Risk Factors For Psychosis
Not everyone with Parkinsons will develop hallucinations or delusions, but there are several things can increase your risk:
- Dementia or impaired memory
- Depression: Individuals suffering from depression and PD are at a greater risk. In addition, severe depression alone can cause psychosis.
- Sleep disorders, such as vivid dreaming. Individuals commonly report vivid dreaming prior to the onset of psychosis. Other associated sleep disturbances include REM sleep disorder and general insomnia.
- Impaired vision
- Use of PD medications
How Is Parkinsons Disease Diagnosed
Diagnosing Parkinsons disease is sometimes difficult, since early symptoms can mimic other disorders and there are no specific blood or other laboratory tests to diagnose the disease. Imaging tests, such as CT or MRI scans, may be used to rule out other disorders that cause similar symptoms.
To diagnose Parkinsons disease, you will be asked about your medical history and family history of neurologic disorders as well as your current symptoms, medications and possible exposure to toxins. Your doctor will look for signs of tremor and muscle rigidity, watch you walk, check your posture and coordination and look for slowness of movement.
If you think you may have Parkinsons disease, you should probably see a neurologist, preferably a movement disorders-trained neurologist. The treatment decisions made early in the illness can affect the long-term success of the treatment.
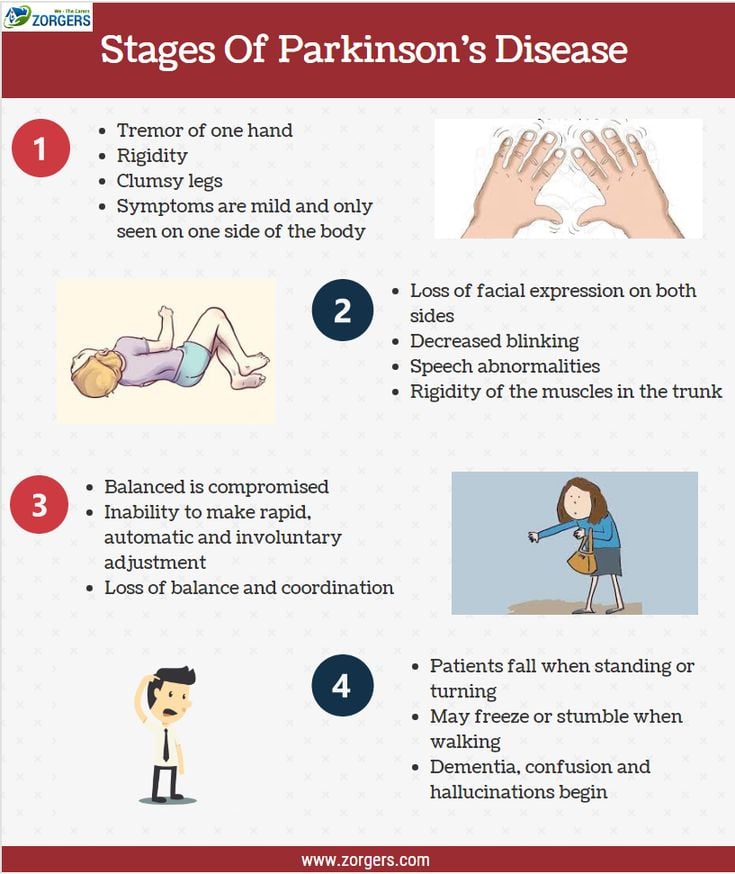
Stage Five Of Parkinsons Disease
Stage five is the most advanced and is characterized by an inability to rise from a chair or get out of bed without help, they may have a tendency to fall when standing or turning, and they may freeze or stumble when walking.
Around-the-clock assistance is required at this stage to reduce the risk of falling and help the patient with all daily activities. At stage five, the patient may also experience hallucinations or delusions.
