Breathing & Respiratory Difficulties
Some people with Parkinsons disease may experience shortness of breath. There is no clear cause underlying respiratory dysfunction in PD, its frequency or the effect that medications have on respiration. Several reasons for shortness of breath in PD include:
- Wearing off is a common experience among people with PD who have been taking levodopa for several years. These occur when the medication benefit wears off and PD symptoms return before the next dose.
- Respiratory dyskinesia refers to an occurrence of irregular and rapid breathing when levodopa medications reach their peak effect. These may accompanied by involuntary body movements, typically experienced as dyskinesia.
- Anxiety is a common symptom of PD that may also exacerbate shortness of breath, whether by itself or as a consequence of wearing off of the medication.
- Aspirationpneumonia is a pneumonia that develops after food or liquid goes down the wrong pipe. Advanced PD can increase the risk of swallowing difficulties, choking and aspiration pneumonia.
- Non-PD health issues include conditions such as asthma, allergies, lung disease, heart disease and other conditions that may cause shortness of breath.
Relaxation With Guided Imagery
During guided imagery, a person is given ideas and images to mentally focus on while they are relaxing and breathing deeply.5
One study evaluated the benefit of relaxation with guided imagery in people with PD. Researchers found that the tremor from PD is more pronounced during stress. During the study, some people were given guided imagery meditations. Others listened to relaxing music. A third group was encouraged to self-relax.5
The group of people who experienced the guided meditation all had a decrease in their tremor. The improvement continued for several hours. The group of people who listened to relaxing music had a slightly reduced tremor. The group who self-relaxed had no significant effect on their tremor. These findings suggest that guided imagery can supplement traditional medical treatment for tremor in people with PD.5
You May Like: Zhichan Capsule
Breathing Problems In Parkinsons Disease: A Common Problem Rarely Diagnosed
Parkinsons disease is the second most common neurodegenerative disorder after Alzheimers disease. It is characterized by bradykinesia tremor, rigidity, and postural instability. Potential non-motor manifestations of PD include depression, anxiety, constipation, overactive bladder symptoms, dementia, and sleep disturbances.
Although James Parkinson, in 1817, described breathing abnormalities in his Essay on the shaking palsy, there has been limited research on this important non-motor symptom.
People living with Parkinsons may present with a wide variety of respiratory symptoms, ranging from shortness of breath at rest to acute stridor. Shortness of breath can be very distressing for patients and clinicians alike. Multiple investigations may be undertaken, looking for infection, blood clots and heart problems. Although these potential causes of breathing abnormalities need to be excluded, clinicians must remember that PD itself and its medications can cause SOB and that normal investigations should not automatically lead to a diagnosis of anxiety, depression or lead to inappropriate treatment plans.
Several different patterns of breathing abnormality may be found in PD:
KM Torsney, D Forsyth
Don’t Miss: Can Parkinson’s Cause Incontinence
Central Case Management Brain Injury
Central Case Management has a clear focus: ensuring brain injury clients have the support that will help them work towards achieving their own goals and a better quality of life. The company, based in Duffield, Derbyshire, works with a range of brain injury professionals in creating and delivering bespoke support and rehabilitation to its clientsRead moreCentral Case Management Brain injury
Symptomatology Correlations Between The Diaphragm And Irritable Bowel Syndrome
The text reviews the diaphragms functions, anatomy, and neurological links in correlation with the presence of chronic symptoms associated to IBS, like chronic low back pain, chronic pelvic pain, chronic headache, and temporomandibular joint dysfunction, vagus nerve inflammation, and depression and anxiety. The interplay between an individuals breath dynamic and intestinal behaviour is still an unaddressed point and the paucity of scientific studies should recommend further research to better understand the importance of breathing in this syndrome.
This article explains the direct links between diaphragm dysfunction and: issues with the pelvic floor, jaw and tongue lower back pain headaches gastroesophageal reflux perceived pain emotional state and body image pain and inflammation the nervous system.
Read Also: Best Food For Parkinson Patient
Strength Training Helps Build Muscle Mass
Strength training can involve lifting weights, using machines at the gym, using your own body weight for resistance, or even using common household items like a milk jug filled with sand, the Parkinsons Foundation notes. Your strength training should focus on the following muscle groups:
- Core muscles
- Arm muscles
- Hands and wrists
In general, strength training should be done two to three times per week, but scheduled so that youre not targeting the same muscles on consecutive days, as your muscles need to rest and recover, the foundation advises.
As with stretching exercises, strength training can be performed while standing, sitting, or while on the ground.
The Wisconsin Parkinson Association recommends several exercises to help strengthen your grip and improve your reach. Tasks such as handwriting and reaching for items on higher shelves can be a challenge for people with Parkinsons disease, and hand exercises can help minimize these issues.
