Pain In Parkinsons Disease: A Spotlight On Women
This 2-page interview with neurologist, Dr. Jori E. Fleisher, discusses pain in Parkinsons disease with some interesting statistics about women and pain. Dr. Fleisher outlines the 4 primary types of pain in PD, how depression interferes with pain management, the role of exercise and medications in pain management as well as alternative therapies.
What Are The Symptoms Of Atypical Parkinsonian Disorders
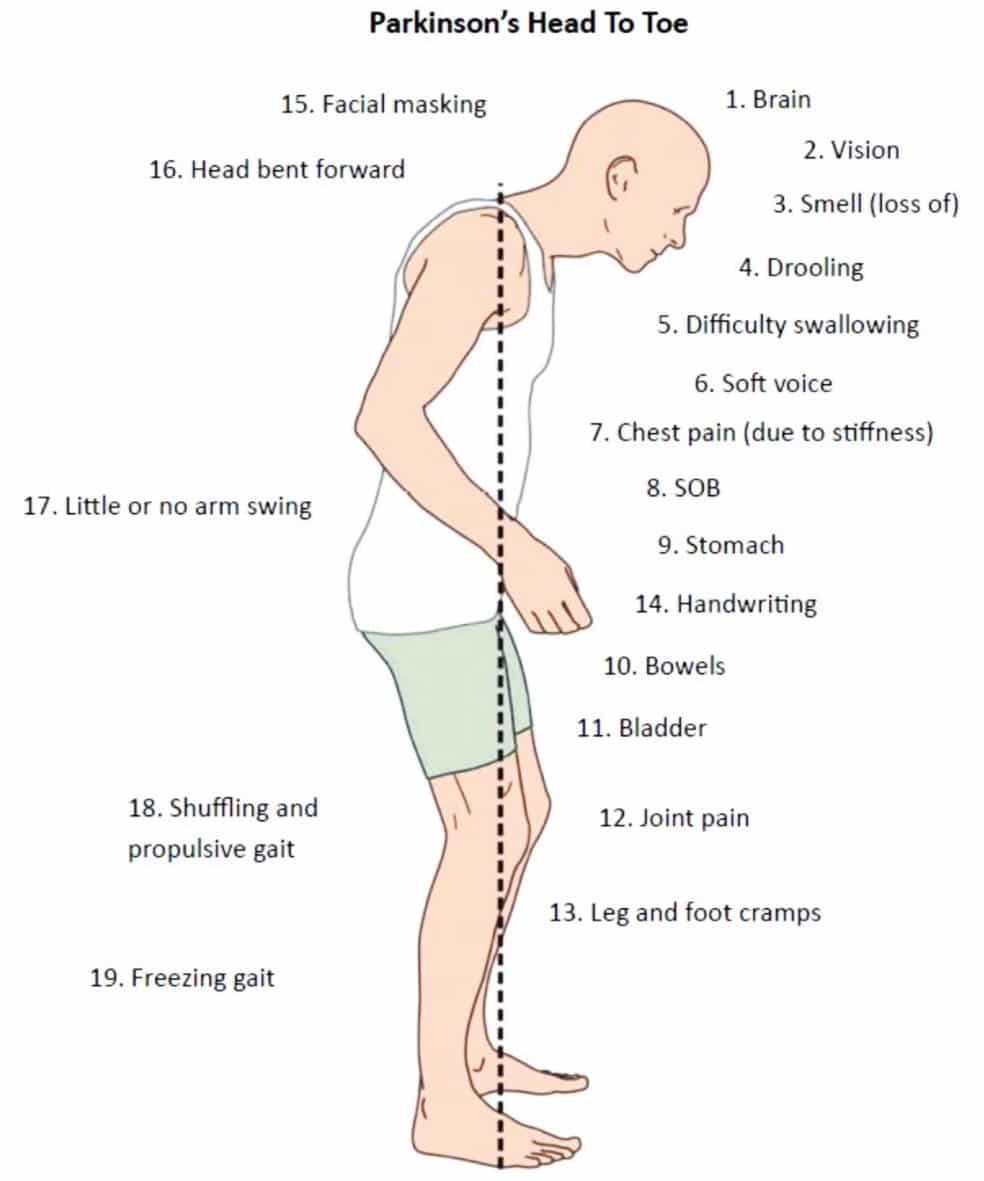
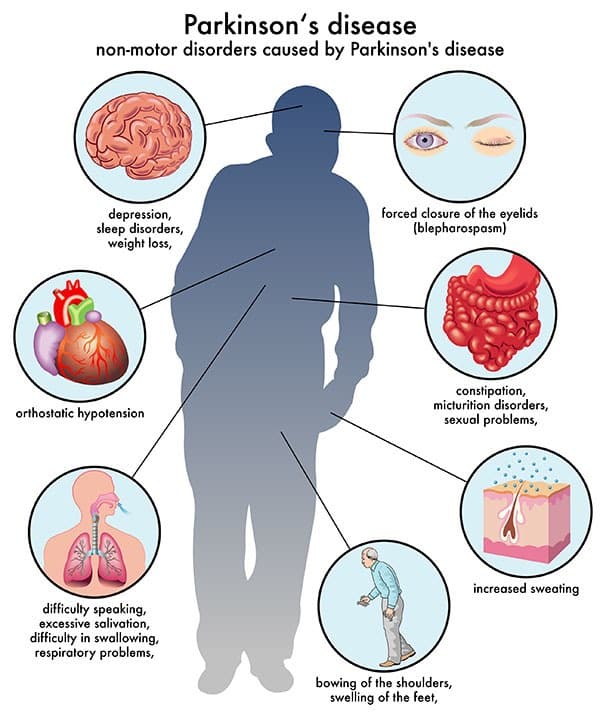
Like classic Parkinsons disease, atypical Parkinsonian disorders cause muscle stiffness, tremor, and problems with walking/balance and fine motor coordination.
Patients with atypical Parkinsonism often have some degree of difficulty speaking or swallowing, and drooling can be a problem. Psychiatric disturbances such as agitation, anxiety or depression may also be part of the clinical picture.
Dementia with Lewy bodies can cause changes in attention or alertness over hours or days, often with long periods of sleep during the day. Visual hallucinations typically of small animals or children, or moving shadows in the periphery of the visual field are common in DLB. DLB is second only to Alzheimers disease as a cause of dementia in the elderly, and it most commonly affects patients in their 60s.
Patients with progressive supranuclear palsy may have difficulties with eye movements, particularly when looking downward, and with balance when descending stairs, for instance. Backward falls are common and may occur during the early course of the disease. PSP is not usually associated with tremor, unlike Parkinsons disease.
Parkinsonâs Disease and Movement Disorders Center
Examples Of Pain Scales
Visual analog scale
