How Is Parkinsons Disease Dementia Diagnosed
No single test can diagnose Parkinsons disease dementia. Instead, doctors rely on a series or combination of tests and indicators.
Your neurologist will likely diagnose you with Parkinsons and then track your progression. They may monitor you for signs of dementia. As you get older, your risk for Parkinsons dementia increases.
Your doctor is more likely to conduct regular testing to monitor your cognitive functions, memory recall, and mental health.
What Are Parkinson’s Disease Dementia Medical Treatment And Medications
There is no specific therapy for dementia in Parkinson’s disease. Although cognitive symptoms initially may appear to respond to drugs that promote dopamine production, the improvement is mild and transient in contrast to the early responses to motor control improvement with medication in patients with Parkinson’s disease.
Parkinson’s disease dementia medications
Various medications are used to treat the movement disorders of Parkinson’s disease, some may exacerbate symptoms related to dementia.
- These include dopamine given in the form of levodopa medications known as dopamine agonists that act on the dopamine receptor and medications that slow down the metabolism of dopamine. They are often used in conjunction with monoamine oxidase inhibitors such as rasagiline. In addition, anticholinergic drugs are sometimes used.
- Unfortunately, these drugs may affect cognitive symptoms and mood disorders.
- The anticholinergic drugs, for example, help balance levels of dopamine and acetylcholine, another neurotransmitter, in the brain. These drugs can improve movement disorders but often make memory loss worse.
The dementia of Parkinson’s disease may respond to drugs used in patients with Alzheimer’s disease. However, these drugs, called cholinesterase inhibitors , lead to only small and temporary improvements in cognition.
Mood disorders and psychoses are usually treated with other medication.
Parkinson’s Disease Dementia Surgery And Gene Therapy
- Great strides have been made in the surgical treatment of Parkinson’s disease. Several different procedures are now available, and they are successful in many patients in relieving movement symptoms. Unfortunately, surgery has no effect on cognitive symptoms. In fact, most people with dementia are not candidates for surgery.
- Gene therapy is in its infancy there are ongoing human and animal trials with various methods to insert genes into neuronal cells to reduce or stop Parkinson’s disease symptoms by causing cells to produce dopamine coded by the newly inserted genes. Early results with the treatment termed ProSavin are encouraging. However, it is not clear if such therapy could prevent or reverse Parkinson’s disease dementia.
Read Also: Moringa And Parkinson’s Disease
Who Gets Parkinson’s Disease Dementia
No two cases of Parkinson’s are exactly alike, so it’s hard to say for sure who will develop Parkinson’s disease dementia and who will not. However, researchers have identified several factors that may increase a person’s risk for Parkinson’s disease dementia, including:
- Older age, especially at the time Parkinson’s symptoms began
- Being a man
- Advancing to late-stage Parkinson’s disease
- Experiencing visual hallucinations
What Is Parkinsons Disease
Parkinsons disease is a progressive brain disorder that affects mobility and mental ability. If you or a loved one has been diagnosed with Parkinsons, you may be wondering about life expectancy.
According to some research, on average, people with Parkinsons can expect to live almost as long as those who dont have the condition.
Don’t Miss: How Young Can Parkinson’s Start
Parkinsons Disease Life Expectancy
Most people with Parkinsons can have a normalor close to normallife expectancy today, thanks to new medications, therapies, and other treatments. Survival rates for those with typical Parkinsons disease are either the same as for the general population or shortened by about a year, studies show.
Risk factors for earlier mortality with Parkinsons include:
-
Being diagnosed before age 70
-
Having early in the disease
-
Developing Parkinsons
People with Parkinsons dont die from the disease itself, but from associated complications, such as infections or injuries . Cardiovascular disease is another common cause of death.
Treatments and lifestyle improvements, can help forestall cognitive decline, lower your risk of falls and strengthen your cardiovascular system. These can help improve your quality of life and, by slowing progression of the illness, potentially keep you living longer.
Researchers are continuing to explore new treatments that they hope will one day lead to better therapies for Parkinsons, which will result in an improved prognosis.
Stages Of Parkinsons Disease
Experts have identified a general Parkinsons progression and created a set of Parkinsons stages, which can help determine where you are at in the disease and what your prognosis might be. However, not everybody progresses through Parkinsons disease in the same way or on the same time frame. Some people skip stages or rapidly progress to later stages. Others live for many years with mild or moderate Parkinsons and never reach the more advanced stage of the illness.
Here are five commonly recognized stages of Parkinsons, including what symptoms you might expect. Treatment also can occur during these stages to help prevent or delay later stages of the illness. This can include medication, , and lifestyle changes, such as a healthy diet and exercise program.