In general, resistance training helps build and maintain muscle mass, Subramanian says. The stronger you are, the more independent youll be.
Ropinirole Cause Of Shortness Of Breath Anxiety
- Gail BrightbillParticipant
My new neurologist took me off Rasagiline after a years use and prescribed Ropinirole. I also take Sinemet I immediately began to have extreme anxiety reactions when the two meds began to wear off after 2-3 hours. Has anyone else had this reaction?
- September 16, 2020 at 5:27 pm#19380Participant
I had a very similar reaction when I added Contam to my Sinemet doses recently. Ive had shortness of breath & heart palpitations while on Sinemet alone, too, but neither my neurologist nor my cardiologist seem to think thats the cause because thats not a common side effect. However, I am certain that its the med, and after my experience with adding the entacapone Im even more certain! Very frustrating though because it doesnt seem like I have any other options for PD symptom control other than DBS.
- You must be logged in to reply to this topic.
Newest Topics
- Active 4 hours, 42 minutes ago
Forums
Disclaimer:
Parkinsons News Today is strictly a news and information website about the disease. It does not provide medical advice, diagnosis or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
CONTACT US
Don’t Miss: What Is Vascular Parkinson’s Disease
Respiratory Dysfunction In Parkinsons Disease
Respiratory dysfunction has been associated with Parkinsons disease since it was first described in 1817, coronary artery disease and anxiety.Cited by: 4Parkinson.Org said: Some people with Parkinsons disease may experience shortness of breath, sudden difficulty with speech, a wearing-off symptom in Parkinson
What To Expect From Diagnosis
Theres no single test for Parkinsons, so it can take some time to reach the diagnosis.
Your doctor will likely refer you to a neurologist, who will review your symptoms and perform a physical examination. Tell your doctor about all the medications you take. Some of these symptoms could be side effects of those drugs.
Your doctor will also want to check for other conditions that cause similar symptoms.
Diagnostic testing will be based on your symptoms and neurologic workup and may include:
- blood tests
Read Also: Does Restore Gold Work For Parkinson’s Disease
What Are The Causes
People with Parkinsons may experience varied respiratory symptoms, ranging from shortness of breath without exertion to acute stridor, the sudden onset of high-pitched breathing sounds when taking a breath.1,3
Dysfunction can be caused by a variety of factors including physiological restrictive changes in the lungs, upper airway obstruction, and response to medications.1,3
Wendy Hawkins Working On Behalf Of A Client With Traumatic Brain Injury And Locked
Wendy Hawkins is a Brain Injury Case Manager for CA Case Management Ltd. Here she explains how Almond Care helped her to put in place a package of care, on behalf of a client who has a severe brain injury and now needs around the clock care at home. I provide case management to aRead moreWendy Hawkins Working on behalf of a client with traumatic brain injury and locked-in syndrome
Read Also: Parkinson’s Disease And Cough Medicine
Connection With The Nervous System
Important nerves both innervate and pass through the diaphragm, including the vagus nerve. The link to Parkinsons Disease and the vagus nerve has come to the fore in recent years. Indeed, my own perspective is that Idiopathic PD occurs when the Nervous System gets stuck in a death feigning or immobilizing response to perceived threats, resulting in inhibition of the ventral part of the vagus nerve, and giving control over to dorsal part of the nerve responsible for immobilized defensive states, see
Read Also: Parkinsons Double Vision
Shortness Of Breath Could Indicate Early Signs Of Parkinsons Disease Say Experts
Home»BlogHome » Shortness of breath could indicate early signs of Parkinsons disease, say experts
Changes in the way you breathe, such as shortness of breath and shallow breathing, could be an early sign of Parkinsons disease, experts have warned.
The symptom which may be confused with a symptom of the coronavirus forms one of the major indicators of the disease which progressively damages the brain over a period of time.
According to the Parkinsons Foundation, shortness of breath could be attributed to respiratory dyskinesia, anxiety, or aspiration pneumonia, which are all associated with the disease.
Some people with Parkinsons disease may experience shortness of breath. There is no clear cause underlying respiratory dysfunction in PD, its frequency or the effect that medications have on respiration, says the Foundation.
Shortness of breathing may be accompanied by a number of other early indicators, the charity warns. These include tremors in your finger, thumb, hand, or chin, smaller handwriting, loss of smell, trouble sleeping, trouble moving or walking, dizziness or fainting, or poor posture.
It can be hard to tell if you or a loved one has Parkinsons disease , said the Foundation.
No single one of these signs means that you should worry, but if you have more than one sign you should consider making an appointment to talk to your doctor.
For advice on the care and support of a loved one, please get in touch with our expert team today.
