Case : Bilateral Gpi Dbs
This patient was a 59-year-old man with PD and severe camptocormia. Parkinson disease was diagnosed based on the initial presenting symptoms of a severe stooped posture, decreased fine finger movements, and bilateral hand tremor. The patient’s camptocormia only minimally responded to dopaminergic medications, and he would fall several times a day. He had begun wearing kneepads to prevent further injury from his frequent falls. He underwent placement of bilateral GPi DBS electrodes to alleviate his parkinsonian symptoms as well as treat his camptocormia. He was discharged to an acute rehabilitation facility on postoperative Day 5 in good condition. At 15-month follow-up, while having some improvement in his parkinsonian symptoms, he continued to suffer from severe camptocormia.
Demographic Data And Clinical Outcomes
Patients with DiLL0° were defined as DiLL , and those with DiLL< 0° were defined as DiLL . The patients preoperative data, including age, sex, body mass index , preoperative lumbopelvic parameters , lumbar flexibility , scoliosis, number and levels of fused segments were compared between the two groups. The incidence of postoperative R-ASD and S-ASD, bony fusion rate, pre- and postoperative VAS, JOA, and ODI scores, postoperative improvement in VAS, JOA, and ODI scores and postoperative Nakais score were compared between the two groups. Furthermore, the above-mentioned clinical data were compared between the DiLL and DiLL groups after excluding patients with scoliosis .
Being Prepared & Anticipating Problems
Because of the concerns that we will discuss below, it is prudent to have your neurologist speak to your surgeon and anesthesiologist prior to the surgery so he/she can discuss the potential issues that may arise during and after the surgery. It is also very useful to have your neurologist write a letter with all the necessary information so it can be dispersed to other members of the medical team who will be responsible for your day-to-day care after the surgery.
Depending on the type of surgery, there may be more than one option for anesthesia. General anesthesia may not be the only option, and a more localized form of anesthesia may be possible. Local anesthesia typically causes fewer side effects. Discuss what anesthesia options you have with the surgeon and anesthesiologist prior to the surgery.
In addition, if the surgery requires you to stay in the hospital overnight, consider having a family member or friend stay with you. This person can provide a calming presence, helping to prevent agitation or distress. He or she can keep an eye on whether you are taking your own medications correctly and what additional medications you are bring given.
Don’t Miss: Is Coffee Bad For Parkinson’s Disease
Can Deep Brain Stimulation Help With Parkinsons
Parkinsons Disease is a life-altering condition. In the past, the belief was those with Parkinsons would live out their days in agony. But, there is hope with the advancement of technology. Deep Brain stimulation is an option to help those with Parkinsons disease live a better quality of life. Heres how deep brain stimulation works
Dealing With Lumbar Spinal Stenosis
As we get older, nothing seems to work as efficiently as in our younger days. This is even true of the spine and the spinal cord within it. Over time the spine can develop degenerative changes that lead to compression of the spinal cord. This condition is called spinal stenosis and can lead to serious
Recommended Reading: Severe Parkinson’s Disease Symptoms
Lumbar Spine Surgery In Parkinsons Patients: Good Results
Researchers from New York and Israel have taken on an unusual topiclumbar spine surgery in patients with Parkinsons disease. The investigators, from Hadassah Hebrew University Medical Center in Jerusalem, and Beth Israel Medical Center and Hospital for Special Surgery in New York City, found that Parkinsons patients fared well after undergoing lumbar spine surgery, and experienced a decrease in pain.
According to the study, the team identified 96 patients who underwent lumbar spine surgery between 2002 and 2012. Of these, 72 had spinal stenosis, 17 experienced spondylolisthesis, and 7 suffered from coronal and/or sagittal deformity. The visual analog scale for back pain improved from 7.4 cm preoperatively to 1.8 cm postoperatively. The visual analog scale for lower-limb pain improved from 7.7 cm preoperatively to 2.3 cm postoperatively. The Oswestry Disability Index score dropped from 54.1 points to 17.7 points at the time of the latest follow-up.
Josh Schroeder, M.D., an orthopedic surgeon with Hadassah Hebrew University Medical Center, told OTW, The study was prompted by several patients who suffered from Parkinsons disease. We tried to locate existing data on the topic, but could not find any large study on Parkinsons, despite this being a disease that affects 5% of the elderly population.