A visual analog scale measures a continuum of a chosen present characteristic. For example, the experienced pain that a patient feels extends over a continuum from no pain to an extreme intensity of pain. This range of perceived pain appears continuous for the patient. Pain does not appear as an ordinary scale with jumps between the values, such as discrete, moderate, or severe. Word descriptors are only used in both ends of the line, which is usually 100 mm in length. This valuation is very subjective and best used within an individual and not between groups of individuals at the same time point. Most experts argue that a VAS at best can produce data of ordinal type. This is important to consider in the statistical analysis of VAS data. Rank ordering of scores rather than the exact values might be the best way to handle patient registrations on the 100 mm line.
Brief Pain Inventory
The Brief Pain Inventory was initially created for the purpose of measuring pain in cancer patients. It measures pain relief, pain quality, and patient perception of the cause of pain in terms of pain intensity and pain interference .
Read Also: Mushrooms For Parkinson’s Disease
What Can We Do
It would seem to me that there are a number of very vicious circles and negative feedback loops between neck stiffness/rigidity/pain and neck immobilization and posture in PD, which not only impact on each other, but also have neurological and physiological implications much more broadly, including on nervous system, blood pressure and breathing. The principal strategy for progressive symptom reduction would therefore be to increase and maintain mobilization of the neck and to improve posture as much as possible, through daily exercises and therapies, and to address any old injuries elsewhere on the body which may be impacting on posture and hence neck strain.
Dr Farias provides a suite of daily exercises which help to reduce these type of neck problems over time, especially designed for, and tailored to the different types of, cervical dystonia. Many people around the world report that doing his exercise classes daily reduces the symptoms and pain of their neck dystonia, and can eventually even lead to a full recovery. This works through a process of neuroplasticity, which re-wires the connections between the muscles and the brain through movement therapy.
