Patients With Parkinsons Disease Have Elevated Tmj Disorder Risk
The progressive nervous system condition Parkinsons disease affects an estimated 10 million Americans each year. Characterized by muscle rigidity and tremors, Parkinsons disease has no known cure. Now a new study is linking Parkinsons to another painful condition: temporomandibular joint disorder.
Temporomandibular joint disorder, or TMJD, is a condition of the temporomandibular joints of the jaw. It affects an estimated 10 million Americans. Much like Parkinsons disease, TMJ disorder can cause muscle stiffness, but its localized in the jaw, neck, back and shoulders.
Dr. Alexandra George practices dentistry in Wexford, Pennsylvania, where she treats patients with temporomandibular joint disorder. She says that, although the conditions are different, the symptoms of temporomandibular joint disorder have their similarities to Parkinsons disease.
Parkinsons and TMJ disorder both cause muscle stiffness, but their origins are very different, says George.
But now, thanks to a new study, researchers have revealed a new connection between the two conditions. Published in the journal PLoS One, the research out of Taiwan shows that persons with Parkinsons disease may have an elevated risk of developing TMJ disorder.
According to George, the data revealed that 32 cases of TMJ disorder appeared in the Parkinsons disease group and 50 in the larger population meaning those with Parkinsons were at far higher odds of developing TMJ disorder than those in the control group.
The Association Between Parkinsons Disease And Temporomandibular Disorder
- Ya-Yi Chen,
Roles Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Writing original draft, Writing review & editing
Affiliations Department of Stomatology, Tungs Taichung MetroHarbor Hospital, Wuchi, Taichung, Taiwan, Republic of China, Institute of Genomics and Bioinformatics, College of Life Sciences, National of Chung Hsing University, Taichung, Taiwan, Republic of China
- Hueng-Chuen Fan,
Roles Data curation, Formal analysis, Methodology, Resources, Supervision, Writing original draft, Writing review & editing
Affiliations Department of Pediatrics, Tungs Taichung MetroHarbor Hospital, Wuchi, Taichung, Taiwan, Republic of China, Department of Medical Research, Tungs Taichung MetroHarbor Hospital, Wuchi, Taichung, Taiwan, Republic of China, Department of Rehabilitation, Jen-Teh Junior College of Medicine and Management, Hou-Loung Town, Miaoli, Taiwan, Republic of China
-
Affiliation Department of Surgery, Tungs Taichung MetroHarbor Hospital, Wuchi, Taichung, Taiwan, Republic of China
Can Parkinsons Disease Be Prevented
Unfortunately, no. Parkinsons disease is long-term disease that worsens over time. Although there is no way to prevent or cure the disease , medications may significantly relieve your symptoms. In some patients especially those with later-stage disease, surgery to improve symptoms may be an option.
Read Also: Does Parkinson’s Cause Neuropathy
Ways Of Better Ensuring Good Dental Care In Parkinsons Reviewed
Another PD issue that can affect oral health is swallowing. Dry mouth and decreased strength in jaw, tongue, or facial muscles affect swallowing. Eating nutritious foods because of problems with chewing and swallowing can lead to more dental problems such as cavities and mouth ulcers.
Bev had speech therapy for swallowing issues that started in the past year. The therapist recommended taking smaller bites when chewing and before swallowing, eating more slowly before swallowing, and sitting upright with her head up when eating.
Jaw exercises to strengthen muscles in the mouth and jaw may also help PD patients with improved quality of life and oral health.
A literature review titled Evidence-Based Recommendations for the Oral Health of Patients with Parkinsons Disease, published last March in the journal Neurology and Therapy, concluded that Patients with PD had reduced quality of oral health and hygiene, and high prevalence of gingival recession , periodontal disease , dental calculus , tooth decay, tooth mobility and loss, drooling, xerostomia , dysphagia and temporomandibular disorders.
Because of the challenges of oral health for people with PD, routine consultations with an oral surgeon in addition to a general dentist may be recommended.