While the symptoms worsen over time, it is worth noting that some patients with PD never reach stage five. Also, the length of time to progress through the different stages varies from individual to individual. Not all the symptoms may occur in one individual either. For example, one person may have a tremor but balance remains intact. In addition, there are treatments available that can help at every stage of the disease. However, the earlier the diagnosis, and the earlier the stage at which the disease is diagnosed, the more effective the treatment is at alleviating symptoms.
Also Check: Parkinson’s And Similar Diseases
Theory Of Pd Progression: Braaks Hypothesis
The current theory is that the earliest signs of Parkinson’s are found in the enteric nervous system, the medulla and the olfactory bulb, which controls sense of smell. Under this theory, Parkinson’s only progresses to the substantia nigra and cortex over time.
This theory is increasingly borne out by evidence that non-motor symptoms, such as a loss of sense of smell , sleep disorders and constipation may precede the motor features of the disease by several years. For this reason, researchers are increasingly focused on these non-motor symptoms to detect PD as early as possible and to look for ways to stop its progression.
Page reviewed by Dr. Ryan Barmore, Movement Disorders Fellow at the University of Florida, a Parkinsons Foundation Center of Excellence.
What Are The Important Points Regarding Duodopa At The End Of Life
Duodopa is a continuous infusion of dopaminergic medication administered as a gel into the gut, pumped via a percutaneously inserted gastrostomy tube . There is a requirement for care of the stoma and PEG tube together with functioning of the pump by the patient or carer.41 It reduces the time in motor off periods in advanced PD and quality of life.42 There is evidence of effective treatment up until death from within a case series.43
Read Also: Difference Between Parkinson’s And Dementia
What To Do With Deep Brain Stimulation At The End Of Life
Deep brain stimulation uses an Implantable Pulse Generator, usually placed in the infraclavicular area, connected to leads within the brain. There is a remote programmer, and also a charging unit in the case of a rechargeable device, which are given to the patient and their carer. It improves dyskinesias and also has a levodopa sparing effect.37
Deactivation of DBS may lead to increased symptom burden as mentioned in the section above and so awareness of features of PHS should be considered if there is failure at the end of life. Supportive treatment should be given if possible,38 and anticipation of symptoms of distress from rigidity and fever.
After death, deactivation of the device with the patients handheld programmer is required before removing the pulse generator and battery in the case of a cremation.
How Do I Know If I Have A Swallowing Problem
- I have recently lost weight without trying.
- I tend to avoid drinking liquids.
- I get the sensation of food being stuck in my throat.
- I tend to drool.
- I notice food collecting around my gum line.
- I tend to cough or choke before, during or after eating or drinking.
- I often have heartburn or a sore throat.
- I have trouble keeping food or liquid in my mouth.
*Please note that not all content is available in both languages. If you are interested in receiving Spanish communications, we recommend selecting both” to stay best informed on the Foundation’s work and the latest in PD news.
Recommended Reading: Drugs Contraindicated In Parkinson’s Disease
How To Manage Symptoms At The End Of Life
At the end of life, good practice is to plan for any potential symptoms that may arise. The most common symptoms anticipated are pain, dyspnoea, nausea and vomiting, agitation, anxiety, delirium and noisy respiratory secretions.18 For patients with PD particular considerations should be given to the more commonly used medicines, specifically anticholinergics and antidopaminergics. These are usually prescribed for treatment of respiratory secretions and nausea and vomiting. Alternatives are available for respiratory secretions, and include glycopyrronium, in preference to hyoscine hydrobromide. Although this is an anticholinergic, only a small proportion crosses the blood brain barrier.
