Living With Parkinson’s Disease
Coming to terms with a diagnosis of Parkinson’s and living with the disease is challenging and will take a lot of adjustment. There are still things you can do that can help you to feel more in control of your situation and to stay positive. Some things that might help could include:
- choosing to lead a healthy lifestyle
- making informed decisions related to your treatment
- keeping a diary of your symptoms in preparation for meetings with health and social care professionals
- attending a self-management course
What Has Changed In The Treatment Of Advanced Parkinson Disease
In advanced Parkinson disease, the efficacy of levodopa can decline and fluctuate throughout the day switching between on and off medication periods.92 The motor and nonmotor fluctuations mirror those seen in levodopa plasma concentrations resulting from levodopas short half-life.93 Providing continuous dopaminergic stimulation is the goal of treating fluctuations in patients with advanced Parkinson disease.9496 We now have surgical options, including deep brain stimulation and levodopacarbidopa intestinal gel, to provide treatment to such patients. Currently, deep brain stimulation has the highest level of evidence with the largest number of randomized controlled trials.97 Emerging therapies currently being studied in Parkinson disease are listed in Appendix 7, available at www.cmaj.ca/lookup/suppl/doi:10.1503/cmaj.151179/-/DC1.
Is There Anything I Can Do To Slow The Progression Of Parkinsons Symptoms
Treatment for Parkinsons can help you manage your symptoms. Currently, theres no way to cure or stop the progression of Parkinsons. However, medical professionals have found ways to slow the progression of symptoms with therapies such as medications and deep brain therapy.
Diet and exercise are also known to slow down Parkinsons. Studies have shown that eating a nutritious diet, such as the Mediterranean diet, can help slow down the progression of Parkinsons disease.
Additionally, getting regular exercise has been shown to slow down symptom progression. People with Parkinsons should try to get at least 2.5 hours of exercise each week. A physical therapist or another medical professional can help you develop an exercise routine that meets your needs.
Also Check: What Part Of The Brain Does Parkinson’s Disease Affect
Deep Brain Stimulation Surgery
As Parkinsons disease progresses, deep brain stimulation surgery may become an option. Our team is one of the most experienced in the United States. Under the direction of Dr. Delaram Safarpour, Dr. Kim Burchiel, an OHSU neurosurgeon, pioneered asleep DBS so you dont have to be awake during surgery.
For this procedure, our team places tiny electrodes in your brain. The electrodes are connected to a small pacemaker-like device placed under the skin of your chest. The device sends mild electrical pulses to regulate movement and control Parkinsons symptoms such as:
In some parts of the state, you can have follow-up care at a doctors office in your community.
Colin Halstead had deep brain stimulation surgery at OHSU to treat his Parkinsons. It gave me my life back, he says.
Passive Manipulation Of Limbs
To test for the presence of rigidity, we need to passively manipulate the limbs of the patient. However, If the disease is in its early stage or the symptoms are well controlled with medications, we may not be able to see rigidity. We will need to use some activation maneuvers, that basically consist in performing repetitive movements with the limb contralateral to the one that is being tested.
Also, there are two types of rigidity:
– Lead-pipe rigidity: where the tone is uniformly and smoothly increased throughout the entire range of movement
– Cogwheel rigidity: where a tremor is superimposed on the hypertonia, making the movement irregular due to intermittent increase and reduction of tone
Upper Extremity Testing
For the upper extremity the most sensitive joint where to check for rigidity is the wrist. To uncover rigidity, passively rotate the wrist and feel for a resistance to the movement. It is very important that the arm of the patient is fully relaxed when rotating the wrist. To do this, place your proximal hand under the patients forearm, while your distal hand grabs and rotates the wrist of the patient. When rigidity is present, the range of motion will be preserved but you will feel a resistance in performing the movement.
Wrist rotation with activation maneuver.
It is also possible to test for rigidity in the elbow by passively flexing and extending the forearm.
Elbow flexion-extension with activation maneuver.
Lower Extremity Testing
Don’t Miss: New Treatment Options For Parkinson’s Disease
How Is Parkinson’s Diagnosed
Current evidence suggests that Parkinsons tends to develop gradually. It may be many months, even years, before the symptoms become obvious enough for someone to go to the doctor.