What Causes Parkinsons Disease
Parkinsons disease occurs when nerve cells, or neurons, in an area of the brain that controls movement become impaired and/or die. Normally, these neurons produce an important brain chemical known as dopamine. When the neurons die or become impaired, they produce less dopamine, which causes the movement problems of Parkinsons. Scientists still do not know what causes cells that produce dopamine to die.
People with Parkinsons also lose the nerve endings that produce norepinephrine, the main chemical messenger of the sympathetic nervous system, which controls many automatic functions of the body, such as heart rate and blood pressure. The loss of norepinephrine might help explain some of the non-movement features of Parkinsons, such as fatigue, irregular blood pressure, decreased movement of food through the digestive tract, and sudden drop in blood pressure when a person stands up from a sitting or lying-down position.
Many brain cells of people with Parkinsons contain Lewy bodies, unusual clumps of the protein alpha-synuclein. Scientists are trying to better understand the normal and abnormal functions of alpha-synuclein and its relationship to genetic mutations that impact Parkinsons disease and Lewy body dementia.
Don’t Miss: Boxing And Parkinson’s Disease
How Is Parkinsons Disease Treated
There is no cure for Parkinsons disease. However, medications and other treatments can help relieve some of your symptoms. Exercise can help your Parkinsons symptoms significantly. In addition, physical therapy, occupational therapy and speech-language therapy can help with walking and balance problems, eating and swallowing challenges and speech problems. Surgery is an option for some patients.
Will My Parkinsons Mean I Need To See A Specialist Dentist
Its important to tell your dentist that you have Parkinsons and how it affects you.
Most dentists will be able to treat people at all stages of the condition.
But tell your dentist about issues you experience because of Parkinson’s. For example, you may find you move a lot during an appointment if you have a tremor or dyskinesia.
If your dentist feels you need specialist care, they will refer you to a colleague on the General Dental Councils special care register.
If you have to have dental surgery, talk to your dentist about Parkinsons symptoms you experience and how these may affect your operation.
You should also tell your dentist about your drug regime so that you continue to get the right dose when you have your operation.
If youve had deep brain stimulation and you now need to have a dental operation, you will need to take antibiotics. This will help make sure that you dont get an infection or another issue that could affect your deep brain stimulation device.
If you wear dentures Parkinsons may mean you have difficulty controlling them. This could be because of:
- problems controlling your facial muscles
- loss of muscle tone
Recommended Reading: Bicycle Therapy For Parkinson’s Disease
Data Analysis And Statistics
Descriptive data were calculated for all variables. Subsequently, Chi-square test was used to test possible association between the presence of PD/PR and the following variables: orofacial pain, possible TMD-pain, possible sleep or awake bruxism, jaw locking, and tooth wear. Differences between the patient group and the control group were tested with independent sample t test for the CPI. Statistical analyses were performed with IBM SPSS statistics, version 24. The level of significance was set at α < 0.05.
Breathing & Respiratory Difficulties
Some people with Parkinsons disease may experience shortness of breath. There is no clear cause underlying respiratory dysfunction in PD, its frequency or the effect that medications have on respiration. Several reasons for shortness of breath in PD include:
- Wearing off is a common experience among people with PD who have been taking levodopa for several years. These occur when the medication benefit wears off and PD symptoms return before the next dose.
- Respiratory dyskinesia refers to an occurrence of irregular and rapid breathing when levodopa medications reach their peak effect. These may accompanied by involuntary body movements, typically experienced as dyskinesia.
- Anxiety is a common symptom of PD that may also exacerbate shortness of breath, whether by itself or as a consequence of wearing off of the medication.
- Aspirationpneumonia is a pneumonia that develops after food or liquid goes down the wrong pipe. Advanced PD can increase the risk of swallowing difficulties, choking and aspiration pneumonia.
- Non-PD health issues include conditions such as asthma, allergies, lung disease, heart disease and other conditions that may cause shortness of breath.