Pain In Parkinsons Disease
Parkinsons patients suffer from the same pain other people have, often amplified by the motor dysfunction, but they also have additional pain problems unique to PD. Lower back pain and back of he neck pain are most common. Strengthening exercises or stretching may be helpful. Identifying the cause of the pain is essential in treating the pain. Treatments include physical therapy, medications, and alternative therapies like Reiki, acupuncture and massage.
You May Like: Caring For Someone With Parkinsons Disease
You May Like: Non Invasive Treatment For Parkinson’s Disease
Parkinsons Atypical Parkinsonism Can Have Same Symptoms
Getting a diagnosis of Parkinsons can take time because not all symptoms may be identified by conventional tests run in the doctors office. The diagnosis can be even harder when symptoms overlap with other neurodegenerative diseases that present as atypical parkinsonism, such as cortical basal degeneration and progressive supranuclear palsy, known as PSP.
Atypical parkinsonism shows up as muscle tremors and stiffness, but is caused by different disorders than Parkinsons.
As such, there is an urgent need for biomarkers in tissues and/or bodily fluids that may help discriminate between these similar conditions, and thereby reduce delayed diagnosis and misdiagnosis.
A previous study showed that levels of certain proteins including alpha-synuclein in the cerebrospinal fluid , which surrounds the brain and the spinal cord, could help discriminate Parkinsons from atypical parkinsonism. However, CSF collection is a highly invasive procedure.
In recent years the possibility of using neural-derived extracellular vesicles as a window into the brain has been suggested, the researchers wrote.
NDEVs are tiny molecule-filled vesicles released by neurons or nerve cells and involved in cell communication. They are readily accessible, as they can be isolated from blood and analyzed in their content of disease-associated molecules, the researchers wrote.
A minimally invasive blood test measuring the concentration of and tau aggregates can represent a promising tool
Nerves And Nervous System
The vagus nerve is not the only important nerve which passes through the neck. According to the polyvagal research of Dr Stephen Porges, five of the cranial nerves form the parasympathetic ventral vagus complex, responsible for Social Engagement functions. Interestingly, this vagal complex includes the accessory nerve, that innervates the neck muscles used to turn the head. In his early paper on polyvagal theory, Dr Porges writes:
Thus, more specialized functions such as head rotation to orient sensory receptors toward the source of stimulation, mastication to ingest food, and salivation to initiate gustatory and digestive processes are integrated into the vagal system.
In mammals, the part of the brain where these nerves originate controls the complex coordination of pharynx, soft palate, larynx, and esophagus. Of special note to psychophysiological processes the carotid body, containing peripheral chemosensitive receptors sensitive to oxygen and carbon dioxide levels
In addition, the accessory nerve provides fibers originating in the cervical spinal cord that innervate the positioning of the neck. The critical carotid arteries, internal jugular veins, and vagus nerves run deep in these muscles.
Thus, this complex also has the ability to orient visceral receptors via somatic muscles , to coordinate structures related to ingestion and expulsion, and to regulate facial expression and emotion.
Read Also: Leg Weakness Parkinson’s Disease
How Might Dystonia Be Experienced
- Feet: people with Parkinsons mainly experience dystonia in their feet. Typically the toes curl up into a claw-like position, the foot turns inwards at the ankle, and occasionally the big toe sticks up. This position, caused by spasms in the calf muscles, can be very uncomfortable and makes it hard to fit feet into tight shoes.
- Hands: writers cramp in the hands only occurs during handwriting.
- Neck: cervical dystonia affects the neck muscles, which causes the head to twist to one side, forwards or occasionally backwards.
- Eyelids: the eyelid muscles may contract and make the eye close involuntarily . This is often experienced as excessive blinking, intolerance to light, a burning feeling in the eye or irritation.
- Vocal cords: dystonia affecting the vocal cords or speech muscles makes speaking difficult or strained.
- Jaw area and side of the face:oromandibular dystonia affects the jaw area, tongue, mouth or one side of the face. The jaw may be pulled either open or shut, and speech and swallowing can be difficult.
Dont Miss: How Long Parkinson Patients Live
Can Parkinsons Disease Be Prevented
Unfortunately, no. Parkinsons disease is long-term disease that worsens over time. Although there is no way to prevent or cure the disease , medications may significantly relieve your symptoms. In some patients especially those with later-stage disease, surgery to improve symptoms may be an option.
