Top Patient Complaint About Dbs Device: Ineffective Stimulation
Now, researchers at Vanderbilt University Medical Center, in Tennessee, where the trial took place, reported five-year results regarding medication costs. They also projected such costs through 15 years to reflect the mean time for Parkinsons to progress from early to advanced stages the time when a typical patient may be offered DBS.
Data from motor symptom-targeting medications, collected at each visit, were used to calculate and project medication costs.
The analysis included 28 participants who completed at least one follow-up visit. They had a mean age of 61.1 and had lived with the disease for a mean of 2.1 years at study entry.
The results showed that the mean annual Parkinsons medication cost had increased from $4,941 at the studys start to $14,177 after five years for patients receiving standard medication alone. For the DBS group, the costs increased from $4,507 to $6,636.
This represented a 2.4 times lower annual medication cost and a five-year cumulative cost reduction of $28,246 for patients receiving both DBS and standard medication relative to the control group.
Patients originally assigned to medication alone also were five times more likely to have higher medication costs than those in the DBS group.
In addition, annual medication costs at 15 years using 10% annual cost increases to account for disease progression were projected to reach $30,371 for the control group and $14,216 for the DBS group.
The Future Could Hold Even Bigger Innovations In Dbs
I hope mostly that we are learning to treat patients better, says Dr Stieglitz. Maybe in the future we could even learn how to do multi-target stimulation. In the future we might have the technology and also the knowledge to influence complex networks in the brain in a more sophisticated way.
But Dr Stieglitz feels the first priority should be making DBS therapy available to more people with Parkinsons disease. I hope that more patients will benefit from deep brain stimulation. This is the first thing not to improve the treatments for a few patients, but to bring the treatments to more people in need, he says. I believe in the future of DBS.
Medtronics Percept PC neurostimulator with BrainSense technology.
Find out more about Medtronic DBS therapy for Parkinsons disease.
At a glance: benefits of the Percept PC neurostimulator
- It can continuously sense and record brain signals, allowing clinicians to track patient-specific signals and correlate these with patient-recorded events
- Its the only DBS system that is compatible with 3T full-body MRI scans*, meaning it can be left on with certain stimulation configurations while the scans take place
- It incorporates low pulse width, providing expanded stimulation options
- It has improved battery longevity** and a comfortable new shape
- It has an enhanced Patient Programmer*** through a custom-configured Samsung mobile device, allowing patients to manage their therapy more easily.
Need to know
Footnotes
Research To Improve Deep Brain Stimulation
Researchers are working to improve upon existing DBS devices and methods to help treat more symptoms and more people. Some researchers are putting electrodes in a different area of the brain the pedunculopontine nucleus to treat walking and balance problems that don’t typically improve with present-day DBS. Others are developing a “smart” DBS device that can record a person’s unique brain signals and deliver electrical stimulation only when needed, such as when symptoms return, rather than continuously, as the current systems do. This could help reduce side effects such as numbness and weakness and lengthen the battery life of the neurostimulator, which would result in a longer time between battery replacement procedures.
Scientists also are planning to test deep brain stimulation in the first years after a Parkinson’s diagnosis to see if the therapy may slow or stop disease progression. Testing in Parkinson’s models showed the therapy may help protect brain cells, and a small human trial showed motor symptoms improved after early-stage DBS.
You May Like: Best Stationary Bike For Parkinson’s
Global Dbs Devices Market For Parkinsons Disease $57 Billion By 2027
The global market for deep brain stimulation devices for Parkinsons disease estimated to reach $5.7 billion by 2027, growing at a CAGR of 8.5% over the forecast period, driven by increasing prevalence and incidence rates of the disease and technological advances in the device-assisted therapy area.
Parkinsons disease affects an estimated one million Americans including men and women of all ages and races, though it is slightly more common in men.
- Parkinsons is caused by a combination of genetic and environmental factors, with age being the main risk factor. There is no cure, but there are many excellent symptomatic treatments.
- Deep brain stimulation has become a well-established symptomatic treatment for Parkinsons disease during the last 25 years.
- The therapy delivers electrical pulses to brain cells to decrease symptoms of Parkinsons disease, especially if symptoms cannot be adequately controlled with medication.