Don’t Miss: Nad Therapy For Parkinson’s Disease
How Is Parkinsons Disease Diagnosed
Diagnosing Parkinsons disease is sometimes difficult, since early symptoms can mimic other disorders and there are no specific blood or other laboratory tests to diagnose the disease. Imaging tests, such as CT or MRI scans, may be used to rule out other disorders that cause similar symptoms.
To diagnose Parkinsons disease, you will be asked about your medical history and family history of neurologic disorders as well as your current symptoms, medications and possible exposure to toxins. Your doctor will look for signs of tremor and muscle rigidity, watch you walk, check your posture and coordination and look for slowness of movement.
If you think you may have Parkinsons disease, you should probably see a neurologist, preferably a movement disorders-trained neurologist. The treatment decisions made early in the illness can affect the long-term success of the treatment.
While There Is No Cure For Pd Early Diagnosis Is Still Key
Individuals with PD experience tremors because, as the disease progresses, it damages neurons in the brain. These nerve cells are responsible for the production of dopamine, a neurotransmitter that keeps the body’s motor functions operating smoothly. As more cells become damaged or die, communication in the basal ganglia region of the brain becomes frayed. By the time PD patients experience motor symptoms, between 60 and 80 percent of dopamine-generating neurons have already been damaged or destroyed, experts say.
That’s why it’s so essential to seek immediate medical care if you suspect PD symptoms. As the Mayo Clinic notes, there is currently no cure for Parkinson’s, but a combination of medication and lifestyle interventions can help to mitigate your symptoms. Additionally, studies have found that up to 90 percent of patients with disabling tremors see improvements in their symptoms following deep brain stimulation surgery. The sooner you seek out medical evaluation, the sooner you can find a care strategy that works for you.
Recommended Reading: Does Alan Alda Have Parkinson’s
Is Parkinsons Disease Inherited
Scientists have discovered gene mutations that are associated with Parkinsons disease.
There is some belief that some cases of early-onset Parkinsons disease disease starting before age 50 may be inherited. Scientists identified a gene mutation in people with Parkinsons disease whose brains contain Lewy bodies, which are clumps of the protein alpha-synuclein. Scientists are trying to understand the function of this protein and its relationship to genetic mutations that are sometimes seen in Parkinsons disease and in people with a type of dementia called Lewy body dementia.
Several other gene mutations have been found to play a role in Parkinsons disease. Mutations in these genes cause abnormal cell functioning, which affects the nerve cells ability to release dopamine and causes nerve cell death. Researchers are still trying to discover what causes these genes to mutate in order to understand how gene mutations influence the development of Parkinsons disease.
Scientists think that about 10% to 15% of persons with Parkinsons disease may have a genetic mutation that predisposes them to development of the disease. There are also environmental factors involved that are not fully understood.
Medication Side Effects And The Gut

The interactions between PD medication ingestion and the gut can play a major role in motor fluctuations the phenomenon in which a patients response to Levodopa varies widely during the day. A recent APDA webinar helps to explain this interplay.
Delayed gastric emptying
Delayed gastric emptying can interfere with medication absorption. Medication doses that are ingested by mouth may sit in the stomach before being transported to the small intestine where they are absorbed. Delayed gastric emptying could be responsible for dose failures when a dose of medication does not have a robust enough effect.
Protein effect
Levodopa crosses the wall of the small intestine via a molecule in the intestinal wall that transports amino acids, the building blocks of protein. When dietary protein is also present in the small intestine, then there are fewer transporters available for Levodopa to use. A patient may therefore experience the protein effect, in which he or she feels that medication is not as effective after a high-protein meal. Sources of dietary protein include: beef, chicken, pork, fish, eggs, nuts and dairy.
Helicobacter pylori and small intestinal bacterial overgrowth
About a third of PD patients are infected with Helicobacter pylori, a common bacteria which can cause gastritis and ulcers. Infection with Helicobacter pylori has been linked to worsened motor fluctuations. It can be diagnosed with a urea breath test that analyzes exhaled air.
