The Weird Dream Symptom That Made Alan Alda Suspect He Had Parkinsons Disease
Actor Alan Alda has revealed that he was diagnosed with Parkinson’s disease over three years ago. In an interview on CBS This Morning on Tuesday, Alda said he decided to speak publicly about his diagnosis because his thumb was twitching in recent TV interviews and he thought people would be curious.
But before his official diagnosis, it was a much weirder symptom that tipped him off.
I was having a dream that someone was attacking me and I threw a sack of potatoes at him, but what I was really doing was throwing a pillow at my wife, Alda, 82, said, noting that he didn’t have any other symptoms at the time. It wasn’t until months later that he noticed his thumb twitching.
So, Alda asked for a brain scan and was eventually diagnosed with the disease. Although there isn’t a specific test that can be used to definitively diagnose Parkinson’s, doctors may use brain scans, blood tests, and other exams to rule out other options.
Parkinson’s disease is a progressive disorder that affects the nerves and, consequently, movement, the Mayo Clinic explains. Although symptoms may start mildly, they become more severe over time and may include tremors as well as muscle stiffness, slowed movement, impaired balance, and changes in speech and/or writing. The exact cause of the disorder is unknown, but age, genes, and environmental factors may play a role.
Twitter content
Related:
The Following Tips Can Help You And Your Partner Manage Rbd:
- Talk with your partner. It is essential to maintain an open dialogue about sleep symptoms that your partner may not be aware of. Since RBD can be physically dangerous, it is especially important to find the right management options for both of you.
- Go to doctors appointments. You may notice new symptoms, worsening symptoms, or improvement of symptoms that your partner with Parkinsons does not notice. Since RBD can be potentially dangerous to you or your partner, it is critical to talk with your doctor about the best options for your specific situation.
- A 2010 study found that out of 242 people living with Parkinsons, between 31.8% and 65.2% had undeclarednonmotorsymptoms. This research highlights the importance of knowing about non-motor symptoms so that both people with Parkinsons and their care partners know what to talk with physicians about.
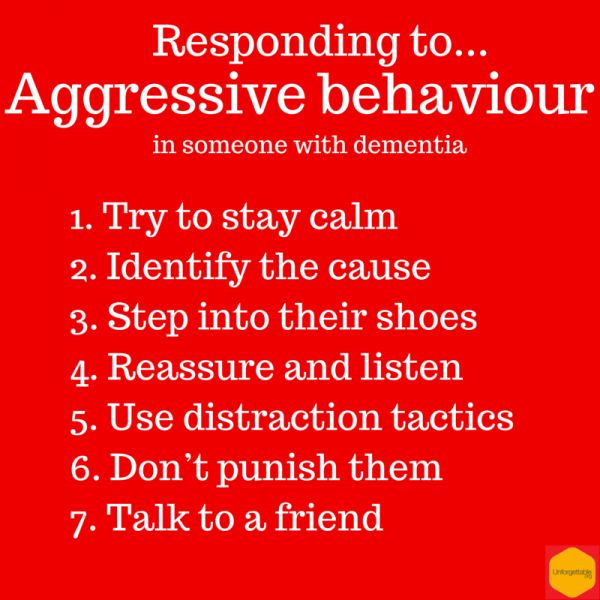
Determining The Cause Of The Behavior
Taking the time to listen and assess the situation can help pinpoint the source of anxiety and intent of the behavior. Is there a pattern to the behavior? Has anything changed in the patient’s health, environment, treatment plan, or daily routine?
Ask these kinds of questions when determining the cause of violent behavior and remember: Don’t take it personally. It may seem like the dementia patient is attacking you, but really they are anxious and you happen to be around.
When behavioral disturbances occur, give the person space you may need to leave the room until you’re both calm, according to the Alzheimer’s Society. Showing your anxiety may make the dementia patient more agitated, so make sure you can approach them calmly. Tell the person you can see they’re upset.
Read Also: Rehabilitation Programs For Parkinson’s Disease
More Drugs Is More Dopamine And Less Activity
Treated animals showed less head-shoulder motility and more sitting, and imaging of dopamine receptor binding indicated an association between this decrease in activity and an increased availability of dopamine. Both doses of the drug reduced the binding of dopamine to its receptor and made the animals less active in a dose-depended manner. The findings also suggest that the decline in activity after L-DOPA administration may be due to the drugs effect on the rate of behavioral habituation to a novel environment.