- The electrical signals delivered by DBS deactivate the target site within the brain without destroying any tissue, restoring the balance of electrical activity within brain, to offset the progressive loss of cells caused by Parkinsons.
Older surgical therapies such as pallidotomy and thalamotomy can ease symptoms but have not been proven to change the underlying course of disease.
The World Health Organization has estimated that the global elderly population will reach around 2 billion by 2050.
- Product
Dbs Device Management During A Crisis
Patients who utilize DBS therapy for management of neuropsychiatric disorders require ongoing surgical care and outpatient clinic visits for device management. The implantation of de novo DBS leads is considered an elective procedure and should not be scheduled while pandemic measures are in place.
The necessary maintenance includes routine IPG replacements , infection management, assessment of hardware-related complications, as well as outpatient stimulation adjustments . Limited device programming and management can be handled through telemedicine . The telemedicine visits and telephone consultations are also critical to promptly identify any potential surgical issues.
Surgical procedures can be classified into four categories according to the American College of Surgeons guidelines : elective , time-sensitive , urgent , and emergent . Outpatient clinic visits can be classified more simply as elective or urgent . We define an urgent clinic visit as one that would potentially prevent an emergency department visit, a hospitalization or significant disability. Pandemic measures may permit only emergent/urgent procedures and urgent outpatient visits. Depending on local regulations, virus spread, and available resources some elective and time-sensitive procedures may be liberalized based on need.
Also Check: Parkinson’s Disease And Weight Loss
Awake Vs Asleep Surgery
Standard DBS surgery is performed while you are awake and requires that you stop taking the medicines that control your Parkinson’s symptoms. During surgery, you are asked to perform tasks to help guide the electrode to the precise location in the brain.
Being awake during brain surgery, or being off medicine, is unsettling for some people. Asleep DBS is an alternative option at some centers.
Asleep DBS surgery is performed while you are unconscious and under anesthesia. Surgery takes place in an MRI or CT scanner to target and verify accurate placement of your DBS electrodes. Ask your surgeon if asleep DBS is an option for you.
| Must hold medications the morning of surgery | Don’t have to hold medications |
Placement Of The Neurostimulator
This procedure takes place under general anesthesia so that the person is asleep. The surgical team inserts the neurostimulator under the outer layers of skin, usually just under the collarbone, but sometimes in the chest or abdomen. The extension wire from the lead is attached to the neurostimulator.
Recommended Reading: Effect Of Exercise On Parkinson’s Disease
A General Rule Is That Dbs Will Likely Improve Parkinsons Symptoms That Respond To Medication
The Evaluation prior to DBS Surgery
A team of experts, including a movement disorder specialist and a neurosurgeon , conduct an extensive assessment when considering DBS for someone. The evaluation consists of medication and symptom review, examination both on and off Parkinsons drugs, brain imaging, and oftentimes also detailed memory/thinking testing . If DBS is offered, its important to discuss the expected benefits as each persons experience is unique. Its also critical to discuss the potential surgical risks, including bleeding, stroke and infection.
The DBS Procedure and Device Programming
In DBS surgery, thin wires called electrodes are placed into one or both sides of the brain in specific areas that control movement. Usually a person remains awake during surgery so that he or she can answer questions and perform certain tasks to make sure that the electrodes are positioned correctly. However, some medical centers now are using brain imaging to guide the electrodes to the right spot while a person is asleep. Each method has its pros and cons and may not be suitable for everyone or available everywhere.
Once the electrodes are situated, they are connected to a battery-operated device that is typically placed under the skin below the collarbone. This device, called a neurostimulator, delivers continuous electrical pulses through the electrodes to decrease Parkinsons symptoms.
How DBS Works
Research on DBS
What Happens After Surgery
After surgery, you may take your regular dose of Parkinson’s medication immediately. You are kept overnight for monitoring and observation. Most patients are discharged home the next day.
During the recovery time after implanting the electrodes, you may feel better than normal. Brain swelling around the electrode tip causes a lesion effect that lasts a couple days to weeks. This temporary effect is a good predictor of your outcome once the stimulator is implanted and programmed.
About a week later, you will return to the hospital for outpatient surgery to implant the stimulator in the chest/abdomen. This surgery is performed under general anesthesia and takes about an hour. Patients go home the same day.