Also Check: What Other Diseases Mimic Parkinson’s
Symptoms Of Parkinsons Disease
Parkinsons disease has four main symptoms:
- Tremor in hands, arms, legs, jaw, or head
- Stiffness of the limbs and trunk
- Slowness of movement
- Impaired balance and coordination, sometimes leading to falls
Other symptoms may include depression and other emotional changes difficulty swallowing, chewing, and speaking urinary problems or constipation skin problems and sleep disruptions.
Symptoms of Parkinsons and the rate of progression differ among individuals. Sometimes people dismiss early symptoms of Parkinsons as the effects of normal aging. In most cases, there are no medical tests to definitively detect the disease, so it can be difficult to diagnose accurately.
Early symptoms of Parkinsons disease are subtle and occur gradually. For example, affected people may feel mild tremors or have difficulty getting out of a chair. They may notice that they speak too softly, or that their handwriting is slow and looks cramped or small. Friends or family members may be the first to notice changes in someone with early Parkinsons. They may see that the persons face lacks expression and animation, or that the person does not move an arm or leg normally.
People with Parkinsons often develop a parkinsonian gait that includes a tendency to lean forward, small quick steps as if hurrying forward, and reduced swinging of the arms. They also may have trouble initiating or continuing movement.
What Are The Primary Motor Symptoms Of Parkinsons Disease
There are four primary motor symptoms of Parkinsons disease: tremor, rigidity, bradykinesia and postural instability . Observing two or more of these symptoms is the main way that physicians diagnose Parkinsons.
It is important to know that not all of these symptoms must be present for a diagnosis of Parkinsons disease to be considered. In fact, younger people may only notice one or two of these motor symptoms, especially in the early stages of the disease. Not everyone with Parkinsons disease has a tremor, nor is a tremor proof of Parkinsons. If you suspect Parkinsons, see a neurologist or movement disorders specialist.
Tremors
Rigidity
Bradykinesia
Postural Instability
Walking or Gait Difficulties
Dystonia
Vocal Symptoms
Don’t Miss: Parkinson’s Disease Environmental Factors
What Lifestyle Changes Can I Make To Ease Parkinsons Symptoms
Exercise: Exercise helps improve muscle strength, balance, coordination, flexibility, and tremor. It is also strongly believed to improve memory, thinking and reduce the risk of falls and decrease anxiety and depression. One study in persons with Parkinsons disease showed that 2.5 hours of exercise per week resulted in improved ability to move and a slower decline in quality of life compared to those who didnt exercise or didnt start until later in the course of their disease. Some exercises to consider include strengthening or resistance training, stretching exercises or aerobics . All types of exercise are helpful.
Eat a healthy, balanced diet: This is not only good for your general health but can ease some of the non-movement related symptoms of Parkinsons, such as constipation. Eating foods high in fiber in particular can relieve constipation. The Mediterranean diet is one example of a healthy diet.
Preventing falls and maintaining balance: Falls are a frequent complication of Parkinson’s. While you can do many things to reduce your risk of falling, the two most important are: 1) to work with your doctor to ensure that your treatments whether medicines or deep brain stimulation are optimal and 2) to consult with a physical therapist who can assess your walking and balance. The physical therapist is the expert when it comes to recommending assistive devices or exercise to improve safety and preventing falls.
Shooting Pain And Paraesthesia
Radicular pain is a sharp pain that shoots down a limb and often affects fingers or toes. Paraesthesia is sometimes described as a feeling of pins and needles or perhaps numbness in a limb which has fallen asleep. Such pain is usually related to trapped nerves in the spinal cord and can feel similar to an electric shock, a tingling or a burning sensation.
Treatment: Painkillers and exercise will generally settle the pain. If not your specialist may refer you for tests such as an MRI scan to check for a trapped nerve in the spinal cord.
