Parkinson’s Foundation Professional Talk Series: Interprofessional Care Team Approach To Cognitive Changes In Parkinson’s
Parkinsons Foundation Cognition Talk Series is a 7-part online course focusing on cognition concerns and challenges of living with Parkinsons disease. Each section of the series is presented by a specialized health professional discussing cognition from their viewpoint.
Audience: This activity is designed for neurologists, movement disorder specialists, neuropsychologist, primary care providers, nurse practitioners, physician assistants, nurses, pharmacists, physical therapists, occupational therapists, speech and language pathologists, social workers, and any other health care practitioner interested in learning more about the cognition concerns and challenges of living with Parkinsons disease.
Free or Fee: $29.99 to receive CMEs/CEUs | Free with no CMEs/CEUs awarded
CME Credit: Oakstone Publishing designates this enduring material for a maximum of 3.5 AMA PRA Category 1 Credits. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
This activity has been planned and implemented in accordance with the accreditation requirements and policies of the Accreditation Council for Continuing Medical Education through the joint providership of Oakstone Publishing and The Parkinson Foundation. Oakstone Publishing is accredited by the ACCME to provide continuing medical education for physicians.
Register Here:Register Now
For more information on online courses for Care Partners and People living with Parkinsons disease, .
Protect People With Parkinson’s By Screening And Monitoring Them Throughout Their Treatment
Tracey:
It is our responsibility as nurses and clinicians to ensure that we ask our patients at every clinic appointment if they are experiencing any impulsive or compulsive behaviours and to document that conversation.
Stephen:
Impulsive and compulsive behaviour side effects destroyed my life. It took me from being a career person with a great lifestyle to living homeless on the streets of London in less than 14 months.
It all could have been prevented if I had been pre-screened for suitability for the medication and I’d been monitored whilst taking the medication.
Availability Of Data And Materials
On the consent form, participants will be asked whether they agree with the following statement: I know that participating in this trial is voluntary. I also know that at any time I can decide to withdraw from the trial. I do not have to give any reason. The data that is collected until that moment, will be used for the research. A number of people are allowed to view my data. These include the members of the research team, the Ethical Committee, people that verify the safety of the trial , and the Dutch Healthcare Inspection.
This trial does not involve collecting biological specimens for storage. The aggregated datasets analyzed during the current study will be available from the corresponding author upon reasonable request.
Also Check: Can Mold Cause Parkinson’s Disease
Training And Coaching Of Parkinsons Disease Nurse Specialists
Before the start of the study, we will organize a single training session with all participating PDNSs . The goal of this meeting is to acquire commitment to the study and uniformity in workflow by reviewing the Nursing care in Parkinsons disease guideline to explain the study specifics and to discuss practical issues related to the study intervention. In addition, PDNSs will be closely coached in order to optimize the intervention and adherence to the guideline. Every month, an experienced PD nurse from Radboudumc will have an individual intervention session with each PDNS, mainly to discuss difficult cases and to optimize the intervention and its uniformity. Finally, we will organize a video meeting every 3 months with all PDNSs to maintain their commitment, support each other, discuss difficulties related to the study, and give each other advice .
Importantly, for the purpose of this study, we will implement an increase in nursing staff capacity for participating nurses. This will allow us to study the real impact of current usual care, which would not be achieved by adding a new set of specifically trained research nurses to the existing PDNS staff. The PDNSs are all graduated nurses with a certificate in Parkinsons nursing. Furthermore, they have achieved a standard of competence as described in the Nursing care in Parkinsons disease guideline .