For nausea and vomiting, ondansetron,19 cyclizine, domperidone have all been suggested in PD.20 However, ondansetron has been shown to be inferior to domperidone in the pre-treatment of apomorphine.21 Cyclizine has anticholinergic properties and may exacerbate confusion, especially when comorbid psychosis or cognitive impairment are present. Levomepromazine, although it has antidopaminergic effects, has been shown to be effective for nausea with rotigotine in a case report.22
Agitation, dyspnoea and pain can all be managed with the same anticipatory medications as recommended.20 Specifically relating to PD, several case reports have supported the intraoperative use of midazolam, during sedation, for tremor and dyskinesias,23,24 as well as for agitation at the end of life.20
Early Symptoms Of Parkinsons Disease
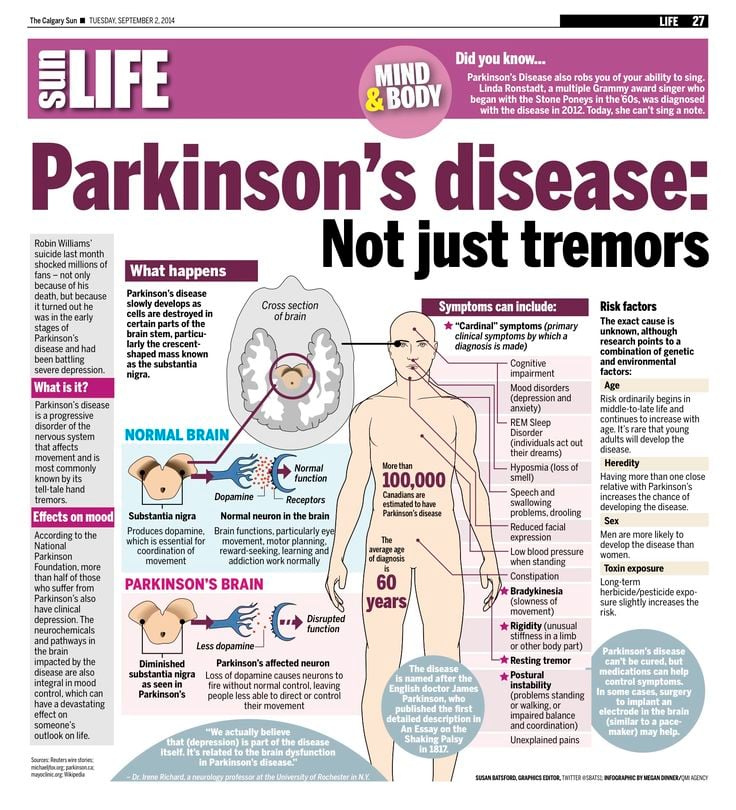
Parkinsons disease starts in the brain cells known as neurons. Neurons release a substance called dopamine and control the movements of the body. The symptoms of Parkinsons disease start when the neurons die and the level of dopamine in the brain decreases. Various studies suggest that by the time the symptoms appear the brain has lost around 60-80 percent of neurons. The early symptoms of Parkinsons disease are often given a miss as they are very mild. They usually start on one side of the body and are related to voluntary or involuntary motor functions.
Tremors: This is the most noticeable early symptom of Parkinsons disease. The patient experiences twitching, shaking of fingers, hand, or foot. These tremors occur while at rest but not when the individual is involved in a task. They may worsen as the patient is tired, excited or much stressed.
Stiffness: The patient may experience stiffness and slowing down of the movements. As the Parkinsons disease mostly affects the elderly or the people aged 60 and above, rigidity is absolutely normal development in many individuals. In the patients with Parkinsons disease, the stiffness does not go away as the patient begins the movement.
The patient experience shuffling gait and jerkier motions.
Posture: A leaning or a stooped posture is noticed in the Parkinsons disease patient. Impairment or lost reflexes makes it difficult to adjust or maintain the balance.
You May Like: Parkinson’s Vs Multiple Sclerosis
What Can Be Done
The first step is to get a referral to a speechlanguage pathologist . This professional will take a medical history and interview you about eating and swallowing. Next you will probably have a swallowing evaluation, using either a video x-ray or an endoscopic exam. During this procedure, you will swallow different consistencies of food and liquids, and the SLP can observe the entire swallowing process: from your first sip and bite, through the mouth, down the throat and esophagus, and into the stomach. This is the best way to find out the extent and cause of swallowing problems. Then the SLP can recommend treatment.