This information looks at what parkinsonism is, how Parkinsons and other similar conditions may be diagnosed, and explains some of the tests that may be involved in the process.
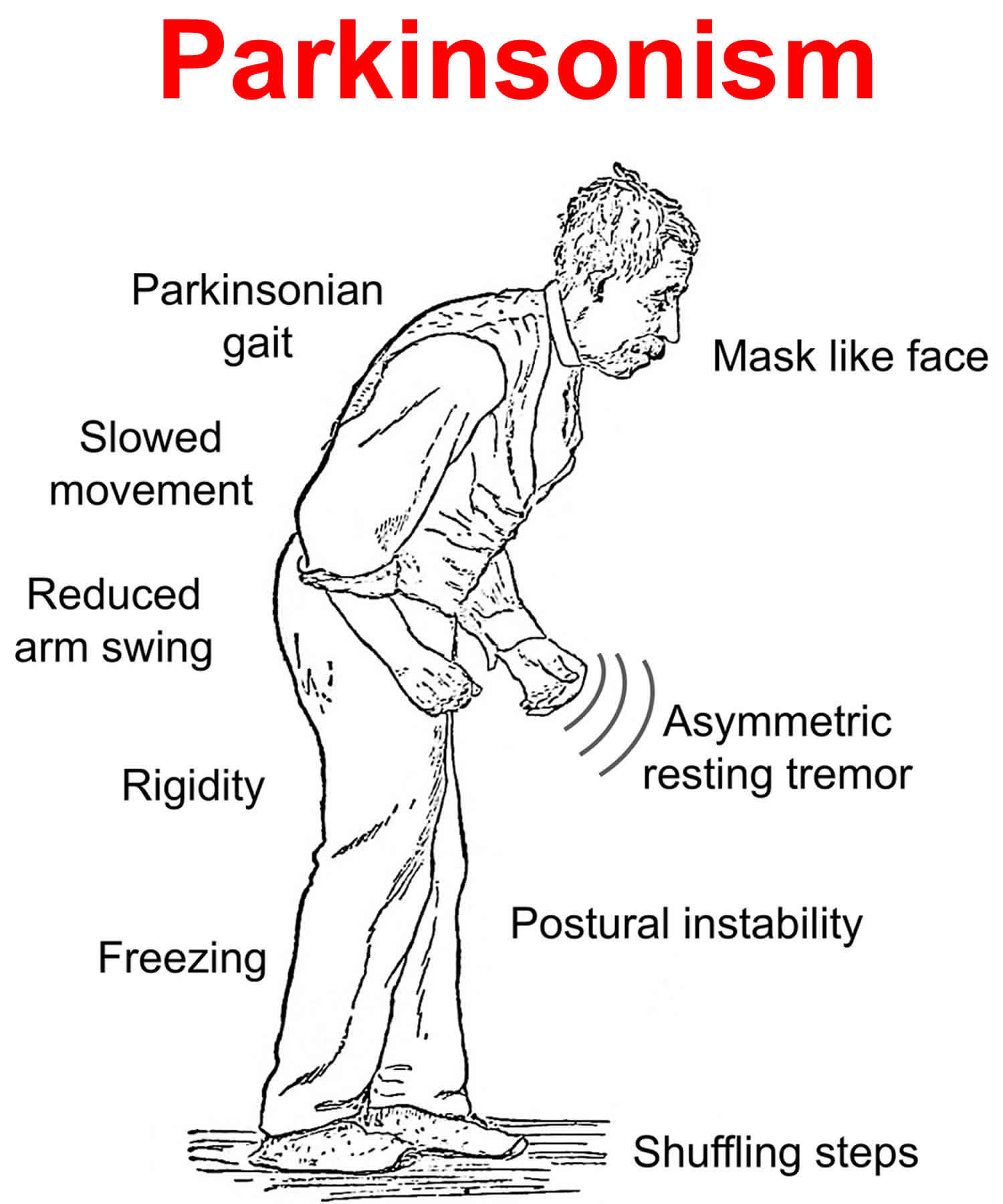
Parkinsonism is a term used to describe symptoms or signs that are found in Parkinsons, but which can also be found in other conditions that cause slowness of movement, stiffness and tremor.