Is Parkinsons Disease Fatal
Parkinsons disease is not fatal itself, however, complications that come with the disease can be serious. For example, some injuries caused by falling or issues associated with dementia can be fatal.
Furthermore, some people who have Parkinsons disease may experience difficulty swallowing. This may lead to aspiration pneumonia which is a condition that causes foods or other foreign objects to be inhaled into the lungs.
Read Also: How To Care For Someone With Parkinson’s Disease
How Is Parkinsons Disease Dementia Diagnosed
No single test can diagnose Parkinsons disease dementia. Instead, doctors rely on a series or combination of tests and indicators.
Your neurologist will likely diagnose you with Parkinsons and then track your progression. They may monitor you for signs of dementia. As you get older, your risk for Parkinsons dementia increases.
Your doctor is more likely to conduct regular testing to monitor your cognitive functions, memory recall, and mental health.
Psychosis & Advanced Pd
This set of symptoms encompasses hallucinations, delusions and paranoia. Symptoms of psychosis can be very variable in their manifestation and severity. In addition, the degree of insight into the psychotic thought or vision can be variable as well. As mentioned above, psychosis can lead to behavioral symptoms and needs to be explored as a possibility when behavioral symptoms arise. They can also exist independently of any behavioral symptoms. People with PD are often very reluctant to report these symptoms, for fear that they will be perceived as crazy.
Of note, hallucinations are a risk factor for dementia and dementia is a risk factor for hallucinations.
Also Check: Drugs Prescribed For Parkinson’s Disease
Tips For Living With Hallucinations
It is important for people with PD to talk about hallucinations with their family and care team, because they are manageable and can be troublesome if not treated. Discuss all possible symptoms with your doctor, no matter how minor, rare or bizarre you may think they are.
- Good lighting and stimulating activities in the evening can help keep hallucinations at bay.
- While a hallucination is occurring, caregivers can help their loved one by reassuring them that they will be safe and validating their partners experience. For example, say, Ill take the cat outside instead of arguing that there is no cat.
Risk Of Experiencing These Behaviours
It is important that all people with Parkinsons are assessed for any potential risk of impulsive and compulsive behaviour before they start taking their medication. This is an important discussion to have with your specialist.
Research has shown that around 17% of people with Parkinsons who take dopamine agonists experience impulsive and compulsive behaviour. For a small number of people, levodopa, has also been shown to have similar side effects. The research suggests that 7% of people who take these other kinds of medication are affected.
Evidence suggests that you may be more likely to experience impulsive and compulsive behaviour if you are:
- Male
- Someone with a history of addictive behaviour
- Someone who has a family history of gambling or alcohol abuse
Its important to emphasise that not everyone will experience this behaviour. It is a possible side effect. It should not put you off taking your medication. Your specialist will assess your risk of impulsive and compulsive behaviours and you can work together to find the most appropriate treatment option for you.
Recommended Reading: Shirts For Parkinson’s Patients
What Causes Parkinson Disease
Parkinson disease arises from decreased dopamine production in the brain. The absence of dopamine makes it hard for the brain to coordinate muscle movements. Low dopamine also contributes to mood and cognitive problems later in the course of the disease. Experts don’t know what triggers the development of Parkinson disease most of the time. Early onset Parkinson disease is often inherited and is the result of certain gene defects.
Side Effects Of Common Pd Treatment
Shortage of dopamine in the brain is the well-known cause of PD. L-DOPA is often used to treat PD, but while it initially compensates for the dopamine deficiency, inhibitory feedback eventually leads to more dopamine depletion, resulting in dyskinesia , motor fluctuations, and the wearing-off of the effects of the medication.
You May Like: Parkinson’s Coughing At Night
What Are Hallucinations
Hallucinations are when someone sees, hears or feels something that is not actually there. They are best described as deceptions or tricks played by the brain that involve the bodys senses. Hallucinations are not dreams or nightmares. They happen when the person is awake and can occur at any time of day or night.
Thanks For Signing Up
We are proud to have you as a part of our community. To ensure you receive the latest Parkinsons news, research updates and more, please check your email for a message from us. If you do not see our email, it may be in your spam folder. Just mark as not spam and you should receive our emails as expected.
