Memory Problems And Dementia
Research shows that hallucinations and delusions often happen when someone with Parkinsons also has problems with memory, thinking problems or dementia.
If you experience hallucinations at an early stage of Parkinsons, it could be a sign of another medical condition, such as dementia with Lewy bodies.
You May Like: Ultrasound Treatment For Parkinsons Disease
Next Step: Get A Health Screening
If you think you may have had your first hallucination, its important to talk to your health provider about whats going on. Especially if your hallucinations have come on quickly or are dramatically different, there may be something else going on, like a urinary tract infection, which is associated with cognitive changes in older patients, says Melita Petrossian, M.D., a neurologist at Providence Saint Johns Health Center in Santa Monica, CA. You may also be having vision issues, so that should also get checked, as well as your mental health.
Pathophysiology Of Pd Psychosis
The precise pathophysiology of visual hallucinations in PD remains unclear however, neuropathological and structural imaging studies have provided some insight regarding the type and distribution of pathologic change associated with these phenomena. Neuronal loss in multiple brain regions, with associated LBs containing alpha-synuclein, is the principle pathological finding in Parkinsons disease . However, characteristic Alzheimers disease pathology can be found in the brains of patients with PD and is associated with earlier onset of dementia . Cognitive impairment is a risk factor for visual hallucinations, and concomitant AD pathology has been linked with the phenomena .
Dopamine cell loss in the substantia nigra is a required feature for the pathological confirmation of PD, but this is not the earliest affected area . According to Braaks hypothesis, LBD pathology begins in the olfactory regions and lower brain stem , progresses to the midbrain substantia nigra , and then to the basal forebrain, hypothalamus, thalamus, and hippocampus before spreading to higher-order cortical association areas . The evolution of visual hallucinations in PD has been conceptualized to mirror this spreading pathology with minor experiences indicating brainstem pathology, formed visual hallucinations with insight indicating basal forebrain involvement, and multimodality hallucinations with associated loss of insight and delusions indicating widespread cortical LBD pathology .
Don’t Miss: What Is The Difference Between Parkinson’s And Alzheimer’s
Selfcare For The Person With Parkinsons
- Join a Parkinsons support group if you dont already belong to one. Talk about your experiences, ask for help if you need it and share whats worked and not worked for you.
- Offer to have coffee with someone you know has been newly diagnosed and offer them support and encouragement.
- Make time to exercise and get out in nature every day.
- Communicate frequently with your doctors and discuss the possibility of tweaking your medications if your symptoms become worse.
- Rest when you need it.
- Plan a day trip or a vacation and get away from your normal surroundings.
- Take control where you can and keep authoring your own story.
- Practice meditation or yoga or tai chi to relax and calm your mind.
- Start a new project that youre excited to work on every day.
- Communicate with your care partners and let them know how they can best help you.
Visual Integrity And Visual Perceptual Scores
Cataracts were reported by 20% of the recruited participants while 19% of the participants had cataracts removed . Other ophthalmological history reported include glaucoma by two participants , macular degeneration by one participant , and laser treatment .
Visual acuity and perceptual scores are summarized in Table 1. There was a pattern of overall decline in visual integrity within the PDD patients relative to the control group, characterized by a significant reduction in LOGMAR measurements of visual acuity. As expected, PDD-CVH patients showed a characteristic significant increase in the number of false perceptions reported during the pareidolia task compared to PDD-NCVH patients. Interocular latency differences were significantly higher in PDD-CVH compared to the PDD-NCVH group.
Also Check: How Long Does It Take To Diagnose Parkinsons
Also Check: Strength Training Exercises For Parkinson’s
Do Hallucinations Go Away
Some visual hallucinations are so mild they might not even register on a conscious level, Dr. Ramdhani says. For instance, you may see a shadow thats not there, or glimpse something in your peripheral vision that clears when you turn your head. For some people, those may go away on their own, especially with a change in medication. In more advanced stages, though, these hallucinations may occur along with delusions, which means a false belieflike thinking your spouse isnt your real partner. Dr. Ramdhani says this can happen due to cognitive impairment, such as dementia.