Most people with a form of parkinsonism have idiopathic Parkinsons disease, also known as Parkinsons. Idiopathic means the cause is unknown.
Other less common forms of parkinsonism include multiple system atrophy , progressive supranuclear palsy , drug-induced parkinsonism and vascular Parkinsons.
If youre concerned about symptoms youve been experiencing, you should visit your GP. If your GP suspects you have Parkinsons, clinical guidelines recommend they should refer you quickly to a specialist with experience in diagnosing the condition .
Its not always easy to diagnose the condition. So its important that you see a Parkinsons specialist to get an accurate diagnosis and to consider the best treatment options.
Diagnosing Parkinsons can take some time as there are other conditions, such as essential tremor , with similar symptoms. There is also currently no definitive test for diagnosing Parkinsons.
Determining Diagnosis Through Response To Parkinsons Medication
If a persons symptoms and neurologic examination are only suggestive of Parkinsons disease or if the diagnosis is otherwise in doubt, the physician may, nevertheless, prescribe a medication intended for Parkinsons disease to provide additional information. In the case of idiopathic Parkinsons, there is typically a positive, predictable response to Parkinsons disease medication in the case of some related Parkinsonian syndromes, the response to medication may not be particularly robust, or it may be absent entirely.
Unfortunately, there are no standard biological tests for the disease, such as a blood test. However, researchers are actively trying to find biomarkers in blood and other bodily fluids that could help confirm the diagnosis.
Recommended Reading: Can Anxiety Cause Parkinson’s Disease
Who Gets Parkinson Disease
The exact cause of Parkinson disease is unknown, but it is assumed to be the result of a combination of environmental influences superimposed on genetic predisposition or susceptibility .1416 There is increasing evidence that the genetic and environmental insults leading to Parkinson disease commonly lead to abnormal forms of a normal protein, -synuclein, which seems to contribute to cell death.16,23 The onset of Parkinson disease can be categorized as juvenile , early onset and late onset .24,25 The juvenile form is rare, is often familial , is most frequently associated with a parkin gene mutation and has an atypical presentation.25,26 Of patients with Parkinson disease, 10%16% have an affected first- or second-degree relative first-degree relatives may have double the risk of Parkinson disease compared with the general population.2629 In early- and late-onset Parkinson disease, the frequency of a positive family history is not statistically different.24
Medical History And Physical Exam
The process of diagnosing Parkinsons usually begins with the neurologist evaluating your medical history and performing a physical exam. For a formal diagnosis to be made, you need to have a general slowness of movement with either a resting tremor or rigidity.
During the physical exam, your doctor will have you perform a series of tests to monitor your movement. An example of a test they might use is a finger tap, where they measure how many times you can tap your finger in 10 to 15 seconds.
They will also look for signs that you may have another condition. A group of movement disorders collectively called parkinsonisms can produce symptoms that are indistinguishable from those of Parkinsons but are not the same. Usually, additional tests are needed to rule out these conditions as well.
You May Like: Parkinson’s And Autonomic Dysfunction
What Are The Symptoms
Each person is affected differently by Parkinsons disease and no two people will experience exactly the same symptoms. The impact of Parkinsons disease can be unpredictable and it is common for people to have good days and bad days.
The main symptoms of Parkinsons disease are:
- balance problems
- problems with posture
Other possible symptoms include difficulty initiating movement , a shuffling gait when walking, and freezing when trying to move . People might experience a loss of facial expression, speech problems , swallowing problems, bowel and bladder problems, difficulties at night and tiredness during the day. Skin can become greasy and people might experience excessive sweating. Sexual problems are common. People often experience depression and anxiety. Another common symptom is small handwriting .
Other less common symptoms can include pain and memory problems.
How Parkinsons Disease Is Diagnosed
Parkinsons disease is usually diagnosed clinically, meaning that a physician looks for the presence or absence of the possible symptoms of Parkinsons disease by interviewing the patient and performing a detailed neurologic examination.