Read Also: What Medications Are Used For Parkinson’s Disease
Thanks For Signing Up
We are proud to have you as a part of our community. To ensure you receive the latest Parkinsons news, research updates and more, please check your email for a message from us. If you do not see our email, it may be in your spam folder. Just mark as not spam and you should receive our emails as expected.
How Physical Therapy Can Help
A physical therapist will complete a thorough evaluation of your mobility including balance, walking, strength, and endurance. In-person and virtual sessions will be scheduled to help assist with your rehabilitation journey.
A physical therapist can help with:
- education and self-management advice
- exercise routines to improve balance, walking, prevention of falls and what to do if you fall
- mobility around the house and community
- using assistive devices for mobility such as canes, walkers, or hiking poles
- Freezing what to do and prevention
- cognitive executive function
Also Check: Parkinson Silverware
Recommended Reading: Young Onset Parkinson’s Support Group
Parkinsons Diseasesigns And Symptoms
Parkinsons generally progresses slowly, sometimes taking years for symptoms to appear. The disease usually strikes adults over age 50, although it has been diagnosed as early as age 20. About 15 percent of Parkinsons patients have a family history of the disease.
Because it develops gradually, most people have many years of productive living after being diagnosed.
Some of the first symptoms commonly experienced with Parkinsons include the following:
- Rigidity Arms and legs become stiff and hard to move
- Tremors Rapid shaking of the hands, arms or legs
- Slowed movements Difficulty starting or completing movements, called bradykinesia
- Impaired balance Lack of balance or difficulty adjusting to sudden changes in position
These symptoms may make it difficult for you to walk, pick up and hold things, eat, write, or react quickly to prevent injury if you fall.
Other symptoms include difficulty speaking or swallowing, drooling, stooped posture, inability to make facial expressions, oily skin, cramped handwriting, shortness of breath, constipation, increased sweating, erectile dysfunction, difficulty sleeping, problems urinating and anxiety.
UCSF Health medical specialists have reviewed this information. It is for educational purposes only and is not intended to replace the advice of your doctor or other health care provider. We encourage you to discuss any questions or concerns you may have with your provider.
Symptoms That May Be Related To Pd
These symptoms can be associated with PD, but are also commonly associated with other medical conditions, so more testing is necessary. For example, weight loss may be associated with PD, but may also be a sign of a gastrointestinal problem or cancer. Pain may be associated with PD, but could be also due to arthritis, spinal stenosis, cancer, or a whole host of other causes.
There is a fourth category of non-motor symptoms that I would like to focus on now:
Read Also: Does Alcohol Affect Parkinson Tremors
Indirect Consequences Of Stress And Anxiety
The way we breathe is a powerful aspect of self-expression. Anxiety, emotional constipation, and other habits of mind and dysfunctional and self-limiting behavioural patterns might be associated with strong breathing patterns, especially shallow breathing.
Shallow breath is what we do when we literally hide . It is also what we do when we feel like we want to hide! Deep breathing is one of the main practical suggestions for fighting anxiety. Its a feedback loop.
Habitually breathing shallowly can be so subtle for so long that we dont even realize theres a problem until all the contributing factors and bad habits and vicious cycles are too deeply entrenched to break free a classic boiling frog kind of problem.
All of this is a rather complicated mess to try to sort out, but Im not going to leave you hanging. Here are several relevant, practical self-help articles. They all focus on what you can do about these issues:
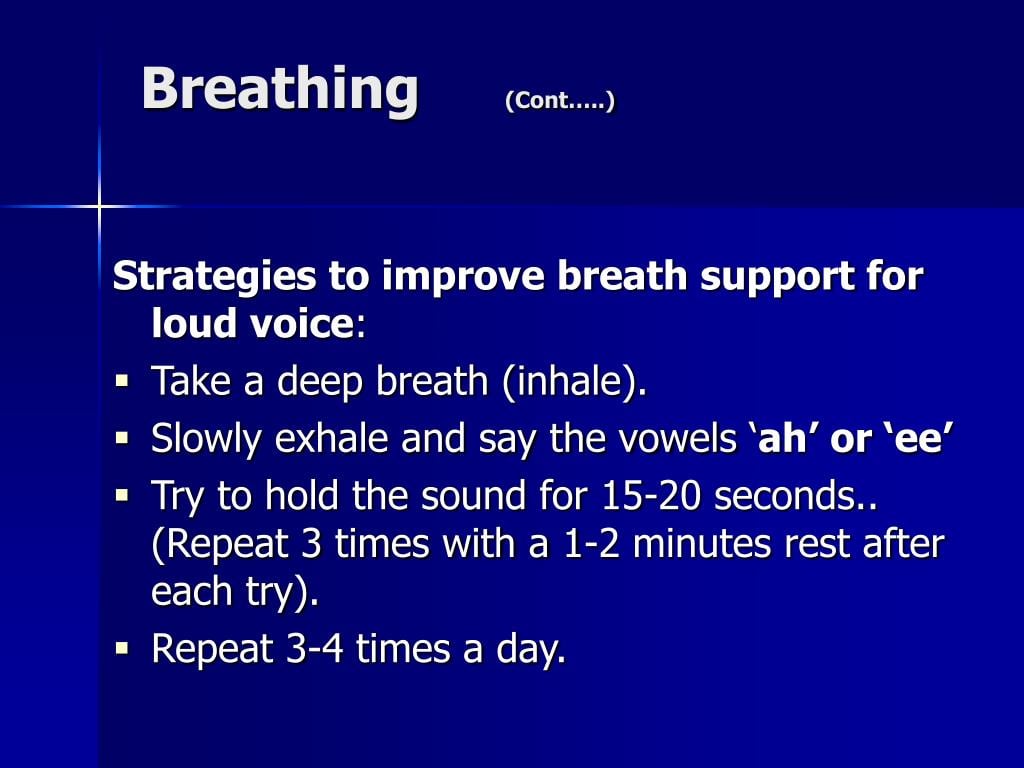
What Can We Do About It