Complications Of Parkinsons Disease
You May Like: How Close To A Cure For Parkinson’s
Imbalanced Nutrition Less Than Body Requirements
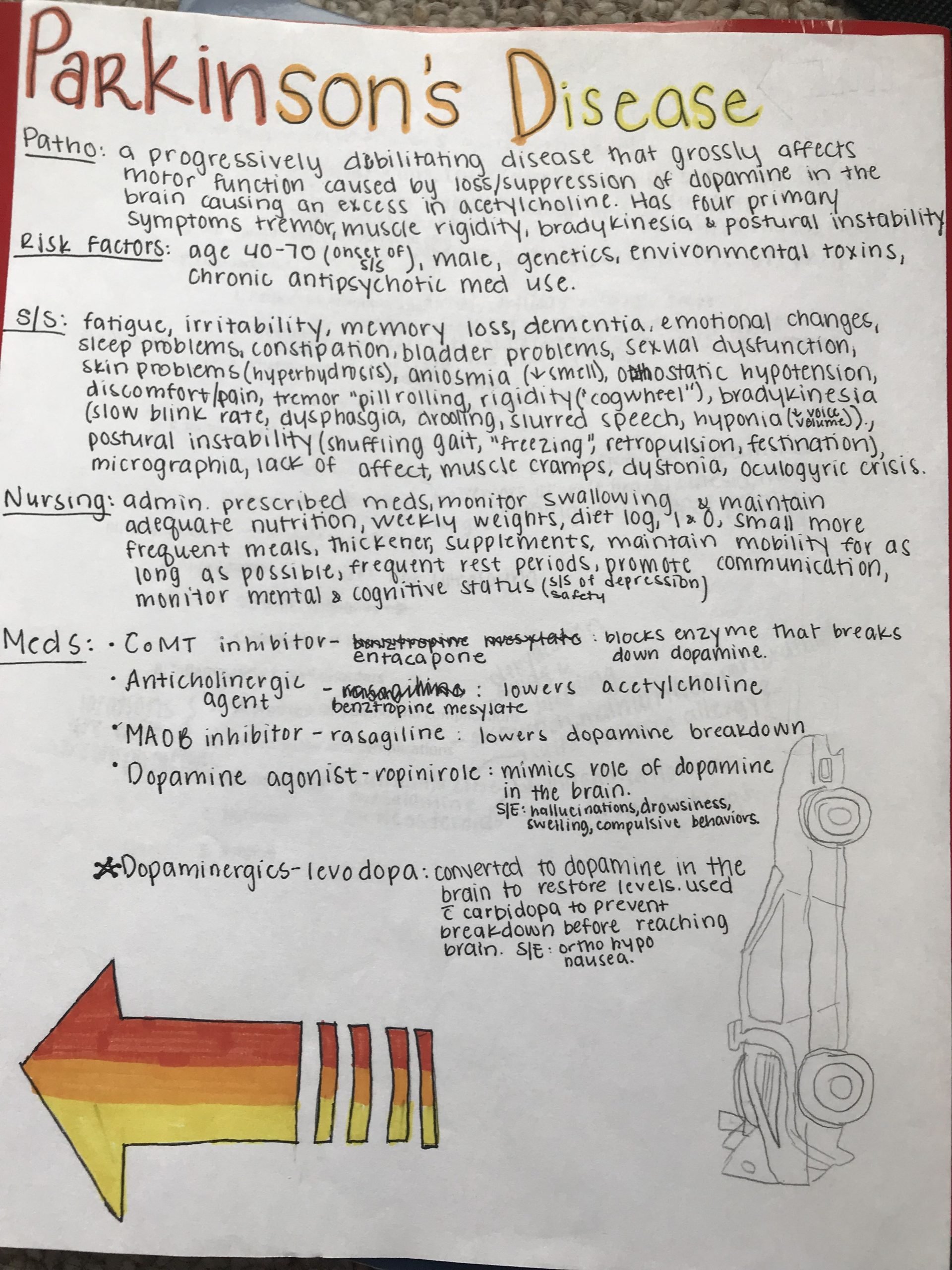
In Parkinson’s disease, tremors, bradykinesia, and impaired chewing and swallowing contribute to imbalanced nutrition, with fewer calories than the body requires. The nursing assessment may note declining food intake and weight loss.
