First Direct Evidence That Abnormal Protein In Parkinsons Disease Triggers Immune Response
New York, NY Researchers have found the first direct evidence that autoimmunityin which the immune system attacks the bodys own tissuesplays a role in Parkinsons disease, the neurodegenerative movement disorder. The findings raise the possibility that the death of neurons in Parkinsons could be prevented by therapies that dampen the immune response.
The study, led by scientists at Columbia University Irving Medical Center and the La Jolla Institute for Allergy and Immunology, was published today in Nature.
The idea that a malfunctioning immune system contributes to Parkinsons dates back almost 100 years, said study co-leader David Sulzer, PhD, professor of neurobiology . But until now, no one has been able to connect the dots. Our findings show that two fragments of alpha-synuclein, a protein that accumulates in the brain cells of people with Parkinsons, can activate the T cells involved in autoimmune attacks.
It remains to be seen whether the immune response to alpha-synuclein is an initial cause of Parkinsons or if it contributes to neuronal death and worsening symptoms after the onset of the disease, said study co-leader Alessandro Sette, Dr. Biol. Sci., professor in the Center for Infectious Disease at La Jolla Institute for Allergy and Immunology in La Jolla, Calif. These findings, however, could provide a much-needed diagnostic test for Parkinsons disease and could help us to identify individuals at risk or in the early stages of the disease.
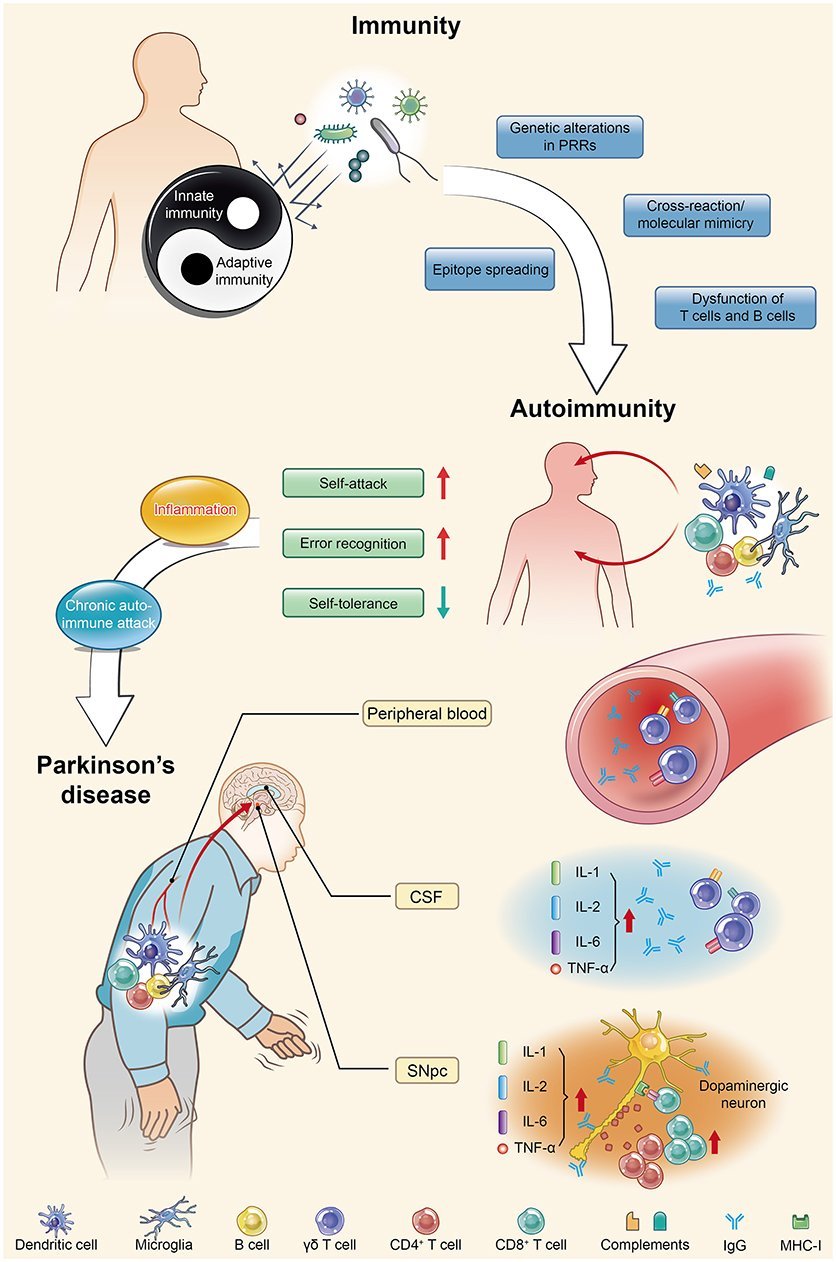
Pathogenic Protein Function In Autoimmunity
As discussed above, molecular mimicry and cross immunoreactions are two of the primary mechanisms through which autoimmunity is triggered. Molecular mimicry between herpes simplex virus 1 and human -syn was detected in PD patients in 2016. HSV1 infection could enhance the development of autoimmunity because autoreactive antibodies induced by HSV1 have the same response to the human -syn homologous peptide bound to the membrane of DNs and lead to DN destruction . These results also support the assumption that -syn participates in autoimmunity involved in the pathological progression of PD.
Parkinsons An Autoimmune Disease
Discovering the cause or etiology of diseases such as Parkinsons is essential to finding a treatment to prevent it. There are more and more advances in this field. And one of the latest ones is that Parkinsons could be an autoimmune disease.
Índice
Recommended Reading: Pharmacological Treatment Of Parkinson’s Disease
Potential New Treatment Strategies For Parkinson’s