Don’t Miss: What Age Parkinson’s Disease
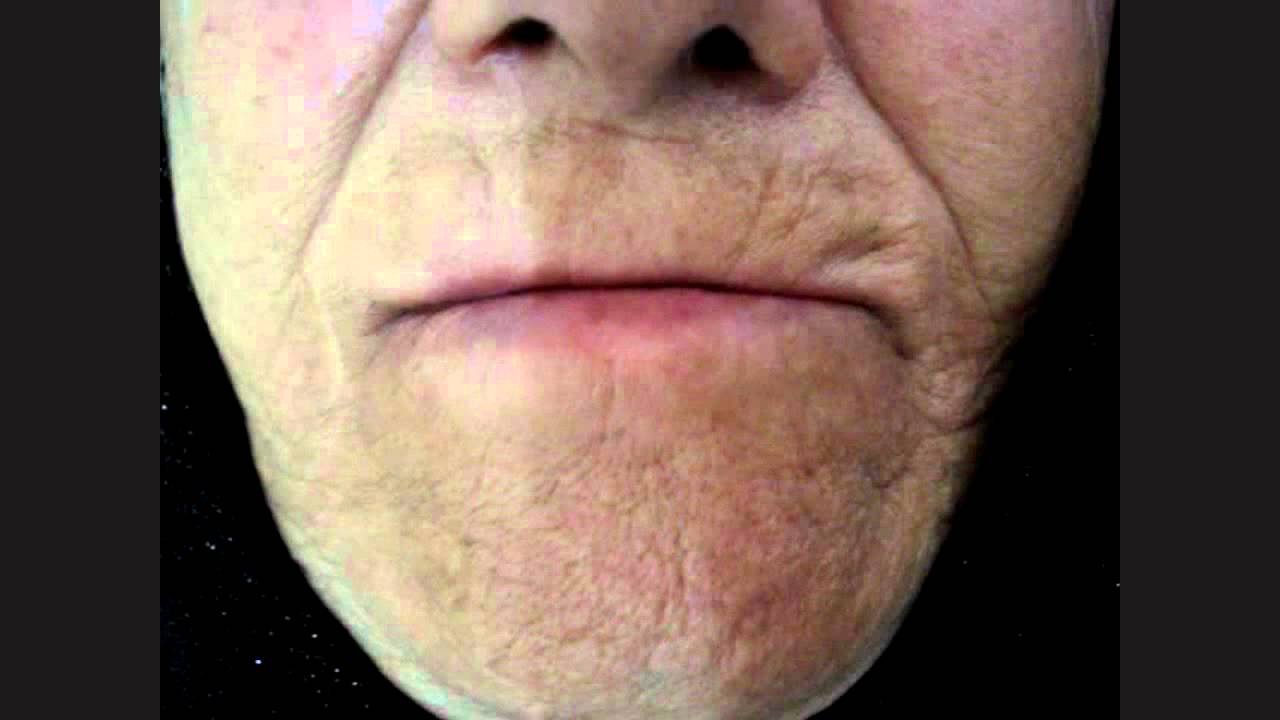
What Does Tardive Dyskinesia Look Like
TD looks like different, uncontrollable movements and patterns of the limbs and face. Sometimes referred to as stereotypy, the activity can be patterned, repetitive, and rhythmic movements that can involve one or more body parts. More than 3/4 of those with TD experience oral-facial-lingual stereotypic movements .1 The Baylor College of Medicine Movement Disorders Clinic conducted a videotape review of 100 people with tardive dyskinesia. The evaluation showed that the majority experienced irregular and chaotic movements in the OFL region, including lip smacking, chewing and other tongue and mouth movements. Other areas of the body can also show signs of TD like nodding and rocking, repeated body movements like crossing and uncrossing arms and legs, and random vocalizations.
Those who experience these involuntary movements may not even realize it. Like other conditions, these stereotypies can get worse under stress. They can manifest as muscle contractions or spasms, inability to be still, facial tics, or other jerking and abnormal movements.