Step 7: implant the stimulator You will be taken to the OR and put to sleep with general anesthesia. A portion of the scalp incision is reopened to access the leads. A small incision is made near the collarbone and the neurostimulator is implanted under the skin. The lead is attached to an extension wire that is passed under the skin of the scalp, down the neck, to the stimulator/battery in the chest or abdomen. The device will be visible as a small bulge under the skin, but it is usually not seen under clothes.
You should avoid arm movements over your shoulder and excessive stretching of your neck while the incisions heal. Pain at the incision sites can be managed with medication.
Read Also: Nursing Management Of Parkinson’s Disease
Is Your Patient A Candidate For Dbs Therapy
Consider deep brain stimulation when a patient has:
- Symptoms of levodopa-responsive Parkinson’s disease of at least 4 years’ duration that are not adequately controlled with medication.
- And motor complications of recent onset or motor complications of longer-standing duration.
The safety and effectiveness of this therapy has not been established for the following:
- Patients with neurological disease origins other than idiopathic Parkinsons disease
- Patients with a previous surgical ablation procedure
- Patients who are pregnant
- Patients under the age of 18 years
- Patients with dementia
- Patients with moderate to severe depression
How Is Deep Brain Stimulation Used To Treat Parkinsons Disease
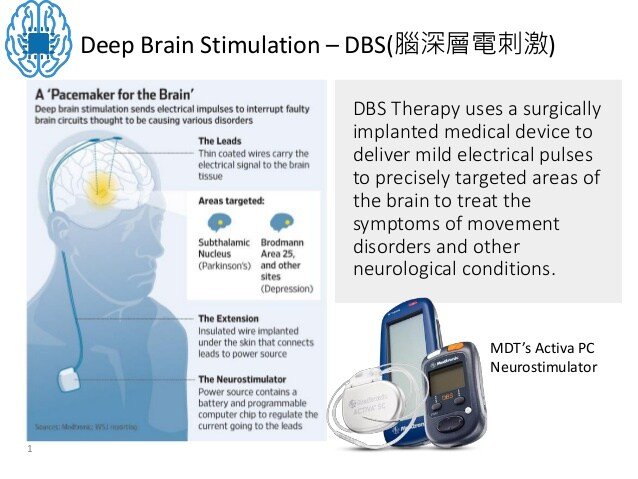
Deep brain stimulation delivers electrical impulses to a targeted area of the brain that is responsible for the movement symptoms caused by Parkinsons disease. The electrical impulses disrupt the abnormal activity that occurs in the brains circuitry, which is causing the symptoms.
There are three areas in the brain that can be targets for deep brain stimulation in patients with Parkinsons disease. They are the subthalamic nucleus, the globus pallidus internus, and the ventral intermediate nucleus of the thalamus. Each of these areas plays a role in the brains circuitry that is responsible for the control of movement.
The specific area in the brain to target in an individual with Parkinsons disease depends on symptoms that need to be treated. For example, deep brain stimulation of subthalamic nucleus is effective for all major movement symptoms of Parkinson’s disease, such as tremor, slowness of movement , stiffness , and problems with walking and balance. Deep brain stimulation of globus pallidus is another effective target for a wide range of Parkinson’s symptoms. The thalamic target is sometimes selected for patients with tremor symptoms. The recommended target for each patient is made collaboratively with the neurologist, neurosurgeon and other caregivers involved in the decision making process.
Read Also: Treating Depression In Parkinson’s Disease
Advances In Dbs Technology
The treatment can be used to tackle additional neurological problems and other disorders, Wodziak said, including epilepsy, seizures and dystonia, which is the sustained, involuntary contraction of muscles and can lead to painful cramping of the feet or hands, curling toes, or turning and twisting of the neck. A version of the same technology can even be used on the spinal cord. This year, Dr. Andre Machado of the Cleveland Clinic performed the first DBS surgery for stroke recovery using the Boston Scientific Vercise system. It is also considered for depression and weight loss.
Although the treatment has been around since the 90’s, there have been some incremental advances to the technology, including leads capable of focusing electricity to increasingly specific parts of the brain and smaller generators capable of connecting to devices using Bluetooth. Abbott’s DBS system was the first to be approved in the United States with a “directional lead,” which allows physicians to direct current more precisely than traditional DBS. It also allows for system control from an iPod Touch.