Monitoring weight weekly is recommended. The ongoing nursing assessment also evaluates the patient’s ability to feed himself/herself, helping to determine when family/caregiver supervision as needed.
The patient should be in a sitting position when eating or drinking. A good general diet high in fiber is recommended, if the patient is able eat such foods. Soft or pureed foods may be easier to swallow.
Recommend taking small bites of food, then swallowing twice or more after each bite. Thin liquids may be difficult to swallow and cause aspiration thickened liquids may be easier. Allow sufficient time for meals. Small frequent meals may be beneficial.
Teach patients and caregivers eating techniques that may decrease tremor . Using stabilized dishes and utensils or other adaptive equipment for eating can be helpful, and occupational therapy may be a good resource for patients and families.
High calorie supplements between meals may be appropriate. A referral to a dietician may be helpful for recommendations on meeting nutritional and caloric requirements and providing food of the most appropriate consistency. A swallowing consultation may be helpful if the patient has swallowing problems .
Benefits Of The Drugs
Tracey:
The benefits of the drugs that can trigger off impulsive and compulsive behaviour can be huge for some patients and I think that is what is very, very important that when you are talking to someone prior to them starting it that you don’t scare them.
These can be extremely beneficial, appropriate, useful drugs which can enhance a person’s life greatly and make a huge, huge difference to them.
You May Like: Nursing Management Of Parkinson’s Disease
What Is Impulsive And Compulsive Behaviour
Tracey Ward, Parkinson’s Specialist Nurse:
Impulsive and compulsive behaviour is where a person feels a drive to do something where in their usual insight they may feel that’s not appropriate. But they actually lose that sense of holding back and so something takes over and impulsively drives them towards that situation.
So they actually lose the ability to control their behaviour in a way in which they would normally do so.
Stephen, diagnosed in 2001:
It started with gambling, hypersexuality, just generally anything that involved risk-taking. At the time of carrying out the behaviours, it was less about the activity and more about the excitement and the thrill.
Dr Nin Bajaj, Consultant Neurologist:
Impulsive behaviours can manifest in a variety of ways. In some people they can be very subtle. Some people just start doing hobbies that they always did a bit more often.
Beyond that, there are varieties of behaviour which cause more concern. We’ve had patients who start to shop obsessively and start to spend very large amounts of money. We’ve had others who start to gamble.
We also see a change in sexuality in patients – some patients become hypersexual and that causes difficulties in their relationship with their spouse.
So you must see impulsive and compulsive behaviour as a very broad spectrum of behaviours, from fairly mild behaviour that can be tolerated, to extremes of behaviour, which can be very detrimental to a relationship and to an individual.
Individual State Behavioral Health Approvals
In addition to states that accept ASWB, NetCE is approved as a provider of continuing education by the following state boards: Alabama State Board of Social Work Examiners, Provider #0515 Florida Board of Clinical Social Work, Marriage and Family Therapy and Mental Health Counseling, CE Broker Provider #50-2405 Illinois Division of Professional Regulation for Social Workers, License #159.001094 Illinois Division of Professional Regulation for Licensed Professional and Clinical Counselors, License #197.000185 Illinois Division of Professional Regulation for Marriage and Family Therapists, License #168.000190
You May Like: Best Walking Cane For Parkinson’s
Other Motor Symptom Medications
- Amantadine hydrochloride
Amantadine is an anti-viral drug that was developed in the 1960’s to treat influenza. It was found coincidentally to decrease the symptoms of Parkinson’s disease and levodopa-induced dyskinesias. It is not clear how amantadine works to improve the symptoms of Parkinson’s disease. It can be used alone in the early stages of Parkinson’s disease, especially to help those with tremor, or combined with anticholinergic drugs or levodopa. Amantadine seems most beneficial for people with Parkinson’s disease who have prominent tremor or levodopa-induced dyskinesias. The effectiveness of amantadine seems to wear off after several months for about half the patients taking this drug.
