How Can Mris Be Used To Detect Early Onset Parkinsons
MRIs use magnets to create detailed images of the inside of the body. Brain MRIs can help doctors spot tumors, brain bleeding, and other brain health conditions. Recently, medical researchers have discovered that MRIs can also spot small changes in the brain that can indicate Parkinsons disease.
A 2019 study on MRIs and Parkinsons found that people with Parkinsons often have visibly damaged brain neurons. The damage to neurons is present before any brain atrophy begins, and before symptoms are present.
Using this information, doctors can prescribe appropriate treatments, such as Deep Brain Stimulation therapy, that can slow down decline and improve the quality of life for people with Parkinsons.
Living With Parkinson Disease
These measures can help you live well with Parkinson disease:
- An exercise routine can help keep muscles flexible and mobile. Exercise also releases natural brain chemicals that can improve emotional well-being.
- High protein meals can benefit your brain chemistry
- Physical, occupational, and speech therapy can help your ability to care for yourself and communicate with others
- If you or your family has questions about Parkinson disease, want information about treatment, or need to find support, you can contact the American Parkinson Disease Association.
Complementary And Alternative Therapies
Some people with Parkinson’s disease find complementary therapies help them feel better. Many complementary treatments and therapies claim to ease the symptoms of Parkinson’s disease.
However, there’s no clinical evidence they’re effective in controlling the symptoms of Parkinson’s disease.
Most people think complementary treatments have no harmful effects. However, some can be harmful and they shouldn’t be used instead of the medicines prescribed by your doctor.
Some types of herbal remedies, such as St John’s wort, can interact unpredictably if taken with some types of medication used to treat Parkinson’s disease.
If you’re considering using an alternative treatment along with your prescribed medicines, check with your care team first.
Read Also: Exercises For People With Parkinson’s Disease
What Are The Five Stages Of Parkinsons Disease
Researchers may disagree on the number of stages of Parkinsons disease . However, they all agree the disease is a progressive disease with symptoms that usually occur in one stage may overlap or occur in another stage. The stage increase in number value for all stage naming systems reflect the increasing severity of the disease. The five stages used by the Parkinsons Foundation are:
- Stage 1: mild symptoms do not interfere with daily activities and occur on one side of the body.
- Stage 2: Symptoms worsen with walking problems and both sides of the body affected.
- Stage 3: Main symptoms worsen with loss of balance and slowness of movement.
- Stage 4: Severity of symptoms require help usually person cannot live alone.
- Stage 5:Caregiver needed for all activities patient may not be able to stand or walk and may be bedridden and may also experience hallucinations and delusions.
A neurologist who specializes in movement disorders will be able to make the most accurate diagnosis. An initial assessment is made based on medical history, a neurological exam, and the symptoms present. For the medical history, it is important to know whether other family members have Parkinsons disease, what types of medication have been or are being taken, and whether there was exposure to toxins or repeated head trauma previously. A neurological exam may include an evaluation of coordination, walking, and fine motor tasks involving the hands.
The diagnosis of Parkinsons disease is more likely if:
How Does Parkinsons Progress
Parkinsons is a chronic and slowly progressive disorder. This means that symptoms normally appear slowly and develop gradually over time. The stage at which symptoms appear, speed at which they progress and the severity of those symptoms will vary from person to person. The most important point is that Parkinsons affects everyone differently.
There are a wide range of symptoms, but it is highly unlikely that you will experience every possible symptom. Some of the early symptoms of Parkinsons include handwriting changes, reduced sense of smell, tiredness and constipation. As Parkinsons progresses symptoms will change over time, and new symptoms will emerge. It can take many years for symptoms to progress to a point where they cause problems.
Ultimately symptoms will begin to impact on your day-to-day life. Many symptoms are related to physical movement, so you may find that walking becomes difficult. You may also experience non-movement symptoms such as mood changes, disrupted sleep or difficulty communicating. As these symptoms worsen it may become difficult to manage all of your daily activities.