Hallucinations And Delusions In Parkinson’s Disease
It might be surprising to learn that 20 to 30 percent of people with Parkinsons disease will experience visual hallucinations. While typically not a symptom of PD itself, they can develop as a result to a change in PD medication or as a symptom of an unrelated infection or illness. It is important to know the signs of hallucinations and how to manage them.
Hallucinations and other more severe perceptual changes can be distressing to family often more so than to the person experiencing them. For the well-being of people with PD and caregivers, it is important to identify hallucinations as early as possible and take steps to reduce them.
The following article is based on the latest research and a Parkinsons Foundation Expert Briefings about hallucinations and delusions in Parkinsons hosted by Christopher G. Goetz, MD, Professor of Neurological Sciences, Professor of Pharmacology at Rush University Medical Center, a Parkinsons Foundation Center of Excellence.
Don’t Miss: Diseases Similar To Parkinson’s
Inborn Errors Of Metabolism
A handful of inborn errors of metabolism may cause visual hallucinations. While these are quite rare, they are nonetheless important to consider because patients with inborn errors of metabolism may present with hallucinations at a time when their disease is treatable and when serious neurologic damage has not yet occurred. Specific inborn errors of metabolism that may present with visual hallucinations include homocysteine remethylation defects, urea cycle defects, GM2 gangliosidosis, Neimann-Pick disease type C, and -mannosidosis.
Whats The Treatment For Parkinsons Disease Psychosis
The single most important thing to do when it comes to Parkinsons disease psychosis is to tell your care providers and partners the minute you notice changes in your vision, hearing, thinking and behavior. The earlier they know whats going on, the sooner they can begin interventions to help you feel better.
Once you bring your concerns up to your doctor, they will typically do a clinical evaluation, review your medications and dosage, assess your lifestyle and determine the severity of your symptoms. Depending upon what they find, they may refer you to counseling or therapy, adjust your medication, change your medication, eliminate medication or do all of the above. If none of those strategies work, they may try antipsychotic drug therapy to see if they can adjust chemical levels in the brain. This can bring with it an entirely different set of problems so its important to be invested every step along the way and be sure youre well-informed before you move in that direction.
Dont Miss: Judy Woodruff Parkinsons
Don’t Miss: Atrial Fibrillation And Parkinson’s
The Bottom Line On Pd Psychosis
While it can be tricky to balance treating your motor symptoms of Parkinsons disease with treating symptoms like psychosis, working closely with your health care team can help you find the right combination of medications and lifestyle management skills for you. And remember: As with many aspects of this disease, early intervention is best. Psychosis in Parkinsons disease is something that, as providers and family members, important to screen for early on so we can monitor it, says Dr. Pan.
-
Parkinsons Information: National Institute of Health. Parkinsons Disease.
-
Psychosis in Parkinsons Information: The Michael J. Fox Foundation for Parkinsons Research. Ask the MD: Parkinsons Disease Psychosis.
-
Hallucinations and Delusions in Parkinsons: Parkinsons Foundation. Hallucinations/Delusions.
-
2017 Psychosis in Parkinsons Study:Parkinsons Disease. Management of Psychosis in Parkinsons Disease: Emphasizing Clinical Subtypes and Pathophysiological Mechanisms of the Condition.
You May Like: Early Parkinsons Symptoms In Young Adults
Other Types Of Hallucinations
In addition to persistent or repeated visual hallucinations, a Parkinsons Disease patient might also see a fleeting image out of the corner of their eyes, like a cat or a shadow passing by, but when they turn to look, there isnt anything there. Sometimes they see slight flashes of light, which are very much like reflections off their eyeglasses. A presence hallucination, is another type of experience which is not really a hallucination. With a presence hallucination, patients have a strong feeling of another person, or an animal, being behind them or to the side, but when they turn around, there isnt anything there. This is a strong feeling something most people have experienced on occasion but in this case, its experienced more frequently and more strongly.