Don’t Miss: Fluid Retention And Parkinson’s
Medications Used For Treating Psychosis
Antipsychotic agents are designed to balance abnormal chemical levels in the brain. Up until the 1990s, the use of antipsychotics in PD was controversial because the drugs used until that time work by reducing excess dopamine. This alleviated psychosis but caused dramatic worsening of PD motor symptoms.
Fortunately, medications that are better tolerated by people with PD are now available. Today, there are three antipsychotic medications considered relatively safe for people with PD: quetiapine , clozapine and the newest agent, pimavanserin . They cause limited worsening of PD while treating hallucinations and delusions.
Effects Of Low Dopamine On Your Health
The perfect balance of dopamine can help you focus, learn, and stay motivated while dopamine deficiency can make it difficult to concentrate, make you feel less enthusiastic, and can cause movement difficulties.
Neurotransmitters such as dopamine communicate with our brain cells. When the communication is disrupted, the messages are lost. The consequences of this can result in many health conditions including Parkinsons disease, depression, anxiety, etc.
Neurotransmitters are responsible to transport messages and since these neurotransmitters can affect areas of the brain, any kind of miscommunication or error in transmission can trigger moods and behaviors such as anger, aggression, mood swings, anxiety, and so on.
Read Also: Assisted Living For Parkinson’s Patients
Read Messages From Our Community Related To Mental Health In Advanced Pd:
My Dad fights aggressively when his aides try to get him to do something he doesnt want to. He gets so angry and is so strong it can take many people to restrain him.
My Mom lives at home, but constantly thinks that she is somewhere else and wants to go home. She becomes irritated and angry with the family because she says that we are holding her hostage.
My husband is verbally abusive towards me. This is an entirely new aspect to his personality. He was always very loving. Now he is aggressive.
My wife is severely depressed. Although she can get out of bed with help, she would rather stay in bed and do nothing. She also doesnt seem to mind that she is doing nothing all day.
Often, my brother doesnt recognize me when I visit. Last week, I saw my brother in the morning, but when I spoke with him on the phone later on in the evening, he mentioned that he had not seen me in a long while.
These quotes highlight a set of very problematic issues in advanced PD which include cognitive decline/dementia, depression, apathy, anxiety, psychosis , and behavior problems . One person often has a mixture of these symptoms and the symptoms can be inter-related.
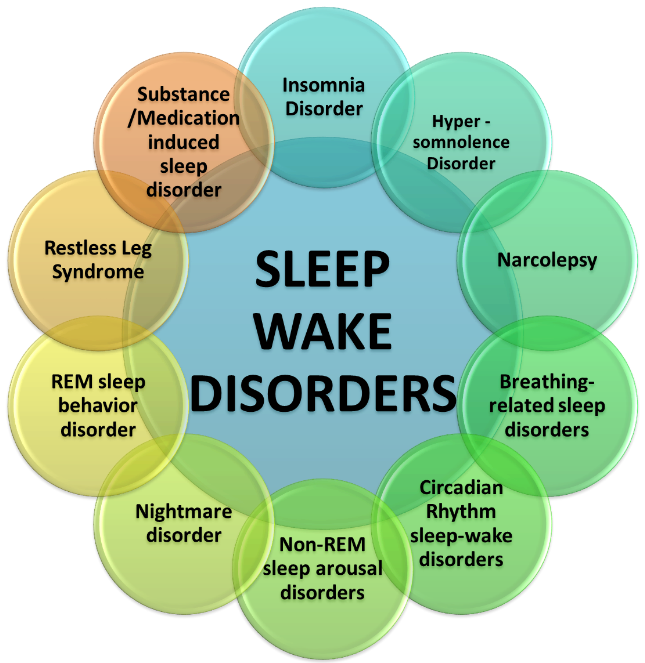
New Pd Subtypes In Development
New classifications of patients with PD may improve both diagnostics and the accuracy of predicted outcomes.
A newly developed system of three subtypes focuses on the severity of key motor and non-motor symptoms and highlights RBD as a relevant non-motor marker.
Thomas Warner MD told Medscape Medical News recently that We have found that it is possible to accurately predict prognosis, disability, and survival of patients with Parkinson’s disease by classifying them into different clinical subtypes at the time of diagnosis.
Warner, senior author of a new study published in January 2019 at JAMA Neurology, defines these subtypes as:
People with PD who also have RBD will likely fall into subtype 2. However, this distinct symptom can help chart a clearer treatment path and prepare you for a more aggressive clinical approach.