Initial Surgery At Our Hospital
Based on the observations, imaging findings, and the patients needs, posterior osteotomy, canal decompression, and internal fixation of the T10-L3 intervertebral plate with bone graft fusion was selected as the treatment option. After the surgery, the patient got out of bed with the protection of a brace, and the pain in the lower back was reduced. Additionally, sensation in the lower limbs was normal, and bowel movement was normal too. The surgical incision healed well and met the criteria for first-stage healing. Postoperative lumbar spine radiography and CT showed that the kyphosis was corrected and the nail rod was not loosened . The patient was satisfied with the outcome of the surgery and was discharged from the hospital. He was asked to continue with oral Parkinsons therapy with additional bisphosphonates, calcium, and vitamin D3 for anti-osteoporosis treatment. The patient was instructed to wear a brace during all daily activities.
Figure 3. Imaging features after initial surgery at our hospital. Postoperative 1-week radiograph indicated alleviation of the kyphosis. Postoperative 1-week CT scan indicated good internal screw fixation .
Unfortunately, a follow-up radiograph taken 1 month after surgery showed a loosening of the L3 pedicle screw. The patient was advised to continue anti-osteoporosis treatment and Parkinsons treatment and wear a brace and was counseled in preparation for possible secondary surgery.
Also Check: Do You Capitalize Parkinson’s Disease
Mis Surgical Treatment For Kyphoscoliosis In A Patient With Parkinsons Disease
24/3/2019
MIS Surgical Treatment for Kyphoscoliosis in a patient with Parkinson’s Disease
The most common neurodegenerative disease is Parkinson’s disease . Its clinical manifestations are tremor, rigidity, and akinesia. Patients with PD could have stooped posture and different types of postural and striatal deformities may also be developed. Multiple studies show that these may also be apparent in roughly a third of PD patients resulting in severe disability.
These can include antecollis or dropped head, Pisa syndrome, camptocormia, kyphosis or/and scoliosis, striatal hands, and striatal toes.
The pathogenesis of these deformities is a combination of central and peripheral impacts such as rigidity, dystonia, and degenerative skeletal changes.
The standard practice in these patients to aim at a long-lasting effect is an open instrumented fusion of the spine usually combined with osteotomies and/or anterior fusion to decompress neural elements, maintain or restore the patients balance.
In combination with the comorbidities seen within this age group, these operations are related to a high rate of complications.
A blood loss of more than 2 liters is considered to be one of the risk factors.
Duration of parkinsonism symptoms is a major risk factor and these deformities are seen in an advanced stage of the disease in most patients.
Patient female 75 years old with a history of Parkinsons Disease treated with medication for 10 years.
Technique
Examining The Correlation Between Preoperative Dill And Clinical Outcomes
Correlation analysis was performed between the preoperative DiLL and R-ASD, S-ASD, and bony fusion status at 1 and 5 years, postoperatively, and each clinical score to examine the association between preoperative DiLL and postoperative clinical outcomes. To exclude the influence of age, sex, BMI, presence of scoliosis, and the number of fused segments, multiple regression analysis was performed after appropriate adjustments.
Read Also: Does Parkinson’s Make You Forgetful
Parkinsons Disease And Preparing For Surgery
People with Parkinsons disease sometimes face procedures or surgeries due to other medical conditions not related to PD. These could be relatively simple procedures such as a colonoscopy or endoscopy, common surgeries such as cataract removal, gall bladder removal or hernia repair, or more complex surgeries such as open-heart surgery or transplant surgery. I am frequently asked about specific concerns that arise when contemplating surgery for someone with PD.
People with PD, as well as people with other brain disorders, are more prone to side effects from anesthesia as well as negative effects from the stress of the surgery itself. Its important to remember that not everyone is affected in the same way, and this doesnt mean people with PD cannot have the surgeries and procedures they need. It is however important to be educated about what potential problems may arise so that you are as prepared as you can be.
The Effect Of Parkinsons Disease On Patients Undergoing Lumbar Spine Surgery
Jeffrey Gilligan
1Department of Neurosurgery, Icahn School of Medicine at Mount Sinai, New York, NY, USA
2Department of Neurosurgery, North Jersey Spine Group, Wayne, NJ, USA
3Department of Orthopaedics, Icahn School of Medicine at Mount Sinai, New York, NY, USA
Abstract
1. Introduction
Parkinsons disease is a neurodegenerative disorder characterized by resting tremors, rigidity, bradykinesia, postural instability, and gait disturbances . The prevalence of PD in industrialized countries is estimated at 0.3% of the entire population with approximately 7 million people affected worldwide . PD is an age-related disease which is rare before the age of 50, with a prevalence of about 1% in people over the age of 60 and up to 4% in people over the age of 80 .