Also Check: Parkinson Like Symptoms From Medications
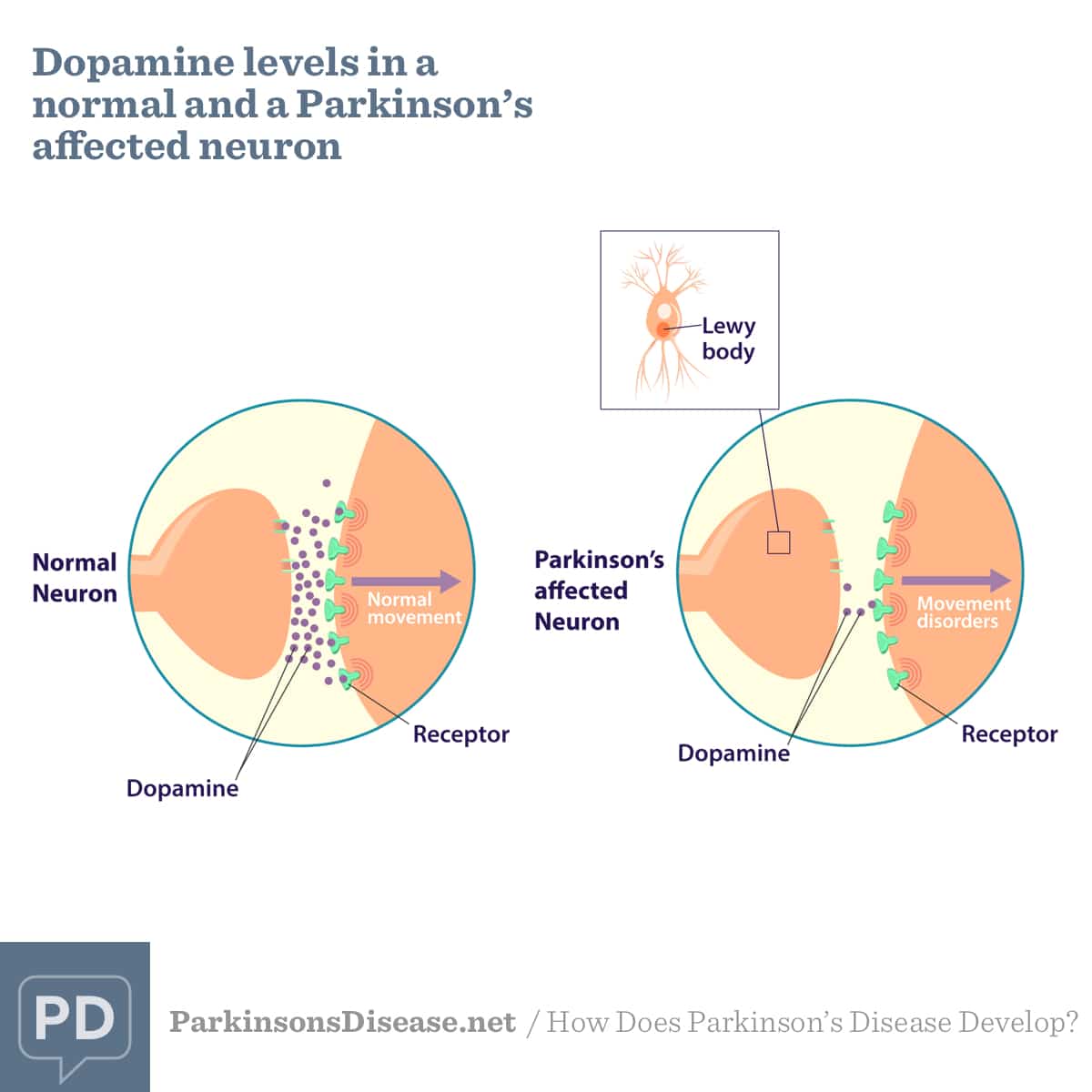
What Causes Parkinsons Disease Psychosis
Parkinsons is a brain disorder associated with a loss of dopamine-producing nerve cells deep inside the brain. Dopamine is a neurotransmitter that helps regulate the bodys movement, and it also allows us to think clearly and regulate our emotions. When you try to replace the dopamine thats been lost in a person with Parkinsons, it can cause the system to get out of whack which can impact thinking, how visual things are processed and more. Parkinsons disease psychosis is therefore typically a side effect of the disease itself or the medications used to manage it.