Also Check: What Medications Are Used To Treat Parkinson’s Disease
A Caregivers Experiences With Pd Psychosis
A commonly asked question is, How soon after diagnosis are symptoms of PD psychosis experienced, and what are the beginning signs? My husband had always been an exceptionally calm and affectionate persona tower of strength for friends and family. He enjoyed good health despite his advancing years. However, he died of Parkinson’s at age 91 with full-blown PD psychosis.
He began having breathing difficulties at night and started using a breathing aid, but he couldn’t tolerate it. When the tremors started, he was diagnosed with Parkinsonism. About four years later, PD was confirmed. With medications and exercise, we were able to live a normal life for a while.
The first undeniable signs of psychosis appeared after his 90th birthday, when he started hearing music that wasnt there. For him, it was the same songs repeating over and over again. His doctors tried several medications without any success. He tolerated this bothersome affliction with good humor, though, and even cracked jokes about it. A few months later, the hallucinations started. At first, they were benign, but they became increasingly scarier. However, he was still in touch with reality. His memory was goodsometimes better than mineand he was very faithful to his exercise regimen.
As his disease progressed and family rallied to our sides, I discovered that it was best for me to live in the moment. Don’t think about the past or the future, I would say to myself.
Impulsive And Compulsive Behaviours In Parkinson’s
Impulsive and compulsive behaviours are a possible side effect of some Parkinsons drugs. This information describes what they are, why they might happen and how to manage them.
In this information we use the term impulsive and compulsive behaviours to include all the different types of behaviour you may experience. But you may also hear the phrase Impulse Control Disorder used to describe some of these behaviours.
Key points:
-
Not everyone who takes Parkinsons medication will experience impulsive and compulsive behaviours, so these side effects should not put you off taking your medication to control your symptoms.
-
Impulsive and compulsive behaviours can have a serious impact on the person affected and those around them so speak to your healthcare professional as soon you notice any changes.
-
Asking your specialist to make changes to your medication regime or adjust the doses that you take is the easiest way to control these behaviours.
People who experience impulsive and compulsive behaviours cant resist the temptation to carry out an activity often one that gives immediate reward or pleasure.
Impulsive and compulsive behaviours happen when a person has an overwhelming urge to behave in a certain way. They will often carry out their behaviour repetitively as a way to reduce the worry or tension they get from their urge. Some people continue to act in this way without thinking and even when they no longer get any pleasure or reward from the activity.
Addictive gambling
Also Check: How Long Does A Person Live With Parkinson’s Disease
Other Types Of Impulsive And Compulsive Behaviours
Punding
This is when someone does things such as continually handling and sorting objects. They may be fascinated with taking technical equipment apart or collecting a type of object.
This behaviour can mean people dont get enough sleep. It can also cause social problems with family or at work. If someone collects objects or takes machinery apart without knowing how to put it back together, it can also have a big financial impact, as theyll need to spend money to buy new objects or getting equipment repaired.
Some people also experience other behaviours such as compulsive singing, writing, smoking, reckless driving or doing crafts
Hoarding
This happens when someone feels that they must continue to keep items that they dont need. The thought of getting rid of the items may make someone feel upset.
Addiction to Parkinsons medication Some people with Parkinsons have a compulsion to take more medication than they need to control their symptoms because they are addicted to the way it makes them feel.
If a person is taking too much medication and their healthcare professional attempts to reduce it to the levels theyre supposed to take, this may cause unpleasant feelings, anxiety and cravings. It may also cause reduced mobility. A person may refuse to accept this, sometimes resulting in aggression, secret hoarding or requests for repeat prescriptions.
The number of people who may experience impulsive and compulsive behaviours may vary in research because of:
Open Field Motor And Exploratory Behaviors

In 2014, Susanne Nikolaus and her colleagues published their research on the influence of L-DOPA on the binding of dopamine to its receptor in relation to motor and exploratory behavior in rats. Nikolaus tested two different dosages of the drug. To assess behaviors, an open field set-up and automated video tracking software were used. The distance travelled was monitored by EthoVision XT and in addition, several specific behaviors were rated: ambulation, sitting still, rearing, head-shoulder motility to assess motor activity and non-selective attention, and grooming*.
Recommended Reading: How To Tell Difference Between Parkinson’s And Essential Tremor