What Health And Care Tips Can You Give To Someone With Parkinsons
My top tips would be:
- Invest in a medication timer, or use your mobile phone. Set 2 alarms each time your medication is due this helps make sure you never miss a dose.
- Use a sealed cup for carrying drinks around the home it ensures you dont spill anything and means you can concentrate more on walking.
- If its safe, use a steak knife for cutting up any food. This helps if you find it hard to use pressure when using cutlery.
- Stay as active as you can exercise helps in so many ways, both physically and mentally.
Please tell us everything so we can help you. Some people come to see us not wanting to bother us, but thats what were here for.
Don’t Miss: How Hereditary Is Parkinson’s Disease
Risk For Falls And Injury
With Parkinson’s disease, bradykinesia, rigidity and tremors can lead to gait problems and a risk for falls and injury.
The nursing assessment includes evaluating the patient’s movement and gait and understanding his/her home environment. Improving movement and gait can reduce the risk of falls .
To promote safety and avoid falls, suggest removing potential hazards in the home, such as loose rugs or obstacles in pathways. Recommend handrails on both sides of stairways, non-skid surfaces and grab rails in showers and tubs, and raised toilet seats. Suggest that patients with Parkinson’s disease wear appropriate shoes with smooth, non-slippery soles. Encourage the family or caregiver to supervise ambulation, as needed. A bedside urinal or commode may be helpful for some patients to prevent nighttime falls.
Some patients with Parkinson’s disease experience orthostatic hypotension. If patients become dizzy when moving from a lying to a standing position, teach them to rise slowly, to remain seated for a few minutes with legs dangling over the side of the bed and flex feet upward, to then stand but sit back down immediately if they feel dizzy. Recommend having someone with them when they stand up.
Review medications, as some anti-Parkinson’s drugs may cause dizziness these can be discussed with the physician to see if alternative medications might be beneficial.
Including Families And Carers In The Conversation
Nin:
It’s always important to include a spouse or partner in discussions about impulse control disorder. The main reason is that the patient is not aware of these behaviours. They’re not doing it on purpose. Often they’re the last to know. These are subconscious behaviours.
So it’s vital to have a spouse involved right from the start, because in a sense, they’re the clinician’s eyes and ears on the ground – they’re the people who are going to tell you if there’s a disorder, because patients are often the last people to tell you about it.
You May Like: Is Massage Good For Parkinson’s
The State Of Nursing Education On Parkinson’s Disease
When I was offered a job to help start a Parkinsons Disease Center in 1981, I knew I loved the concept, but also knew nothing about Parkinsons disease. My masters in community health education would serve me well in the job aspects of outreach, forming support groups, working with community advocates, and providing educational programs, but what about the knowledge I needed on the complexities of Parkinsons disease?
I searched my textbooks and notes from nursing school, hoping to get a start on my learning before the first day on the new job. I found one sentence in my notes, and no content on PD in my nursing texts. That one sentence was simply levodopa, new drug, watch for it! As there was no nursing information on Parkinsons disease, I devoured a book for people with Parkinons written by Roger Duvoisin, MD.
The scholars of the Edmond J. Safra Visiting Nurse Faculty Program at the Parkinsons Foundation are excitedly looking forward to WPC 2019. We hope to see you there and bring even more nurses with us!
_______________________________________________________________________________
Ideas and opinions expressed in this post reflect that of the authors solely. They do not reflect the opinions or positions of the World Parkinson Coalition®
What Does A Parkinson’s Nurse Do
Parkinson’s Nurses work on providing professional support to people living with Parkinsons.
To do so, our nurses develop high-quality medical plans while also providing in-depth information about Parkinson’s.
To help families further, Parkinson’s Nurses will connect people with Parkinsons to speech therapists, occupational therapists, and physiotherapists.
Parkinson’s NZ also runs networking support groups and exercise classes. We also offer physiotherapy, hydrotherapy, as well as art/music therapy sessions to members.