Currently, there is no known way to slow the progression of Parkinsons. However, medications and other treatments can help to effectively manage your symptoms. To ensure the effectiveness of medications, they will need to be reviewed regularly by your specialist or doctor.
Recommended Reading: Unified Parkinson’s Disease Rating Scale Updrs
The Last Year Of Life In Parkinsons Disease
The study also examined nearly 45,000 hospitalizations in people with terminal Parkinsons, meaning their end-of-life period.
Of those with terminal PD, the most common reasons for being in the hospital were:
- Lung disease that was not from an infection
Less common causes for hospitalization were problems related to the stomach or intestines, muscles, nervous system, or endocrine system .
It is not surprising that infection was the most common hospitalization before death, as people with Parkinsons are vulnerable to developing a number of infections as a result of their disease. For example, bladder dysfunction in Parkinsons increases a persons risk of developing urinary tract infections, which can become life-threatening if not detected and treated promptly.
In addition, research suggests that aspiration pneumonia is 3.8 times more common in people with Parkinsons as compared to the general population. It has also been consistently reported to be the main cause of death in people with Parkinsons.
Aspiration pneumonia results from underlying swallowing difficulties, which leads to stomach contents being inhaled into the lungs. Immobilization and rigidity, which can impair phlegm removal, also contribute to the development of pneumonia in people with Parkinsons.
Stooping Or Hunching Over