While there may be no quick fixes for this, in my experience, it is possible to progressively improve matters, through daily diaphragm breathing exercises of the right kind. Due to faster disease progression and the myriad of other health issues associated with poor diaphragmatic breathing, I would recommend anyone with PD, but especially those newly diagnosed, to seek out gentle breathing techniques which they can personally work with, following Dr Fariass advice to avoid methods which try to force the diaphragm to move before it is ready, and commit to setting aside a little time each day to do the exercises. Two modalities Ive found personally beneficial are Dr Fariass own program of breathing exercises, which are tailored specifically for people with dystonia and PD, and a self-care technique called Block Therapy, developed by Deanna Hanson, which isnt specific to PD, but is designed to gently restore diaphragm function. Both of these only require a few minutes a day, every day, for improvements to slowly but surely accrue. However, note that these are generally part of paid-for online subscription courses, although Deanna has free resources explaining how to do the diaphragmatic breathing exercise part of Block Therapy.
Another modality that I am currently considering, as it may be helpful since it is also based on very gentle breathing exercises, is the Buteyko Method.
Also Check: Exercise For Freezing In Parkinson’s
Deep Brain Stimulation And Respiratory Failure
DBS is an effective strategy for the treatment of advanced PD, thus improving motor fluctuations and bradykinesia.
Nonetheless, the classical target of the subthalamic nucleus -DBS reserves stimulation-induced side effects in the long-term period, comprising gait and speech impairment, as well as a progressively worsening of tremor. In this scenario, only few papers have specifically investigated respiratory failure. In particular, STN-DBS may increase the risk of a fixed epiglottis and modify velopharyngeal control these effects seem to strictly depend on frequency parameters, with low-frequency stimulation leading to a clinical improvement, whereas higher frequencies are associated with a detrimental effect on velopharyngeal control .
In support of this view, Hammeret al. have recently found that in STN-DBS patients, respiratory changes do not correlate with limb function, but speech-related respiratory and laryngeal control may benefit when the stimulation is delivered at low frequencies and shorter pulse width . In addition to stimulation frequency, other factors may account for these correlations, including variability in localisation of the active DBS electrodes, individual variability in somatotopic organisation of STN, stimulation fields and potential current spread beyond the STN target . Data on the relationship between respiratory changes and novel DBS targets, such as the pedunculopontine nucleus , have not been extensively reported so far.
Origins Of Breathing Disorders

The book by Leon Chaitow and co-authors cited above explains how breathing disorders are intrinsically linked to chronic stress and anxiety. The shallow, fast chest breathing through the mouth is a hallmark of the body preparing itself for the exertion of flight or fight due to a stress response. While this adaptive in acute stress situations, when stress is chronic and the body is spending a lot of time in fight or flight, the associated pattern of breathing becomes habitual, and eventually the system gets stuck in the new equilibrium of the CO2 intolerant state. However, the vicious circle work both ways, because overbreathing itself puts the body into a stress response state and feeds anxiety. A very good tutorial about the two way links between anxiety and breathing patterns is given by Robert Litman in the video below.
It is not surprising therefore that people with PD can present with disordered breathing associated with chronic stress and anxiety, since there are very significant overlaps between the other symptoms of chronic stress and those of Parkinsons Diseases, and ingrained fight or flight behaviours are common to the pre-diagnosis background histories of people with PD. Conversely, it is important to note that techniques which have been developed to treat breathing disorders should also help to decrease the symptoms of PD, including reduction of anxiety and increasing resilience to stress.
Recommended Reading: Yopd Life Expectancy
You May Like: Rls And Parkinson’s Disease