Don’t Miss: Movie Stars With Parkinson’s Disease
Causes Of Parkinsons Disease
Parkinsons disease is an idiopathic illness, which means that its cause is unknown.
The signs and symptoms it present are caused by the loss of nerve cells in the part of the brain called substantia nigra.
This part of the brain is responsible for the production of dopamine, a neurotransmitter that links the brain and nervous system to coordinate body movements.
Loss of dopamine results in uncoordinated body movements, thereby producing the signs and symptoms of the disease.
Though the exact cause of Parkinsons disease is still unknown, there are possible explanations that may be responsible for the condition, such as:
- Genetics. Studies have shown that a minority of cases of PD have genetic involvement.
- Environmental factors. Exposure to pesticides, herbicides, and industrial pollution is now being looked at as a possible cause of PD. However, the results are still inconclusive.
- Presence of Lewy bodies. Lewy bodies are clumps of substances in the brain cells. These are often seen in people with Parkinsons disease. The studies about them are still inconclusive, but researchers believe that these substances hold useful information to what causes PD. Researchers are also focusing into alpha-synuclein found in the Lewy bodies.
The following are the associated risk factors in developing Parkinsons disease:
Monoamine Oxidase B Inhibitors
- Selegiline hydrochloride
- Rasagiline mesylate
The enzyme monoamine oxidase B breaks down dopamine in the brain. MAO-B inhibitors prevent this breakdown, thus increasing the amount of dopamine in the brain and reducing the motor symptoms of Parkinson’s disease.
MAO-B inhibitors used to treat the symptoms of Parkinson’s disease, either alone or with levodopa. In early Parkinson’s disease, they can delay the need for starting levodopa. Later in the disease, they can be given with levodopa, to enhance and prolong the effects to levodopa, thus reducing the “wearing off” phenomenon. When taken in combination with levodopa, it may allow the dose of levodopa to be reduced.
Side effects of MAO-B inhibitors include nausea, dizziness, headache, confusion, postural hypotension, hallucinations and insomnia. Confusion and hallucinations are more common in the elderly.
MAO-B inhibitors should not be used with meperidine or other opioids because of potential life-threatening drug interactions at high doses. MAO-B inhibitors at high doses could also potentially precipitate a hypertensive crisis if very large amounts of tyramine containing foods are eaten. Serious drug interactions have been reported with MAO-B inhibitors and some antidepressants.
Selegiline and azilect are available are available as standard oral tablets. An oral disintegrating selegiline tablet is also available for people who have difficulty swallowing tablets.
Read Also: Does Weed Help With Parkinson’s
Other Ereaders Or Your Computer
To download this course to your computer, please follow these instructions:
If you are transferring to an eReader:
External Link
This link leads outside of the NetCE site to:
While we have selected sites that we believe offer good, reliable information, we are not responsible for the content provided. Furthermore, these links do not constitute an endorsement of these organizations or their programs by NetCE, and none should be inferred.
How Can Someone Best Prepare For An Appointment With Their Parkinsons Nurse
Our region was one of the early adopters of video calls as coronavirus first hit, and its still something were using. Whether you have a video, phone or face-to-face appointment, there are always things that will make an appointment run smoother.
Its always good to think about your top 3 issues relating to Parkinsons. What is bothering you at the moment? What is difficult?
Its helpful to have a list of drugs youre taking, or even bring your medication along if its a face-to-face appointment.
Please bring someone close to you if you like this is helpful for both parties.
And be honest with us! Please tell us everything so we can help you. Some people come to see us not wanting to bother us, but thats what were here for.
- The process for accessing a nurse is different depending on where in the UK you live. In some areas you can self-refer, or you may have to be referred through your GP or specialist. Try asking your GP surgery as a first point of call. If you have any problems or would like to find out more, please contact our helpline on 0808 800 0303 or email
You May Like: New Parkinson’s Medication For Hallucinations