What Are The Symptoms Of Parkinson’s
The main motor symptoms of Parkinsons are:
- tremor
- slowness of movement
- problems with balance.
However, the condition doesnt only affect movement. People living with the condition can experience a range of non-motor symptoms that can often have a greater impact on their lives than movement difficulties.
Non-motor symptoms include:
- urinary urgency, frequency
- pain.
These non-motor symptoms are present at all stages of the condition but they can become more severe in the later stages of Parkinsons and have a major impact on quality of life.
Parkinsons gets worse over time and it can be difficult to predict how quickly the condition will progress. For most people, it can take years for the condition to progress to a point where it can cause major problems. For others, Parkinsons may progress more quickly.
Read Also: Balancing Exercises For Parkinson’s Patients
Palliative Care As An Option
If your loved one is not eligible for hospice, the good news is that they can still receive palliative care. This type of care focuses on alleviating symptoms, discomfort, and stress associated with any illness, including PD.
The main difference between palliative care and hospice is that palliative care can be given along with standard treatments, including therapies intended to prolong life.
Stage Four Of Parkinsons Disease
In stage four, PD has progressed to a severely disabling disease. Patients with stage four PD may be able to walk and stand unassisted, but they are noticeably incapacitated. Many use a walker to help them.
At this stage, the patient is unable to live an independent life and needs assistance with some activities of daily living. The necessity for help with daily living defines this stage. If the patient is still able to live alone, it is still defined as stage three.
Read Also: Parkinson’s And Violent Behavior
Understanding Parkinsons Care In The Later Stages: Part 3 Of 3
Parkinsons care moves to a whole new level as the disease progresses.
A Parkinsons disease diagnosis has an effect on family members along with the person experiencing this illness. Understanding what to expect as the disease progresses is paramount to being prepared for the changes to come and also to making life the best it can be each day.
Over the last couple of months, we have published blog posts about what to expect in the early and middle stages of Parkinsons disease. Information has included what family caregivers can do to best assist a family member with Parkinsons and how Anthem Home Care, a leader in professional home care in Taft, TX and surrounding areas, can help. In this closing segment in the series, we offer advice about Parkinsons care for someone in the late stages of this illness.
What To Expect In The Late Stages
The late stages of PD are medically classified as stage four and stage five by the Hoehn and Yahr scale:
- Stage Four of Parkinsons Disease In stage four, PD has progressed to a severely disabling disease. Patients with stage four PD may be able to walk and stand unassisted, but they are noticeably incapacitated. Many use a walker to help them. At this stage, the patient is unable to live an independent life and needs assistance with some activities of daily living. The necessity for help with daily living defines this stage. If the patient is still able to live alone, it is still defined as Stage Three.
- Stage Five of Parkinsons Disease Stage five is the most advanced and is characterized by an inability to arise from a chair or get out of bed without help. They may have a tendency to fall when standing or turning, and they may freeze or stumble when walking. Around-the-clock assistance is required at this stage to reduce the risk of falling and help the patient with all daily activities. At stage five, the patient may also experience hallucinations or delusions.1,2
Also Check: Is Cbd Good For Parkinson’s
Depression And Parkinsons Disease
Depression is common in people with Parkinsons disease, occurring in about 40% to 50% of patients. Depression can worsen when the disease becomes more advanced and treatment becomes less effective. Mental health counseling and treatment options are available to help people living with APD. Seek help if you or a loved one is experiencing depression with their Parkinsons.
What Is Advanced Parkinsons Disease
Advanced Parkinsons disease is a late stage of Parkinsons disease that is marked by limited mobility. Medications are used to control Parkinsons in early stages. When these medications lose their ability to work effectively and symptoms progress, physicians classify it as advanced Parkinsons disease.