Dont Miss: Plan Of Care For Parkinsons Disease
Read Also: What Is Stage 5 Parkinson’s
What Lifestyle Changes Can I Make To Ease Parkinsons Symptoms
Exercise: Exercise helps improve muscle strength, balance, coordination, flexibility, and tremor. It is also strongly believed to improve memory, thinking and reduce the risk of falls and decrease anxiety and depression. One study in persons with Parkinsons disease showed that 2.5 hours of exercise per week resulted in improved ability to move and a slower decline in quality of life compared to those who didnt exercise or didnt start until later in the course of their disease. Some exercises to consider include strengthening or resistance training, stretching exercises or aerobics . All types of exercise are helpful.
Eat a healthy, balanced diet: This is not only good for your general health but can ease some of the non-movement related symptoms of Parkinsons, such as constipation. Eating foods high in fiber in particular can relieve constipation. The Mediterranean diet is one example of a healthy diet.
Preventing falls and maintaining balance: Falls are a frequent complication of Parkinsonâs. While you can do many things to reduce your risk of falling, the two most important are: 1) to work with your doctor to ensure that your treatments whether medicines or deep brain stimulation are optimal and 2) to consult with a physical therapist who can assess your walking and balance. The physical therapist is the expert when it comes to recommending assistive devices or exercise to improve safety and preventing falls.
Read Also: Cleveland Clinic Parkinsonâs Bicycle Study 2017
Are My Tremors Associated To Parkinsons Disease
Several neurological conditions can cause tremors and having tremors does not necessarily mean you have Parkinsons disease.
Tremors associated to Parkinsons disease are resting tremors, which occur when the body part is inactive. This typically starts in one hand, fingers, or a foot. Tremors can also affect the jaw or tongue, which can lead to communication difficulties.
As with stiffness, Parkinsons tremors mainly affect one side of the body.
If you think you have resting tremors, consult your doctor. They will perform tests to exclude any other condition often confused with Parkinsons disease.
Recommended Reading: Cleveland Clinic Parkinsons Bicycle Study 2017
You May Like: Emory Parkinson’s Disease Research
Fluctuations Of Pain Experiences In Pd
Patterns of NMS fluctuations are heterogeneous and complex. Psychic NMS seem to fluctuate more frequently and severely than nonpsychic symptoms. A recent study of ten frequent NMS in advanced PD using VAS rating scales in motor-defined on- and off-states, as well as self-ratings at home, confirmed previous suspicions that increased pain in off-states and pain fluctuations correlate with a low health-related quality of life. Pain as NMS was more frequent in the off-state more precisely, it was three to four times more common during the off-state than during the on-state.
How Can You Improve Aggressiveness And Hallucinations In Parkinsons
Hallucinations may spark anger or aggression in a person with Parkinsons disease. Some ways to help include:
- Reassure them, tell them they are safe.
- Speak slowly and calmly.
- Ask questions about the persons feelings.
- Listen to the person, dont interrupt.
- Avoid sudden movements.
- Give the person space and a way out, so they dont feel cornered or threatened.
- Make an emergency plan ahead of time for what you and others in the house will do if the person experiencing hallucinations becomes a danger to themselves, you, or anyone else.
- When it is safe, help the person speak with their healthcare provider about making a plan to address the hallucinations.
You May Like: Big Exercises For Parkinson’s Disease
Clinical Diagnosis Of Rigidity
A doctor will test for rigidity by flexing and extending the patients relaxed wrist and elbow joint, and look for sustained rigidity or intermittent rigidity if tremors are associated with it.
Clinically, Parkinsons rigidity is characterized by increased muscle tone during examination using passive movement of the affected body parts. Parkinsons rigidity is more marked in flexor muscles than extensor muscles . Rigidity may be enhanced by voluntary movement of other body parts and is more pronounced during slow stretching rather than fast stretching. These features help to differentiate Parkinsons rigidity from spasticity, which becomes worse during fast movements.
When Should I See My Healthcare Provider Or When Should I Seek Care
You should see your healthcare provider as recommended, or if you notice changes in your symptoms or the effectiveness of your medication. Adjustments to medications and dosages can make a huge difference in how Parkinsons affects your life.
When should I go to ER?
Your healthcare provider can give you guidance and information on signs or symptoms that mean you should go to the hospital or seek medical care. In general, you should seek care if you fall, especially when you lose consciousness or might have an injury to your head, neck, chest, back or abdomen.