PD is increasingly recognized as an important cause of spinal disorders requiring surgical intervention . However, spinal procedures can be complicated by underlying osteoporosis and severe musculoskeletal dysfunction in this population.
In this study, we investigate the effect of PD on patients undergoing lumbar spine surgery. The aim of this study is to identify the incidence, trend, risk factors, outcomes, and cost of lumbar spinal surgery for degenerative disease in PD patients.
2. Materials and Methods
2.1. Sample Selection
2.2. Outcome Measures
2.3. Data Analysis
No Institutional Board Review approval was required for this study.
3. Results
| Demographics |
4. Discussion
5. Conclusion
Data Availability
Disclosure
Read Also: Essential Tremor And Parkinson’s
Myopathy Associated Postural Deformity In Pd
Inflammatory myopathy of the paraspinal muscles can mimic the appearance of camptocormia in PD. Wunderlich et al.38 have described a 63-year-old man with PD in whom a camptocormia-like deformity developed. They noted hyperintensity within the paraspinal muscles and histopathological features consistent with myositis. The patient was treated with steroids and they noted marked improvement in forward flexion.
Myopathy with nemaline rods, end-stage myopathy with autophagic vacuoles, mitochondrial myopathy, and necrotizing myopathy have all been associated with camptocormia in patients with PD.15,25,30 Gydnia et al.15 have studied 19 consecutive muscle biopsies obtained in patients with PD and either camptocormia or dropped-head syndrome , finding abnormal muscle biopsies in all patients. Although MRI images were not abnormal in all patients, MR imaging generally showed fatty degeneration of the paravertebral musculature or neck extensor musculature in many of them. Electromyography was also generally consistent with myopathy changes.
Demographics Of Patients With And Without Parkinson Disease

Demographic data for patients who underwent surgery for low lumbar OVC below L3 are shown in Table . OVC occurred at L3 in 18 cases, L4 in 18, and L5 in 7. Of the 43 patients, 11 had PD, and 32 did not have PD . There were no significant differences in gender, mean age at the time of surgery, history of other fragility fractures, comorbidities, steroid intake, medication for osteoporosis, affected vertebra levels, surgical procedures, and JOA scores before and after surgery in PD and non-PD patients. BMI was lower in PD cases, but with no significant difference to that in non-PD cases . The mean follow-up period was 3.7±1.0 and 3.5±2.0 years in PD and non-PD cases, respectively. The Hoehn & Yahr stage before surgery was stage II in 5 patients and stage III in 6. Progression of severity of PD occurred in 4 of 11 patients : 3 of 5 in stage II reached stage III, and 1 of 6 in stage III reached stage IV.
Table 1 Demographic data for patients with low lumbar osteoporotic vertebral collapse with and without Parkinsons disease.
Also Check: Uab Parkinson’s Disease Center
What To Expect With Spinal Fusion Surgery
The thought of spinal surgery makes many people uncomfortable. The fear of having a major operation that could leave them bedridden and immobile keeps people from getting the care they need. However, spinal fusion surgery can provide much-needed relief if you are experiencing chronic back and leg pain. Knowing how to prepare and what to
Is It Time For Carpal Tunnel Surgery
Have you been diagnosed with carpal tunnel syndrome? If the answer is yes, and if it is getting worse or interrupting the completion of normal tasks, you might consider correcting it with surgery. Is it time for carpal tunnel surgery? Here are a few things to know if youre considering going under the knife. Carpal
Don’t Miss: Beginning Stages Of Parkinson’s Disease
Surgical Correction Of Kyphosis In Patients With Camptocormia Associated With Parkinsons Disease: A Case Report And Review Of The Literature
- 1Spine Department, Sichuan Province Orthopedic Hospital, Chengdu, China
- 2School of Basic Medicine, Chengdu University of Traditional Chinese Medicine, Chengdu, China
Background: Camptocormia is a postural deformity that is characterized by a markedly flexed lumbar spine, with symptoms that worsen with walking and standing. Here, we report a case of camptocormia associated with Parkinsons disease.
Case description: A 70-year-old man with a 7-year history of Parkinsons disease presented with a fall injury that caused lower back pain for 3 months and was aggravated for 2 months. He had been diagnosed with a compression fracture after the fall and had undergone percutaneous kyphoplasty at a local hospital. MRI showed non-union of the L1 vertebra and compression fracture of L2. The patient underwent posterior osteotomy, canal decompression, and internal fixation of the T10-L3 intervertebral plate with bone graft fusion. Postoperative examination showed that the lumbar lordosis was corrected and sensation was restored in both lower extremities. However, after 1 month, the fixation was loosened and a correction surgery was performed at our hospital. At the most recent follow-up at 1.5 years, the patient was found to be in good general health and did not complain of lower back discomfort. He was also actively exercising according to the rehabilitation regimen and had resumed social life.