APD usually occurs after 10 years of living with Parkinsons, but can occur much later. Patients in this stage may require a wheelchair or other assistive devices, and they have a higher risk of falling, dementia, and other cognitive problems.
This article will discuss the symptoms, treatment, and prognosis for advanced Parkinsons disease.
Also Check: Assisted Living For Parkinson’s Patients
Advanced Parkinsons Disease Symptoms
Parkinsons disease typically occurs in adults as they age and is characterized by tremors in the hands, arms, legs, and face, as well as slow movement, poor balance, and lack of coordination.
Parkinsons disease typically progresses in five stages. In the first three stages, symptoms are mild to moderate and less limiting to daily life. These include:
- Tremors or shaking
- Changes in posture, walking, and facial expression
- Difficulty walking, talking, eating, or dressing
- Falling
In the final two stages, when the disease has progressed to advanced Parkinsons, the symptoms become more severe and limiting. These include:
- Needing a walker or wheelchair to move
- Needing help with daily activities
- Having stiffness in the legs that makes it difficult to stand or walk
- Becoming bedridden
- Experiencing hallucinations and delusions
Stages Of Parkinsons Disease & Its Early And Late Symptoms
Parkinsons disease is a common neurodegenerative disease. It is characterized by progressive loss of muscle control, stiffness, slowness, and impaired balance. As the disease progresses the patient presents symptoms such as difficulty in walking, talking, and completing simple tasks.
The adult onset of Parkinsons disease is very common and it is mostly seen in the people aged 60 years or elder. Early onset i.e. age between 21-40 years or juvenile onset i.e. below 21 years of age can also occur. Before knowing the early and late symptoms of Parkinsons disease, it is necessary to look at the stages of this disease.
Read Also: Parkinson’s And Swollen Feet And Ankles
My Parkinson’s Story: Advanced Parkinsons
This 10-minute video alternates between an interview with a man and his wife and his palliative care team, including a doctor, nurse, clerg and social worker. The man and his wife shares his experience with late stage Parkinson’s. The palliative care team explains that their job is to support the best physical, emotional and spiritual wellbeing of the immediate family as well as help the family make end of life decisions.
What Are The Considerations For Pain Management In The Last Days Of Life In Pd

It is important to consider that pain can be a risk factor for, and associated with, many other symptoms which might be the presenting features in a patient with complex or advanced PD. These include a new or worsened confusion, hallucinations, agitation and symptoms of depression or apathy.
As well as being an underlying cause of another symptom, pain can also be the symptom of other features of PD, such as rigidity, dyskinesia, but also non-motor features, for example, depression and fatigue.
Identifying whether pain is at the root of the presenting complaint and what might be causing the pain is therefore the most important part of the initial history from the patient and the carer. Then using the clinical examination to confirm findings from the history and identify any features not already elicited such as abnormal posturing, or dystonia.
A recent review into the pathophysiology and treatment of pain in PD suggests simple analgesia with paracetamol and non-steroidal anti-inflammatory drugs but advises caution with opiate analgesia as constipation is a recognised problem in PD patients.25 The review mentions, however, the lack of evidence for many widely used analgesics specifically in PD.26
Don’t Miss: Nocturnal Leg Cramps Parkinson’s
Medications Used For Treating Psychosis
Antipsychotic agents are designed to balance abnormal chemical levels in the brain. Up until the 1990s, the use of antipsychotics in PD was controversial because the drugs used until that time work by reducing excess dopamine. This alleviated psychosis but caused dramatic worsening of PD motor symptoms.
Fortunately, medications that are better tolerated by people with PD are now available. Today, there are three antipsychotic medications considered relatively safe for people with PD: quetiapine , clozapine and the newest agent, pimavanserin . They cause limited worsening of PD while treating hallucinations and delusions.
Examples Of Delusions In Pd
- Jealousy
- Belief: Your partner is being unfaithful.
- Behavior: Paranoia, agitation, suspiciousness, aggression.
You May Like: What Is The Last Stage Of Parkinson Disease