Also Check: Lumbar Spine Surgery In Patients With Parkinson Disease
Treatment And Management Options
There are several treatment options available to alleviate the motor symptoms associated with Parkinsons disease. Most of them also help Parkinsons patients overcome issues related to rigidity. These include:
- Medications such as levodopa , dopamine agonists, anticholinergics, catechol-O-methyl transferase inhibitors, and monoamine oxidase-B inhibitors. One treatment or a combination of treatments is commonly prescribed to Parkinsons disease patients to improve motor problems, including rigidity, that occur due to dysfunction in dopaminergic neurons.
- Physiotherapy to improve mobility and the range of movement in muscles and joints, and to alleviate the muscle cramps common in Parkinsons disease patients. An occupational therapist or physiotherapist can advise on daily routines, exercises, and the use of assistive devices, such as walkers or canes, to help the patient stay as mobile and independent as possible. Occupational therapy is generally needed for patients to perform daily activities more effectively, such as rolling in bed or getting up from a chair, for example. Regular exercise and stretching can strengthen muscles and maintain flexibility.
- Speech therapy that teaches facial exercises to help with speech and communication.
- Deep brain stimulation for Parkinsons disease patients whose symptoms are not adequately controlled with medications and/or exercise.
A Critical Reappraisal Of The Worst Drugs In Parkinsons Disease
What are the worst drugs for Parkinsons disease patients? Couldnt a simple list be assembled and disseminated to the Parkinson community? Recently Ed Steinmetz, an experienced neurologist in Ft. Meyers, FL pointed out to me, a list approach published in the Public Citizen Newsletter . The approach was to list every drug associated with a single confirmed or unconfirmed symptom of Parkinsons disease or parkinsonism. Parkinsons disease is defined as a neurodegenerative syndrome , whereas parkinsonism encompasses a wider net of drug induced and other potential causes. In parkinsonism symptoms are similar to Parkinsons disease, but patients do not have Parkinsons disease. Patients and family members confronted with a simple drug list approach may falsely conclude that most medicines are bad for Parkinsons disease, and that any medicine may cause parkinsonism. This concept is in general, incorrect. Although the approach is well-meaning, it is in need of a major revision, as Parkinsons disease and parkinsonism are too complex to summarize by simple lists. In this months column I will try to summarize the key information that patients and family members need to know about the worst pills, for Parkinsons disease and parkinsonism.
A Florida Parkinsons Treatment Blog by Michael S. Okun, M.D.
UF Center for Movement Disorders & Neurorestoration, Gainesville FL
Read Also: Genetic Link Between Parkinson’s And Schizophrenia
Parkinsons Disease: Causes Symptoms And Treatments
Parkinsons disease is a brain disorder that causes unintended or uncontrollable movements, such as shaking, stiffness, and difficulty with balance and coordination.
Symptoms usually begin gradually and worsen over time. As the disease progresses, people may have difficulty walking and talking. They may also have mental and behavioral changes, sleep problems, depression, memory difficulties, and fatigue.
While virtually anyone could be at risk for developing Parkinsons, some research studies suggest this disease affects more men than women. Its unclear why, but studies are underway to understand factors that may increase a persons risk. One clear risk is age: Although most people with Parkinsons first develop the disease after age 60, about 5% to 10% experience onset before the age of 50. Early-onset forms of Parkinsons are often, but not always, inherited, and some forms have been linked to specific gene mutations.
The Substantia Nigra And Movement
The reason that Parkinsons causes movement symptoms is that the substantia nigra makes up part of the circuitry, called the basal ganglia, that the brain uses to turn thought about movement into action.
The structures of the basal ganglia.
The substantia nigra is the master regulator of the circuit, it mainly communicates using the chemical dopamine, but other chemical transmitters are also used to communicate between other areas of the basal ganglia.
The balance of signals being sent between these structures allows us to control movement. But as Parkinsons progresses, and the dopamine-producing brain cells in the substantia nigra are lost, movement symptoms appear. Without enough dopamine, it becomes harder to start and maintain movements, which leads to symptoms such as slowness of movement, rigidity and freezing. And an imbalance of signals in the basal ganglia means people with Parkinsons can experience what is known as a resting tremor.
But while this is the description of Parkinsons you may find in most textbooks, it is now recognised that changes are not limited to the substantia nigra and basal ganglia.
Recommended Reading: Parkinson’s Causes And Prevention