This new finding provides additional knowledge and understanding of the disease processes that are present in PD and opens the door for using immunotherapies, drugs that suppress the abnormal immune response seen in autoimmune disorders. Additional research is needed to understand the molecular steps that occur in PD and the immune response, but researchers are hopeful that an immunotherapy strategy could help to prevent or lessen worsening symptoms in people with PD.1,2
Talk With Others Who Understand
MyParkinsonsTeam is the social network for people with Parkinsons disease and their loved ones. On MyParkinsonsTeam, more than 88,000 members come together to ask questions, give advice, and share their stories with others who understand life with Parkinsons disease.
Do you still have questions about what causes Parkinsons? Share your experience in the comments below, or start a conversation by posting on your Activities page.
Also Check: Does Parkinson’s Affect Your Speech
Understand Your Health With Nutrisense
Parkinsonâs disease is a serious neurological disorder that can cause many health complications and affect your quality of life. It’s important to monitor yourself for potential signs of its onset if you have a family history of the condition to best treat the disease.
NutriSense allows you to work with credentialed dietitians and nutritionists who can guide you and provide valuable information about maintaining a healthy lifestyle.
As a member of the NutriSense CGM program, youâll be able to monitor your bodyâs response to food and access your bodyâs data and response to food and other factors in real-time with the help of CGM devices that can track your glucose levels.
Take control of your health and learn how monitoring your glucose and overall nutrition can help you prevent disease and feel better with NutriSense.
The Connection Between Blood Sugar Levels And Parkinsons Disease
High blood sugar levels can lead to type 2 diabetes, a chronic illness in which the body becomes resistant to insulin. Insulin is a vital hormone responsible for transporting glucose from the blood to the cells to provide energy to the body. If the body becomes resistant to insulin, glucose stays in the blood for a longer time, causing many health complications.
Parkinsonâs disease and type 2 diabetes have been found to share many common pathophysiological mechanisms.
New research suggests a possible link between nerve cell degeneration, which can lead to diabetes, and Parkinsonâs disease. Insulin resistance is present in both individuals with diabetes and those with Parkinsonâs, so improving our blood glucose levels by reducing the glucose intake may help reduce the risks of both diseases.
Read Also: Sindrome De Wolff Parkinson White
Other Causes Of Parkinsonism
Parkinsonism is the umbrella term used to describe the symptoms of tremors, muscle rigidity and slowness of movement.
