry, and abandoned.
Of course, you dont have to experience this alone. Support from other family members or professionals can help:
- relieve stress
- reevaluate approaches to treatment
- offer new perspective on the caregiving relationship
Ask your doctor or your local hospitals health outreach office for contact information for a Parkinsons disease caregiving group. The person youre caring for will likely also benefit from being part of a support group.
Support groups allow for open communication with other people facing the same struggles. These groups also provide an opportunity to share suggestions, ideas, and tips among the group members.
Read Also: Wearable Technology For Parkinson Disease
Treatment Of Parkinsons Disease
Currently, Parkinsons disease has no cure. However, treatments are extremely helpful in managing its signs and symptoms.
Optimizing Future Planning In Parkinson Disease: Suggestions For A Comprehensive Roadmap From Patients And Care Partners
Sarah R. Jordan1, Benzi Kluger2, Roman Ayele3,4, Adreanne Brungardt1, Anne Hall5, Jacqueline Jones4, Maya Katz6, Janis M. Miyasaki7, Hillary D. Lum1,8
1Division of Geriatric Medicine, Department of Medicine, University of Colorado Anschutz Medical Campus , 2Departments of Neurology and Medicine, University of Rochester Medical Center , Rocky Mountain Regional Veterans Affairs Medical Center , University of Colorado Anschutz Medical Campus , 6Movement Disorders and Neuromodulation Center, University of California VA Eastern Colorado Geriatric Research Education and Clinical Center , , USA
Contributions: Conception and design: All authors Administrative support: SR Jordan, A Brungardt Provision of study materials or patients: B Kluger, M Katz, JM Miyasaki Collection and assembly of data: SR Jordan, A Brungardt, J Jones Data analysis and interpretation: All authors Manuscript writing: All authors Final approval of manuscript: All authors.
Correspondence to:
Background: Living with Parkinson disease is complicated by an unpredictable disease course which can delay planning for future needs. This study explores patient and care partner needs related to future planning using a palliative care framework with physical, psychological, social, cultural, end-of-life, and ethical aspects of care in PD to guide analysis.
Keywords: Caregiver decision-making palliative care Parkinson disease qualitative
Submitted Aug 16, 2019. Accepted for publication Sep 10, 2019.
Don’t Miss: Medications For Parkinson’s Patients