Stooping, leaning, or slouching when you stand and having difficulty standing up straight can be an early sign of Parkinsons disease.
Is it normal? Some things like pain from an injury or illness may cause you to have trouble standing straight. Certain bone conditions can also make you hunch over. If there is no clear reason for slouching or leaning, bring it to your doctors attention.
Also Check: How To Test For Parkinson’s Symptoms
How Do Symptoms Progress
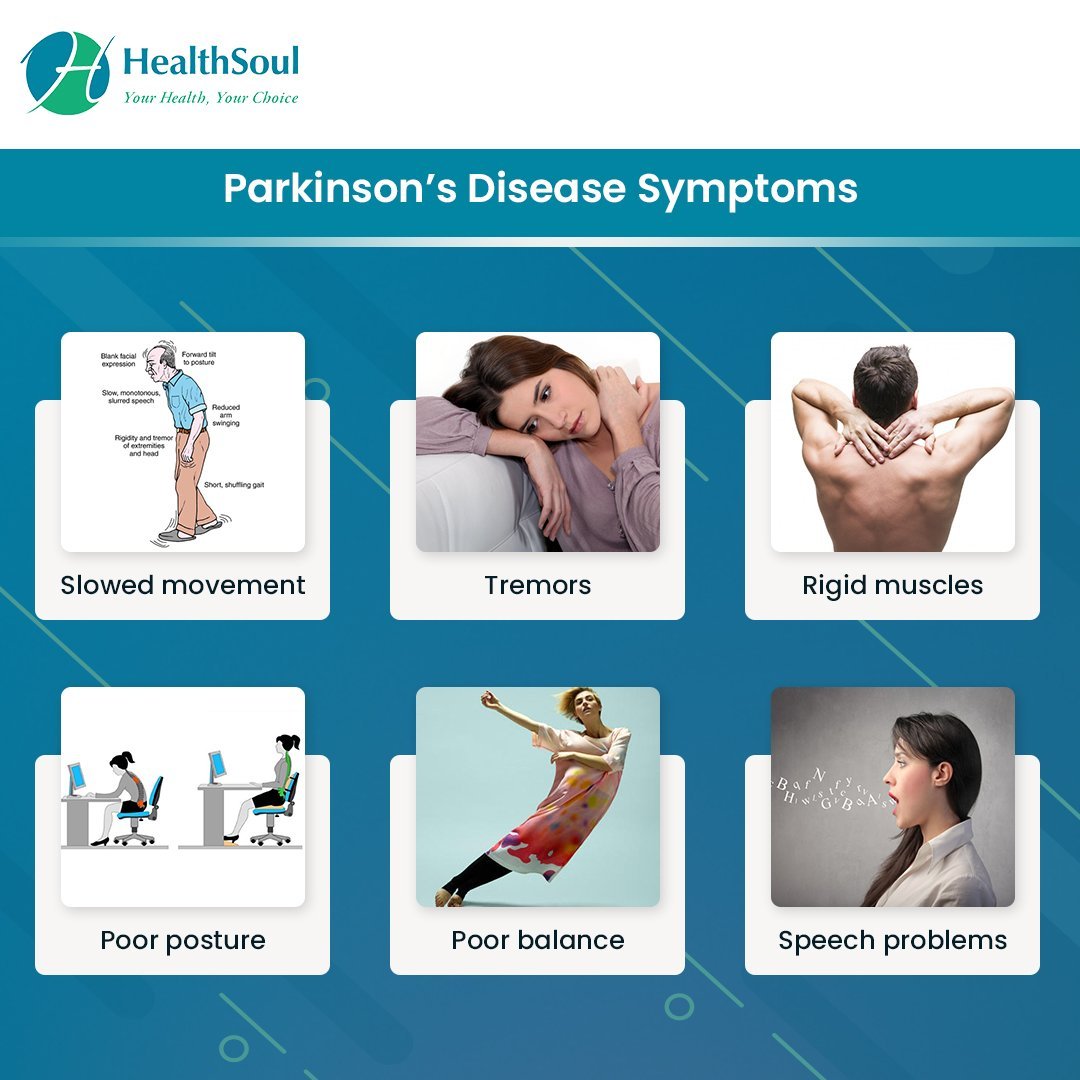
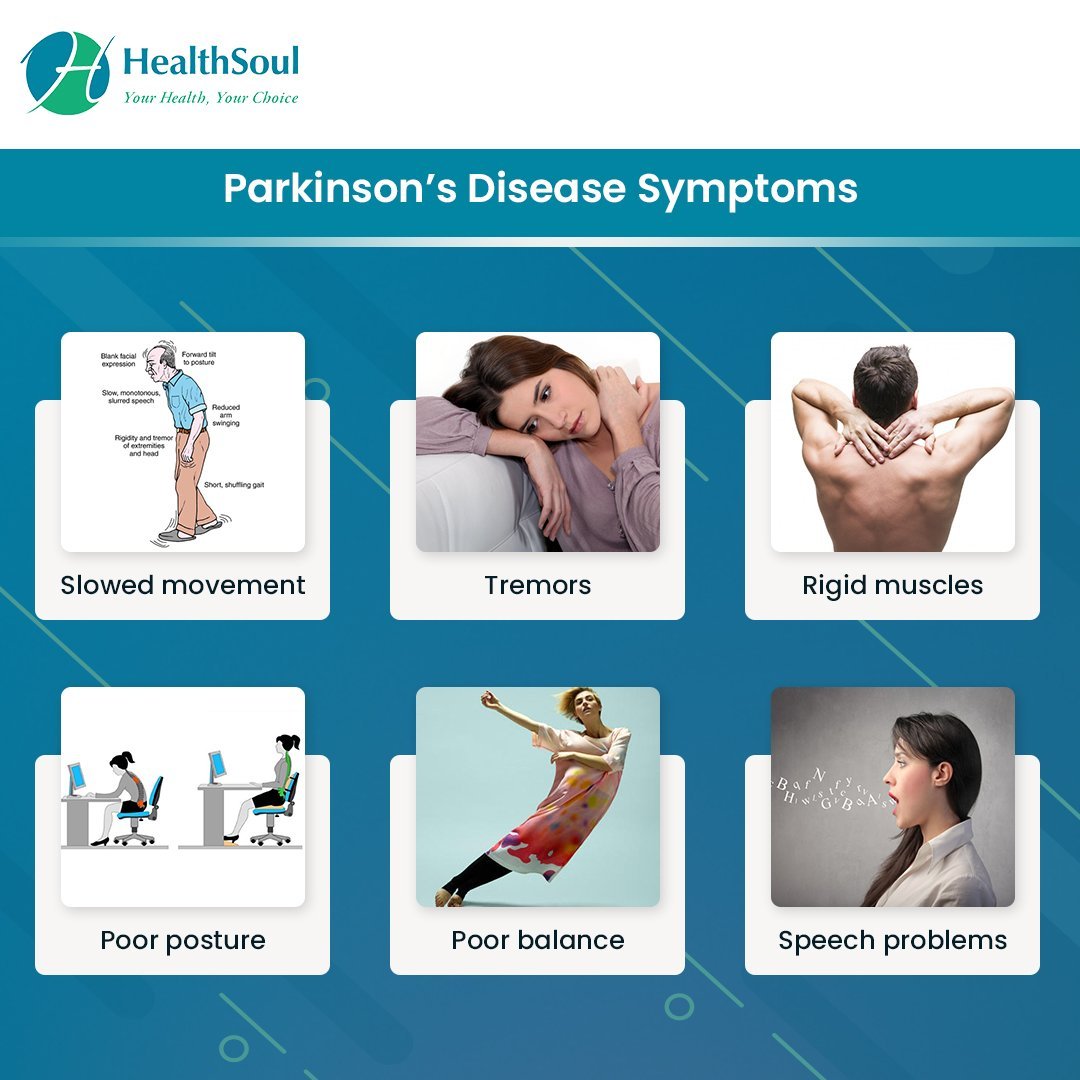
The most common symptoms of Parkinson’s are tremor, rigidity and slowness of movement.
Not everyone with Parkinson’s experiences the same combination of symptoms they vary from person to person.
Also, how Parkinson’s affects someone can change from day to day, and even from hour to hour. Symptoms that may be noticeable one day may not be a problem the next.
Many of the symptoms can be treated or managed with medication and therapies.
Many people with Parkinson’s lead active and fulfilling lives. An important part of coping with Parkinson’s is understanding how it affects you and how to work around it.
It may not always be easy to maintain a positive outlook, especially immediately after diagnosis. But we can give you help and support.
How Can I Tell If My Mci Is Progressing
For many people living with Parkinsons, cognitive changes will never progress beyond mild cognitive impairment. Others experience a slow, prolonged cognitive decline over time. Though less common, some people with Parkinsons experience a dramatic cognitive decline over a short period of time. Parkinsons experts still dont have foolproof methods to determine how severe a person with Parkinsons cognitive challenges may become, so its important to know what to look for in terms of possible progression and to speak up if you notice any changes in your thinking abilities and memory.
A decline in cognition can show up in various ways. For example, you may notice that you no longer feel comfortable driving, or you get lost traveling to spots in town that youve visited countless times. Your judgment may become increasingly impaired. You may struggle to complete routine tasks like counting out change at the store or making a pot of coffee, especially if the task involves multiple steps. You may have more difficulty speaking, understanding, following conversations, and expressing yourself. Your reading and writing abilities may worsen, and you may begin experiencing increased mood symptoms and less desire to engage in activities you once enjoyed.
Read Also: Nad And Parkinson’s Disease
Parkinsons Disease Symptoms Of Dementia
Up to one-third of people living with Parkinson’s disease experience dementia, according to the Parkinson’s Disease Foundation. Problems with dementia may include trouble with memory, attention span, and what is called executive function the process of making decisions, organizing, managing time, and setting priorities.
RELATED: 12 Famous People With Parkinson’s Disease
Mayo Clinic Q And A: Rate Of Progression Of Parkinsons Disease Hard To Predict
DEAR MAYO CLINIC: My father is 64 and was diagnosed with Parkinsons last year. So far his symptoms are very mild, but Im wondering what the typical progression of the disease is like. I have read that deep brain stimulation is sometimes recommended. When is this type of treatment usually considered? Is it safe?