Parkinsons disease is the most common type of parkinsonism, but there are also some rarer types where a specific cause can be identified.
These include parkinsonism caused by:
- medication where symptoms develop after taking certain medications, such as some types of antipsychotic medication, and usually improve once the medication is stopped
- other progressive brain conditions such as progressive supranuclear palsy, multiple systems atrophy and corticobasal degeneration
- cerebrovascular disease where a series of small strokes cause several parts of the brain to die
You can read more about parkinsonism on the Parkinsons UK website.
Page last reviewed: 30 April 2019 Next review due: 30 April 2022
Best Evidence Yet That Parkinsons Could Be Autoimmune Disease
Parkinsons begins with abnormal clumping of a protein called synuclein in the brain
R. Bick, B. Poindexter, UT Medical School/SPL
EVIDENCE that Parkinsons disease may be an autoimmune disorder could lead to new ways to treat the illness.
Parkinsons begins with abnormal clumping of a protein called synuclein in the brain. Neighbouring dopamine-producing neurons then die, causing tremors and difficulty moving.
The prevailing wisdom has been that these neurons die from a toxic reaction to synuclein deposits. However, Parkinsons has been linked to some gene variants that affect how the immune system works, leading to an alternative theory that synuclein causes Parkinsons by triggering the immune system to attack the brain.
An argument against this theory has been that brain cells are safe from immune system attack, because most neurons dont have antigens the markers immune cells use to recognise a target. But by studying postmortem brain tissue samples, David Sulzer at Columbia University and his team have discovered that dopamine-producing neurons do display antigens. The team has now conducted blood tests to reveal that people with Parkinsons show an immune response to these antigens, while people who dont have the condition do not .
This article appeared in print under the headline Parkinsons may be the result of immune attack
More on these topics:
Read Also: Dopamine Treatment Parkinson’s Disease
Thanks For Signing Up
We are proud to have you as a part of our community. To ensure you receive the latest Parkinsons news, research updates and more, please check your email for a message from us. If you do not see our email, it may be in your spam folder. Just mark as not spam and you should receive our emails as expected.
Parkinsons Disease And Autoimmunity
This autoimmune component of PD may only be one piece of a larger puzzle. It has long been suspected that immune alterations are an important part of the development of PD, says Maureen Leehey, MD, professor of neurobiology at the University of Colorado School of Medicine in Aurora, CO. She notes previous research that has linked ibuprofen use in mid-life with lower PD risk. And studies have shown that in the early stages, but not the late stages, there is activation of immune fighting cells in the brains of persons with PD, Dr. Leehey says. I think that immune alterations are an important part of the progression of central nervous system damage in PD.
This isnt the first research being done on Parkinsons and autoimmunity there have been multiple studies in this vein in recent years. In 2017, the same researchers from La Jolla and Columbia University identified a specific protein that drives the T cell response in early Parkinsons disease. Further work has suggested that Parkinsons could be triggered by bacterial infection.
Paredes explains that changes in the can cause chronic inflammation that might influence Parkinsons symptoms. An April 2020 study in Nature Genetics theorized that Parkinsons may start in the gut, due to evidence that neurons in the gut are directly associated with the onset of disease.
Read Also: What Causes Parkinson’s Tremors
Changes In T Cell Subpopulations And Cytokines
Consistent with the systemic view that PD involves multiple systems and tissues, several studies have shown general alterations in cytokines and immune cell populations.
Proinflammatory cytokines are elevated in the blood of PD patients, including increased levels of IL-2 6 8 , MCP-1 , MIP-1 , RANTES , TNF , and IFN . Increased levels of proinflammatory cytokines and chemokines are indicative of an immune system responding to tissue damage and/or foreign molecules. The levels of cytokines and chemokines correlate with the clinical stage of the disease, highlighting a role for peripheral inflammation in PD progression . Altered T cells populations can also contribute to the changes in circulating cytokines. Th1 and TH17+ CD4+ cells can contribute to the increased levels of IFN, TNF, and IL-17 .