While there is presently no definitive test for Parkinsons, it can often be identified by a general neurologist, who is trained to diagnose and treat neurologic disorders. To avoid misdiagnosis, consultation with a movement disorder specialist is recommended. A movement disorder specialist is a physician who has undergone additional, subspecialty training in the diagnosis and treatment of movement disorders, such as Parkinsons, after training in general neurology.
What to expect during your visit with a physician
Typically, a trained physician will only consider the diagnosis of Parkinsons disease if the person being examined has at least two of the core motor symptoms of Parkinsons, including tremor, the characteristic bradykinesia , or rigidity. At the end of your visit, the physician should discuss with you why you may or may not have Parkinsons disease and the level of certainty about the diagnosis. This determination is based on your medical history and examination at this visit.
Brain imaging and other tools to aid diagnosis of Parkinsons
Don’t Miss: Medical Alert Bracelets For Parkinson’s Disease
Pd Diagnosis Disease Severity And Disease Progression
The diagnosis of PD is essentially clinical , and we believe that the clinical evaluation of patients will not be replaced by modern imaging techniques. Nevertheless, as pointed out earlier, misdiagnosis can approach 20% of cases . Recently, in line with the European Union, the U.S. FDA approved DAT scan as a diagnostic tool to help differentiate between PD and Essential Tremor. This is the only current FDA-approved subsidiary examination to aid in PD diagnosis.
The role of magnetic resonance imaging in the diagnosis of PD is still not fully established. Traditionally, it has been seen as a means to potentially exclude alternate diagnoses such as vascular parkinsonism, or more importantly , atypical forms of degenerative parkinsonism such as MSA or progressive supranuclear palsy . Traditional structural MRI findings of these latter diagnoses such as increased pallidal iron, rim of putaminal hyperintensity, hot cross bun sign and/or cerebellar atrophy in MSA or the hummingbird or penguin sign in PSP may not be reliable, particularly in early disease.
Figure 5. Multimodal MRI in PD. Differences are noted between patients with PD and controls through voxel-based analysis of R2, mean diffusivity, and fractional anisotropy maps.
-
Low dopamine transporter uptake in basal ganglia demonstrated by SPECT or PET imaging.*
Brent A. Vogt, in, 2019
What Are The First Symptoms Of Early Onset Parkinsons And When Should I See A Doctor
There are some early warning signs associated with Parkinsons. These symptoms dont always mean a person will develop Parkinsons but can be a signal that its very likely. Symptoms that can act as early warning signs include:
- speaking very quickly
- difficulty writing and changes to handwriting
Its a good idea to talk with a doctor about any early warning signs symptoms or early symptoms of Parkinsons you experience.
You May Like: What Symptoms Of Parkinson’s Disease Does Levodopa Help
What Tests Or Investigations Are Available To Help With Diagnosis
Parkinson disease is a clinical diagnosis, and magnetic resonance imaging may be used only to exclude other causes, as listed in Appendix 1. Advancements in neuroimaging studies, including transcranial Doppler ultrasonography,51 positron emission tomography , single-photon emission computed tomography , morphometric MRI studies, tractography, functional MRI and perfusion imaging are being used to differentiate idiopathic Parkinson disease from other parkinsonian disorders.52,53
Radionuclide imaging modalities like PET and SPECT, using a dopamine transporter ligand, have become the best approach to assess dopamine metabolism and deficiency. Tracer uptake is reduced maximally in the posterior or dorsal striatum and is asymmetric in Parkinson disease.52,53
A subgroup of patients suspected of having new-onset Parkinson disease will have no evidence of dopaminergic deficit on dopamine transporter SPECT and fluorine-18 fluoro-L-dopa PET imaging scans.54 In this group of patients, progression of disease, by imaging or clinical measures, is minimal, as is their likelihood of developing idiopathic Parkinson disease.54 However, a few may eventually be diagnosed with Parkinson disease, based on clinical progression, imaging and genetic evidence and a positive response to levodopa.55