ANSWER: The symptoms of Parkinsons disease, or PD, tend to begin very gradually and then become progressively more severe. The rate of progression is hard to predict and is different from one person to another. Treatment for PD includes a variety of options, such as exercise, medication and surgery. Deep brain stimulation is one surgical possibility for treating PD, but its usually only considered in advanced cases when other treatments dont effectively control symptoms.
Parkinsons disease is a syndrome which typically has no known cause. The diagnosis is based on symptoms. Neurologists who specialize in movement disorders typically have the most experience with PD diagnosis and treatment. There are many symptoms of parkinsonism. The most common include excessive slowness and lack of movement, as well as shaking or tremor.
As in your fathers situation, symptoms are often mild at the outset. How quickly they get worse varies substantially, perhaps because there may be multiple underlying causes of the disease. In most cases, symptoms change slowly, with substantive progression taking place over the space of many months or years.
Also Check: Sex And Parkinson’s Disease
Many Techniques Used Include:
- Shifting patients every two hours. Adjusting how patients are seated or supine helps prevent their weight from opening wounds on the skin.
- Toileting. Besides walking patients to the bathroom, caregivers help them undress and clean up afterwards.
- Changing diapers. If the patient is confined to bed, their diapers need to be checked and changed every two hours to prevent serious infections.
- Bathing and grooming. Patients who cant get in and out of the shower require sponge baths. Patients also need help trimming their nails, combing their hair, and brushing their teeth.
- Assistance with eating. Eating can be very challenging for patients. Caregivers may have to push patients to eat, offering small portions of whatever foods they can consume. Because of difficulties experienced when chewing and swallowing, soft foods may be all they can eat at this stage. Oatmeal, scrambled eggs, yogurt, applesauce, mashed potatoes, and smoothies are frequent choices solid food is cut up into bite-sized pieces to ensure patients can eat safely.
- Keeping patients hydrated. Patients need to drink 6-10 glasses of water a day to stay properly hydrated. Caregivers assist with the process, holding bottles, cups and straws as needed.
- Organizing medications. Patients are usually prescribed several medications to reduce shakes and control movement. Medications need to be carefully organized and all caregivers need to be briefed on their instructions.
Remission Of Cognitive Deficits In Parkinsons Disease: Recovery From A Nonamnestic Mild Cognitive Impairment Or Psychiatric Symptoms Remission
Jonas Jardim de PaulaAcademic Editor: Received
Abstract
Mild cognitive impairment is a clinical condition more frequent in patients with Parkinson’s disease than in general population. The nonamnestic presentations, usually characterized by executive dysfunction, are most prevalent. We present a case report of a Parkinsons disease patient diagnosed with nonamnestic mild cognitive impairment that showed complete remission of cognitive symptoms after one year. We discuss the possible causes for the remission, focusing on the treatment of medical conditions such as a major depressive episode and vitamin B12 deficiency, in addition to the change of pharmacological treatment. In a third assessment, cognitive performance remained normal. The case report highlights the importance of controlling clinical comorbidities on the assessment and followup of mild cognitive impairment, especially on Parkinsons disease.
1. Introduction
The concept of mild cognitive impairment in Parkinsons disease refers to a cognitive disorder where the subject shows an objective impairment in one or more cognitive domains and lack of or only mild functional impairment . Due to the absence of uniformity in diagnostic criteria, there is little agreement in the literature on what subtype of MCI is the most frequent in Parkinsons disease.
2. Case Description and Clinical Exam
3. Neuropsychological Assessment
3.1. Cognitive Status and Global Measures
3.2. Episodic Memory
3.3. Language
4. Discussion
Recommended Reading: Classic Signs Of Parkinson’s Disease
Theory Of Pd Progression: Braaks Hypothesis
Researchers believe a combination of genetic and environmental factors cause Parkinsons. In 2003, Heiko Braak, MD, hypothesized that an unknown pathogen in the gut could be the cause of PD.