Outcomes And Radiological Measurements
Data for age, gender, body mass index , disease duration from diagnosis of compression fracture to that of burst fracture and/or appearance of neurological symptoms, surgical procedures, and postoperative complications were acquired from medical charts. In patients with PD, the Hoehn & Yahr stage before surgery and at follow-up was assessed by senior neurologists. Clinical symptoms, low back pain, radicular leg pain, and cauda equine sign were also stratified based on cleft formation. Radicular leg pain was defined as lower extremity pain consistent with a neurological dominant region. Cauda equina syndrome was diagnosed based on symptoms of neurogenic intermittent claudication or motor and/or sensory disturbance, including bladder dysfunction. The Japanese Orthopaedic Association score for neurological status was obtained before surgery and at follow-up, with all neurological evaluations performed by senior spine surgeons. Neurological improvement rate at follow-up was calculated using the following formula: ×100/. Plain standing radiographs were used to identify other vertebral collapses, the type of vertebral collapse, lumbar lordosis and local lumbar lordosis before surgery and at follow-up.
Figure 3
Also Check: Parkinson’s Disease And Adhd
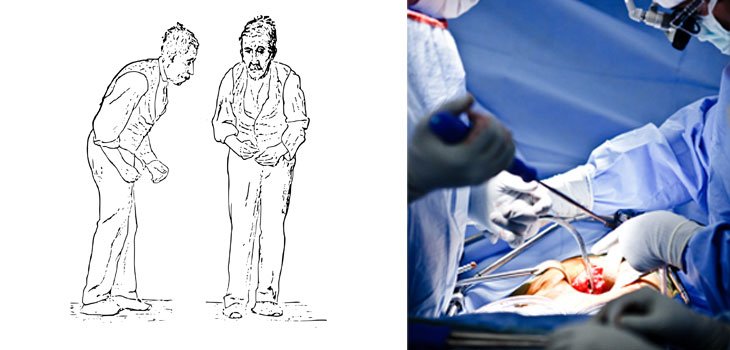
Case : Bilateral Stn Dbs
This patient was a 59-year-old man with advanced idiopathic PD and motor fluctuations. Preoperatively it was noted that he had severe camptocormia . He underwent placement of bilateral STN deep brain stimulators and a right chest dual channel pulse generator. He was discharged to an acute rehabilitation facility on postoperative Day 6 in good condition for several weeks after his hospitalization. At 2-year follow-up, his gait and ease of ambulation had improved, but he had no significant improvement in his camptocormia posture .
Case 1. Preoperative image of patient with severe camptocormia prior to DBS , and postoperative image obtained after DBS at 24-month follow-up .
How Deep Brain Stimulation Works To Treat Parkinsons Disease
Around 60,000 people in the United States are diagnosed with Parkinsons disease each year. This achronic motor system disorder leads to tremors, stiffness and difficulty with coordination and balance. Medication can help, but isnt enough for some patients. Deep brain stimulation can be an effective treatment for this debilitating disease. Read on to learn
Read Also: Parkinson’s Long Term Prognosis
Biography Of Charles J Malemud
Charles J. Malemud received the Ph.D. from George Washington University in 1973 and completed postdoctoral studies at the State University of New York at Stony Brook in 1977. Since 1977, Dr. Malemud has been a member of the faculty at Case Western Reserve University School of Medicine where he is presently Professor of Medicine & Anatomy in the Division of Rheumatic Diseases and Senior Investigator of the Arthritis Research Group. He has published over 230 papers, chapters and reviews primarily in the field of chondrocyte biology. Professor Malemud is on the editorial board of several rheumatology, immunology and musculoskeletal journals and is Editor-in-Chief of the Journal of Clinical and Cellular Immunology and Global Vaccines and Immunology.
Spinal Surgery In Patients With Parkinsons Disease

- George SapkasProfessor of Orthopaedics Orthopaedic Department Metropolitan Hospital, Neo Faliron Athens Greece
- Stamatios PapadakisDirector of the 2nd Orthopaedic Department K.A.T. Hospital, Athens Greece
- Michael PapadakisOrthopaedic Surgeon Orthopaedic Department Metropolitan Hospital, Neo Faliron-Athens-Greece
Also Check: How Does A Person Get Parkinson’s Disease