As a result, its an ongoing balancing act for Parkinsons doctors to prescribe enough dopamine to control a person with Parkinsons motor symptoms, but not so much that the person experiences hallucinations and/or delusions.
Can Hallucinations Be Treated
The treatment for hallucinations consists primarily of removing any existing medical cause, especially reducing or stopping any triggering pharmacological cause for example by reducing a dose or discontinuing treatment with a certain drug. If the increase in motor symptoms then becomes troublesome, a return to the earlier anti-Parkinsons drug may be considered, but with the addition of an atypical neuroleptic drug.
Most neuroleptics can worsen Parkinsons and are forbidden when treating people with the condition. Medications for dementia can also reduce the incidence of illusions and hallucinations when there is underlying cognitive impairment. Parkinsons treatments are developing fast and it is likely that we will see even more effective ways of avoiding and treating hallucinations in the coming years.
The most important thing is to report hallucinations to your doctor or nurse, and to discuss if they should be treated in some way.
Read Also: Microbiome Diet For Parkinson’s Disease
Visual Hallucinations According To The Duration Of Parkinson’s Disease
The prevalence of hallucinations of all types and of visual hallucinations in the 3 months preceding inclusion in the study increased with the duration of Parkinson’s disease . We compared the characteristics of the patients with and without hallucinations among those with a short history of Parkinson’s disease and those with a long history . The results are shown in Table 7. Visual hallucinations had been present for a mean of 0.8 years in the patients with short-duration Parkinson’s disease and for 2.4 years in the patients with long-duration Parkinson’s disease . However, eight patients with long-duration Parkinson’s disease and one patient with short-duration Parkinson’s disease could not remember the year of onset of visual hallucinations. In both groups, patients with formed visual hallucinations were older and were more likely to be demented, according to DSM criteria, than non-hallucinators. The MMP score was lower in patients with visual hallucinations, although the difference reached significance only in patients with long-duration Parkinson’s disease. Patients with visual hallucinations had a more severely affected motor state than non-hallucinators in the long-duration group only.
Visual Hallucinations In Parkinsons Disease: Towards Better Understanding And Treatments
Parkinsons disease is a common neurodegenerative disease, affecting more than 2% of people over 75, with estimated 7 to 10 million affected people worldwide. Although traditionally Parkinsons disease is thought of as a disorder of movement, with tremor and slowing of movement being the cardinal features, it can cause a wide range of other non-motor symptoms and frequently leads to dementia. These non-motor symptoms, are common, can occur even before motor symptoms become evident and are often the most troubling for patients.
Visual hallucinations, the sensation of seeing objects that are not really there, are a common non-motor symptoms in PD, affecting up to 70% of individuals over the course of the disease. As well as causing distress, visual hallucinations have a significant impact on the quality of life of patients and their families: hallucinations often herald the cognitive decline and are a strong predictor for nursing home placement.
The wide variety of visual hallucinations
The experience of visual hallucinations vary from person to person and can change across the course of the disease. Commonly, people with Parkinsons disease experience one or more of the following hallucinations:
Visual hallucinations are challenging to treat
A better understanding of hallucinations is needed
You May Like: What Is The Most Effective Treatment For Parkinson’s
What Is Parkinsons Disease Psychosis
Parkinsons disease psychosis is a non-motor symptom of Parkinsons disease that causes patients to experience hallucinations and/or delusions.More than half of all patients with Parkinsons disease eventually develop symptoms over the course of their disease.1
Diagnosing and treating this condition can be complex. The condition relates to both neurology and psychiatry . For this reason, Parkinsons disease psychosis is considered a neuropsychiatric condition, since it deals with mental health symptoms caused by a disease of the nervous system .
Introducing an easier way to track your symptoms and manage your care.
Dont want to download the app? Use the non-mobile version here.
Visual Hallucinations: Differential Diagnosis And Treatment
Have you ever encountered a patient who reported isolated visual hallucinations but did not have any other symptoms of delirium or psychosis? Have you wondered which medical and neurologic illnesses may present with visual hallucinations? Have you deliberated about how best to work up and treat patients with visual hallucinations?