Matching Cases With Controls
All PD patients were labeled with a matching type constructed from a combination of three study-related variables and eight technical variables. The three study-related variables were: birth year, sex, birth location. The remaining technical variables were not related to our research question but were used to ensure that the cohort used did not interfere nor bias the study results . In total there were 8404 unique matching types.
For each matching type, the following procedure was done:
-
1) PD case individuals of this type were extracted and ordered randomly, forming a pool of cases, named A. PD control individuals of this type were extracted and ordered randomly, forming a much larger pool of controls, named B.
-
2) To find matches for individuals in the pool A, a sub-pool b was formed by selecting individuals from pool B using the following procedure. For each individual in sub-pool b, their personal follow-up end date must supersede the date of PD diagnosis for each individual in pool A. Individual b1, who is the first person in sub-pool b, is assigned to the first person in pool A . Individual b1 is permanently eliminated from pools b and B.
-
3) The step 2) is repeated sequentially with all individuals in A.
-
4) The step 3) is repeated maximum 200 times, or until the pool B is depleted, or until none of the individuals in A is assigned a new match.
Dont Miss: Parkinsons Big Movement Exercises
You May Like: How To Help Someone With Parkinson’s Dementia
Why Parkinsons May Be Autoimmune
In 2017, a study conducted at Columbia University Medical Center reported the first evidence that PD may be partially an autoimmune disease. Read on to learn about the process by which the researchers think Parkinsons may develop.
Protein in the brain called alpha-synuclein misfolds, then starts to build up in structures called Lewy bodies in brain cells that make dopamine. This abnormal process is called aggregation. This aggregation of alpha-synuclein tricks the immune system, causing it to produce a T-cell response.
These T cells engage in an autoimmune attack against the alpha-synuclein in brain cells, specifically in parts of the brain like the substantia nigra. This autoimmune response can occur in the neurons of those with PD. It does not appear to happen inside the bodies and brains of healthy controls.
As people age, their bodies may struggle to break down and recycle protein like alpha-synuclein. This buildup may continue to trigger the autoimmune disorder in their brains, possibly playing a role in the progression of PD.
In 2020, another study at La Jolla Institute for Immunology examined blood samples from people with PD and those without the disease. They confirmed the same T-cell response to alpha-synuclein in people with PD especially during the early stages of this movement disorder.
Data From Animal Models Support A Role For T Cells In Disease Pathogenesis
Although animal models have limitations in recapitulating PD, they are useful tools for genetic manipulation and identifying features of disease pathology. A range of models for studying PD have been developed, employing toxins or genetic mutations that recapitulate certain aspects of the disease. Most of the models highlight a causative role for infiltrating T cells in propagating neurodegeneration.
Toxin Models of PD
Intracerebral injections of the toxin 6-hydroxy-dopamine into the midbrain of mice induces degeneration of dopamine and noradrenaline neurons , which are rendered vulnerable to the drug because they express the dopamine transporter, DAT, that accumulates the toxin. Once in the neuronal cytosol, 6-OHDA mediates oxidative stress-related cytotoxicity . The subsequent acute neurodegeneration is manifested in motor deficits in mice and, if injected unilaterally, in rotational motions. 6-OHDA treated mice show IgG leakage, indicative of a leaky BBB, as well as T and B cell infiltration around CNS blood vessels . Treg cells are significantly decreased in the periphery of 6-OHDA treated rats, which are reported to not show marked T cell infiltration into the midbrain .
Viral Overexpression of -Syn to Model PD
Recommended Reading: Restore Gold Parkinson’s Reviews
Autoimmunity As A Trigger Of Axonal Dying
The death of the brain cells that produce dopamine, the chemical messenger that signals other cells involved in motor control, triggers the symptoms of Parkinsons disease. But researchers still dont know exactly what causes those dopamine-producing cells to die.
At the University of Montreal, Professor Louis-Eric Trudeau, a neuroscientist, investigates the possibility that an autoimmune attack on those dopamine cells is the culprit.