There are currently no biomarkers of proven clinical utility. Cerebrospinal fluid levels of -synuclein may predict cognitive decline but do not correlate with motor progression.56
What Is The Prognosis
Life expectancy is decreased in Parkinson disease , and medical treatments do not appear to alter mortality or delay the onset of nonmotor symptoms.114 Although progression is slower in patients with early-onset disease and there is longer absolute survival, this comes at the expense of increased years of life lost .24,115 Late-onset Parkinson disease is associated with more rapid disease progression and cognitive decline,116 which may be related to a lack of compensatory strategies against cell death.24 Data on the long-term outcomes and in the older population are lacking.117
Prognostic factors are summarized in Table 4. Patients with early-onset disease were slower to reach stage IIIV on the Hoehn and Yahr scale119 . The distribution of Hoehn and Yahr staging according to disease duration is listed in Appendix 8b. In the Rotterdam Study, Parkinson disease was associated with an increased risk of dementia and increased risk of death . When dementia prevalence was controlled for, risk of mortality was only slightly higher than among the general population.120
Read Also: Do Parkinson Patients Shake During Sleep
What Doctors Look For When Diagnosing Parkinsons
Certain physical signs and symptoms noticed by the patient or his or her loved ones are usually what prompt a person to see the doctor. These are the symptoms most often noticed by patients or their families:
-
Shaking or tremor: Called resting tremor, a trembling of a hand or foot that happens when the patient is at rest and typically stops when he or she is active or moving
-
Bradykinesia: Slowness of movement in the limbs, face, walking or overall body
-
Rigidity: Stiffness in the arms, legs or trunk
-
Posture instability: Trouble with balance and possible falls
Once the patient is at the doctors office, the physician:
-
Takes a medical history and does a physical examination.
-
Asks about current and past medications. Some medications may cause symptoms that mimic Parkinsons disease.
-
Performs a neurological examination, testing agility, muscle tone, gait and balance.
The Diagnosis Of Idiopathic Parkinsons Disease
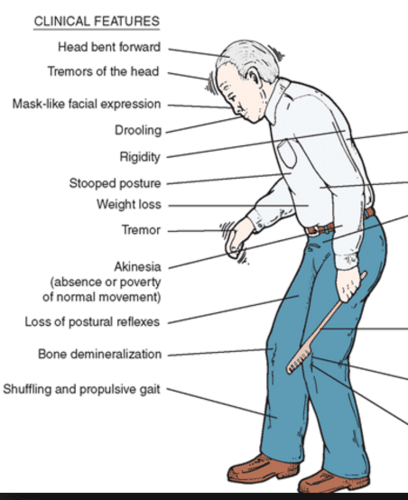
The first component to the diagnosis of PD is establishing that the patient has parkinsonism. This is a clinical diagnosis and relies on three key elements: bradykinesia, tremor, and rigidity. Of these, bradykinesia must be present, with at least one of the other two. PD is an asymmetrical condition, so during the clinical assessment, the parkinsonism should be more apparent on one side and may be purely unilateral in early disease . is a classical illustration of parkinsonism, with a description by William Gowers.
A case of Parkinsons disease as described and illustrated by William Gowers: the aspect of the patient is very characteristic. The head is bent forward, and the expression of the face is anxious and fixed, unchanged by any
Don’t Miss: Dbs Device For Parkinson’s
Dementia With Lewy Bodies
Dementia with Lewy bodies is the second most common cause of dementia, following Alzheimers disease. It is characterized by progressive cognitive impairment together with fluctuating levels of attention, visual hallucinations, REM sleep behavior disorder, and parkinsonism. The predominant pathology in both PD and DLB is Lewy bodies, the main constituent of which is -synuclein, and there is undoubtedly a clinical and pathological overlap. Current diagnostic criteria state that if the cognitive symptoms pre-date or develop within the first year of the emergence of parkinsonism, then the diagnosis is DLB. Should cognitive impairment develop in the context of established PD, then the diagnosis is Parkinsons disease dementia .
The cognitive impairment of DLB affects attentional-executive and visuospatial functions. Patients typically perform poorly on the Stroop and the trail-making tasks as well as drawing tasks, classically clock-drawing or intersecting pentagons . Fluctuating attention can manifest as inconsistent behavior and periods of zoning-out, and in fact, the presence of major fluctuations in a patients cognitive state is a very helpful diagnostic feature of this condition. The visual hallucinations that occur in approximately 80% of patients are complex and tend to involve humans or animals. Patients have a variable amount of insight into their presence .