If you have, then the following questions and answers should serve to frame the differential diagnosis of visual hallucinations and to explore the available options for diagnostic testing and treatment.
Don’t Miss: How To Manage Parkinson’s
Treatment Of Parkinsons Disease Psychosis
Andrew Schleisman, PharmD Candidate 2017
Mikayla Spangler, PharmD, BCPSAssociate Professor of Pharmacy Practice
Emily Knezevich, PharmD, BCPS, CDEAssociate Professor of Pharmacy PracticeCreighton University School of Pharmacy and Health ProfessionsOmaha, Nebraska
US Pharm. 2016 41:HS20-HS26.
ABSTRACT: Delusions and hallucinations in patients with Parkinsons disease, a condition known as Parkinsons disease psychosis , have historically been treated with clozapine and quetiapine because of their relatively low likelihood of worsening motor symptoms. Although clozapine is considered the drug of choice, it is underused in this population because of the need for frequent monitoring. Quetiapine, on the other hand, is generally first-line treatment despite its questionable efficacy. Consequently, in 2006, the American Academy of Neurology identified a need for the development of a novel antipsychotic with evidence of both safety and efficacy in patients with PDP. Pimavanserin, which has shown promise in clinical trials, recently became the first agent to receive FDA approval for the treatment of PDP.
Medications Used For Treating Psychosis
Antipsychotic agents are designed to balance abnormal chemical levels in the brain. Up until the 1990s, the use of antipsychotics in PD was controversial because the drugs used until that time work by reducing excess dopamine. This alleviated psychosis but caused dramatic worsening of PD motor symptoms.Fortunately, medications that are better tolerated by people with PD are now available. Today, there are three antipsychotic medications considered relatively safe for people with PD. They cause limited worsening of PD while treating hallucinations and delusions.
Also Check: Michael J Fox Parkinson’s Research
Treatment Options For Pd Psychosis
Treating psychosis is truly a challenge. Unfortunately, only 10 to 20 percent of people with PD psychosis actually inform their doctor of their symptoms. Dr. Dewey speculates that stigma and fear of embarrassment prevent many patients from seeking help.
When new symptoms of any kind arise, it is crucial to make a doctors appointment to discuss the issue. A physician will first try to determine whether there is an underlying illness that could be causing psychotic behaviors. Treating the underlying cause is one of the simplest ways of minimizing these episodes.
When there is no other identifiable source, doctors often turn their attention to the medications that the patient is taking. Gradually decreasing the dosage of dopamine-enhancing medication may reduce psychotic symptoms, but the obvious trade-off is that the persons motor function is likely to deteriorate more rapidly. Balancing risks and benefits is a delicate and complicated process that often involves a three-step approach, including assessment and planning, adjusting or reducing any medications, and initiating antipsychotic therapy.
Medical research produces discoveries continually, so keeping an ongoing dialogue open with your loved ones doctor should be a priority. Finding the best balance of treatment is crucial for optimum care and quality of life.
Comparison Of Hallucinators And Non
The patients with isolated minor hallucinations were compared with the patients with no hallucinations . The only significant difference was a higher CES-D score in the group with minor hallucinations . When the presence of depression was determined using the cut-off values of the CES-D, depression was more frequent in the patients with minor hallucinations than in the patients without any hallucinations , but this difference did not reach significance.
The patients with formed visual hallucinations are compared with the non-hallucinators in Table 5. Patients with visual hallucinations differed in a number of respects: they were older, had a longer duration of disease, had a more severe motor state, had more depressive symptoms, and were more likely to have cognitive impairment, day-time somnolence and a history of ocular pathology. They were less likely to receive anticholinergics or selegiline and received a higher daily dose of levodopa, but the levodopa-equivalent dose did not differ significantly between the two groups. Visual hallucinations were recorded in 70% of the patients with dementia versus 10% of non-demented patients , and in 55% of the patients with severe cognitive disorders versus 8% of the patients with absent or moderate cognitive impairment .
The patients with hallucinations of any type were compared with the patients with no hallucinations. The results were identical to those of the preceding analysis, except for the degrees of significance .
Read Also: How Long Does Parkinson’s Disease Take To Progress