Trudeau and his immunologist colleague, Michel Desjardins, are studying the role of the portion of cells called axon terminals. These terminalsthe root-like extremities of cellsrelease the chemical messengers that send communication signals. Trudeau believes the death of these terminals, before the death of the dopamine cells themselves, is where the trouble starts.
Using dopamine-producing brain cells from genetically modified mice, Trudeau and his team are exposing dopamine cells directly to immune cells. Then they closely study the axon terminals of those dopamine cells to see what happens in an immune attack.
This project is focused on trying to develop a better understanding of why the terminals are affected, Trudeau says. This is a relatively new field in Parkinsons disease looking at the possibility that this disease is at least in part an autoimmune disease, in some ways like Multiple Sclerosis .
The immune system can be relatively easily targeted for treatment, Trudeau says.
Search
Read Also: Rbd And Parkinsons Disease
Diet Guidelines For Parkinsons Disease
Eating a healthy and nutritious diet is one of the best habits you can introduce into your lifestyle to prevent disease. The Parkinsonâs Foundation recommends a balanced diet full of whole grains, fruits and vegetables, dairy, and protein-rich foods to stay on top of your health and get plenty of exercise. However, everyone is different, and itâs important to test your bodyâs unique response.
For individuals already diagnosed with Parkinsonâs, professionals recommend staying hydrated, limiting sugar and caffeine intake, and increasing fiber intake to aid digestion.
Some studies have also found evidence supporting the use of omega-3, probiotics, and vitamin B and vitamin D supplements to aid in managing this condition.
When considering supplementation, always talk with a credentialed health provider, however a good place to start is by boosting your vitamins and minerals through food. Try adding fatty fish to your diet to boost omega-3, eating yogurt or fermented foods for extra probiotics, and things like good quality animal proteins, leafy greens, and eggs for sources of vitamin B.
Recommended Reading: Nursing Homes For Parkinson’s Patients
Autoimmune Targeting Of Mitochondria As A New Biomarker For Parkinsons Disease
Study Rationale:Parkinsons disease is a complex, age-related disorder for which there are currently no biomarkers available to diagnose or predict the onset of disease. However, growing evidence suggests that brain inflammation and autoimmunity are associated with PD and could thus serve as clinically relevant biomarkers. We recently found that PINK1 and Parkin, proteins that are disabled in early-onset PD, actively repress the processes that lead to the targeting of cellular mitochondria by the immune system. When PINK1 and Parkin are absent, immune cells inappropriately recognize and destroy these vital cell structures damage that is associated with Parkinson’s disease.
Impact on Diagnosis/Treatment of Parkinsons Disease: The ability to monitor the engagement of mitochondria-specific autoimmune mechanisms will open new avenues for the treatment of PD, which had not previously been linked to autoimmunity. Furthermore, our results hold the promise to better categorize people with PD and identify those that will most likely benefit from treatments.
Next Steps for Development:We will recruit independent cohorts to validate the autoimmune signature we identify and to evaluate whether our results can be used as a biomarker to reliably identify individuals with Parkinson’s.
In Vitro Studies Of Ipsc
A recent in vitro study using induced-pluripotent stem cells -derived midbrain neurons and T cells from PD patients was the first to show that PD patient-derived T cells can kill dopamine neurons directly. Sommer et al. determined that PD patients contain significantly higher Th17 cells than healthy controls . The PD patient-derived Th17 cells exerted cytotoxic effects on neurons by releasing IL-17A, a cytokine detected by IL-17R expressed on neurons . The iPSC in vitro cultures lacked glia, which express MHC-II and can potentially interact with Th17 cells. In addition, T cells were activated non-specifically, and so the antigen specificity of Th17 cells remains unclear . While the study indicates that PD-derived T cells can directly kill dopaminergic neurons, the omission of professional antigen presenting cells, antigenicity, and neuronal specificity in the cultures in this initial study overlooks the role of multiple relevant in vivo factors important for disease progression. Moreover, the mode of action that garners specific vulnerability of dopaminergic neurons and avoids unaffected neurons was not resolved in this study. Nevertheless, the study indicates Th17 cells may participate in PD-related neuronal death.
Also Check: Prevalence Of Parkinson’s Disease