This was followed by a more extensive hypothesis, stating that PD starts in two places: the neurons of the nasal cavity and the neurons in the gut. This is now known as Braaks hypothesis. In this theory, the pathogen enters the body via the nose and/or gets swallowed and reaches the gut. The pathogenic products thus come into contact with the olfactory and/or enteric neurons, triggering the aggregation of an abnormal protein called -Synuclein. The aggregated -Synuclein then spreads toward the central nervous system , and eventually arriving in and causing the degeneration of the dopaminergic neurons in the area of the brain called the substantia nigra.
This theory is supported by evidence that non-movement symptoms, such as a loss of sense of smell, sleep disorders and constipation, may appear several years ahead of movement symptoms. For this reason, researchers focus on these non-motor symptoms to detect PD as early as possible and to look for ways to stop its progression.
Page reviewed by Dr. Jun Yu, Movement Disorders Fellow at the University of Florida, a Parkinsons Foundation Center of Excellence.
What Are The Complications Of Parkinson Disease
Parkinson disease causes physical symptoms at first. Problems with cognitive function, including forgetfulness and trouble with concentration, may arise later. As the disease gets worse with time, many people develop dementia. This can cause profound memory loss and makes it hard to maintain relationships.
Parkinson disease dementia can cause problems with:
- Speaking and communicating with others
- Problem solving
- Paying attention
If you have Parkinson disease and dementia, in time, you likely won’t be able to live by yourself. Dementia affects your ability to care of yourself, even if you can still physically do daily tasks.
Experts don’t understand how or why dementia often occurs with Parkinson disease. Its clear, though, that dementia and problems with cognitive function are linked to changes in the brain that cause problems with movement. As with Parkinson disease, dementia occurs when nerve cells degenerate, leading to chemical changes in the brain. Parkinson disease dementia may be treated with medicines also used to treat Alzheimer’s disease, another type of dementia.
Recommended Reading: Did Katherine Hepburn Have Parkinson’s
Managing Symptoms In The End Stages Of Parkinsons
As Parkinsons worsens, it becomes increasingly challenging for families to provide care without professional assistance. Families may also consider residential care options to ensure that patients receive the kind of round-the-clock care they now require.
Due to the degenerative nature of the disease, patients in the end stage of Parkinsons are at severe risk of:
- Digestive problems
To avoid serious complications, patients require 24-hour assistance.
Can Parkinson’s Disease Be Cured
No, Parkinson’s disease is not curable. However, it is treatable, and many treatments are highly effective. It might also be possible to delay the progress and more severe symptoms of the disease.
A note from Cleveland Clinic
Parkinson’s disease is a very common condition, and it is more likely to happen to people as they get older. While Parkinson’s isn’t curable, there are many different ways to treat this condition. They include several different classes of medications, surgery to implant brain-stimulation devices and more. Thanks to advances in treatment and care, many can live for years or even decades with this condition and can adapt to or receive treatment for the effects and symptoms.
Recommended Reading: How To Check For Parkinson’s Disease
When Is It Time For Hospice Care
Even though the course of Parkinsons is predictable, the end stage of Parkinsons is not. Despite its severity, people dont pass on from Parkinsons rather, the disease leaves patients vulnerable to injury or infection which, in their weakened conditions, often proves to be fatal.
Consequently, knowing when to call hospice is not a simple matter of tracking symptoms. Physicians should always be consulted if patients are experiencing:
- Persistent pain
- Systolic blood pressure below 90
- Frequent falls or poor balance
- Recurrent infections
- Constant nausea
Once a doctor has given the patient a six-month prognosis, a hospice team can be called in. Patients can receive hospice wherever they call homeresidential care facilities, retirement communities or wherever theyve been residing.
Hospice serves both patients and families alike. It also gives patients a chance to spend their final weeks or months free from pain, while lifting a huge burden from families.
Hospice teams provide comfort care to patients. Comfort care provides relief from pain, nausea, and shortness of breath. Working closely with the patients doctor, the hospice team creates a personal care plan to manage symptoms. Nurses check in regularly to adjust pain medication. Home Health aides tend to the patients hygiene. Case managers secure high-grade equipment, such as hospital beds or oxygen machines.