Less Medication More Relief

Medtronic DBS therapy may reduce the need for other Parkinsons medications1 and, consequently, medication-related side effects. DBS delivers therapy 24 hours a day and doesnt wear off while sleeping. Its already working when you wake up.
* Signal may not be present or measurable in all patients. Clinical benefits of brain sensing have not been established.
Read Also: Parkinson’s Support Group Connecticut
Risks And Side Effects Of Deep Brain Stimulation
Like any surgery, deep brain stimulation can have side effects, and it carries potential risks. Its also important to consider the complications and side effects of medications you take since their dosages can often be reduced following surgery.
While DBS may cause side effects, it may also reduce side effects from medications.
How Many Years Does The Battery Of Deep Brain Stimulation Last
The best DBS device would have a never-ending battery. But, in real-life the DBS battery does run out after some years.
Each of these devices has two varieties: Non-rechargeable & Rechargeable. The non-rechargeable batteries are cheaper. However, they last for a shorter period.
When the battery runs out, the wires inside the head do not need to be replaced. Only the battery below the chest skin is replaced.
So, the battery replacement surgery is much simpler and quicker than the original surgery.
The estimated average life of each of these batteries is noted below.
Also Check: Can Mold Cause Parkinson’s Disease
How Does It Work
A small device placed inside your chest sends electrical pulses to your brain. The pulses block nerve signals that cause Parkinson’s symptoms.
A DBS system has four parts:
- A thin wire, called a lead, that’s placed in the part of your brain causing symptoms
- A pulse generator, like a pacemaker, that sends tiny electrical signals to the lead
- A wire that connects the lead to the pulse generator
- A remote control to program the system — the only part outside your body
After the system is in place and turned on, a DBS expert will adjust it so you get the best relief for your symptoms.
You can also control the system yourself. You can turn it off and on, check the battery, and tweak the settings.
How Deep Brain Stimulation Works
Exactly how DBS works is not completely understood, but many experts believe it regulates abnormal electrical signaling patterns in the brain. To control normal movement and other functions, brain cells communicate with each other using electrical signals. In Parkinson’s disease, these signals become irregular and uncoordinated, which leads to motor symptoms. DBS may interrupt the irregular signaling patterns so cells can communicate more smoothly and symptoms lessen.
Recommended Reading: Non Shaking Parkinson’s Disease
What Happens Before Surgery
In the doctor’s office you will sign consent forms and complete paperwork to inform the surgeon about your medical history, including allergies, medicines, anesthesia reactions, and previous surgeries. Presurgical tests may need to be done several days before surgery. Consult your primary care physician about stopping certain medications and ensure you are cleared for surgery.You may also need clearance from your cardiologist if you have a history of heart conditions.
Stop taking all non-steroidal anti-inflammatory medicines and blood thinners 7 days before surgery. Stop using nicotine and drinking alcohol 1 week before and 2 weeks after surgery to avoid bleeding and healing problems.
You may be asked to wash your skin and hair with Hibiclens or Dial soap before surgery. It kills bacteria and reduces surgical site infections.
No food or drink, including your Parkinson’s medication, is permitted after midnight the night before surgery.
Try to get a good night’s sleep. The DBS surgery involves multiple steps and lasts most of the day, during which you may be awake and off medication.
Morning of surgery
Arrive at the hospital 2 hours before your scheduled surgery time to complete the necessary paperwork and pre-procedure work-ups. An anesthesiologist will talk with you and explain the effects of anesthesia and its risks.
What Are The Risks And Complications Of Deep Brain Stimulation
As with any surgical procedure, there are risks and complications. Complications of DBS fall into three categories: surgery complications, hardware complications, and stimulation-related complications.
- Surgical complications include brain hemorrhage, brain infection, wrong location of the DBS leads, and less than the best location of the leads.
- Hardware complications include movement of the leads, lead failure, failure of any part of the DBS system, pain over the pulse generator device, battery failure, infection around the device and the device breaking through the skin as the thickness of skin and fat layer change as one ages.
- Stimulation-related complications occur in all patients during the device programming stage. Common side effects are unintended movements , freezing , worsening of balance and gait, speech disturbance, involuntary muscle contractions, numbness and tingling , and double vision . These side effects are reversible when the device is adjusted.
Recommended Reading: Glutathione Injections For Parkinson’s