You May Like: Games For Parkinson’s Patients
What Are The Symptoms Of Parkinson’s Disease Dementia
Cognitive impairment in Parkinson’s disease may range from a single isolated symptom to severe dementia.
- The appearance of a single cognitive symptom does not mean that dementia will develop.
- Cognitive symptoms in Parkinson’s disease usually appear years after physical symptoms are noted.
- Cognitive symptoms early in the disease suggest dementia with Parkinsonian features, a somewhat different condition.
Cognitive symptoms in Parkinson’s disease include the following:
- Loss of decision-making ability
- Loss of short- and long-term memory
- Difficulty putting a sequence of events in correct order
- Problems using complex language and comprehending others’ complex language
Persons with Parkinson’s disease, with or without dementia, may often respond slowly to questions and requests. They may become dependent, fearful, indecisive, and passive. As the disease progresses, many people with Parkinson’s disease may become increasingly dependent on spouses or caregivers.
Major mental disorders are common in Parkinson’s disease. Two or more of these may appear together in the same person.
The combination of depression, dementia, and Parkinson’s disease usually means a faster cognitive decline and more severe disability. Hallucinations, delusions, agitation, and manic states can occur as adverse effects of drug treatment of Parkinson’s disease, this might complicate the diagnosis of Parkinson’s dementia.
What Is Parkinson’s Disease Dementia
Parkinson’s disease is an age-related degenerative disorder of certain brain cells. It mainly affects movements of the body, but other problems, including dementia, may occur. It is not considered a hereditary disease, although a genetic link has been identified in a small number of families.
- The most common symptoms of Parkinson’s disease are tremor of the hands, arms, jaw, and face rigidity of the trunk and limbs slowness of movement and loss of balance and coordination.
- Other symptoms include shuffling, speaking difficulties, , facial masking , swallowing problems, and stooped posture.
- The symptoms worsen gradually over years.
Depression, anxiety, personality and behavior changes, sleep disturbances, and sexual problems are commonly associated with Parkinson’s disease. In many cases, Parkinson’s disease does not affect a person’s ability to think, reason, learn, or remember .
About 500,000 people in the United States have Parkinson’s disease, and about 50,000 new cases are diagnosed each year. The number of those who have some cognitive symptoms is difficult to pinpoint because accurate data are lacking for the following reasons:
Most people have the first symptoms of Parkinson’s disease after the age of 60 years, but Parkinson’s disease also affects younger people. Early-onset Parkinson’s disease strikes people around the age of 40 years, or even earlier.
You May Like: Can Essential Tremor Become Parkinson’s
Parkinsons Disease: Symptoms Stages And Treatment
Parkinson’s disease usually begins after age 60, gradually progressing over the years. Some people can have early-onset Parkinson’s disease, starting in their 30s or 40s. It is primarily a movement disorder characterized by resting tremors and slowness and stiffness of movement.
In the late stages of the disease, Parkinson’s dementia can develop. But most people who have Parkinson’s disease do not develop dementia as a part of the condition.
Hereditary Forms Of Parkinson’s Disease And Their Clinical Features
A small but significant number of PD patients have a family history compatible with Mendelian autosomal inheritance , either dominant or recessive. Many of these are classified as young-onset or juvenile-onset PD . A number of levodopa-responsive parkinsonian syndromes have been described and linked to a specific locus or gene in the last few years, and some of them have been classified as PARK syndromes . Some of these denote true PD, whereas others represent more complex phenotypes and dissimilar diseases. Only the former group will be briefly approached here, as the clinical phenotype may be a useful pointer for the diagnosis in daily practice, guiding subsequent molecular testing. For more details on the genetics of PD please refer to .
Autosomal-dominant PD:
PARK1/PARK4 : Mean age at onset of symptoms is in the 30s or 40s . Progression appears to be faster than in sporadic PD and dementia is a frequent finding at times the clinical picture resembles DLB, but mean age at onset is much lower than in sporadic cases . PARK1 and PARK4 are attributable to SNCA mutations and duplications/triplications, respectively.
PARK3 : Researchers described a group of families with parkinsonism closely resembling that of sporadic PD, including age of onset the locus has been mapped to 2p13. Penetrance was estimated to be below 40% . It has not been clearly defined whether this represents a disease susceptibility locus or a true Mendelian form of PD.
Autosomal recessive PD:
Read Also: Asbestos And Parkinson’s Disease
What Causes Parkinson’s Disease Dementia
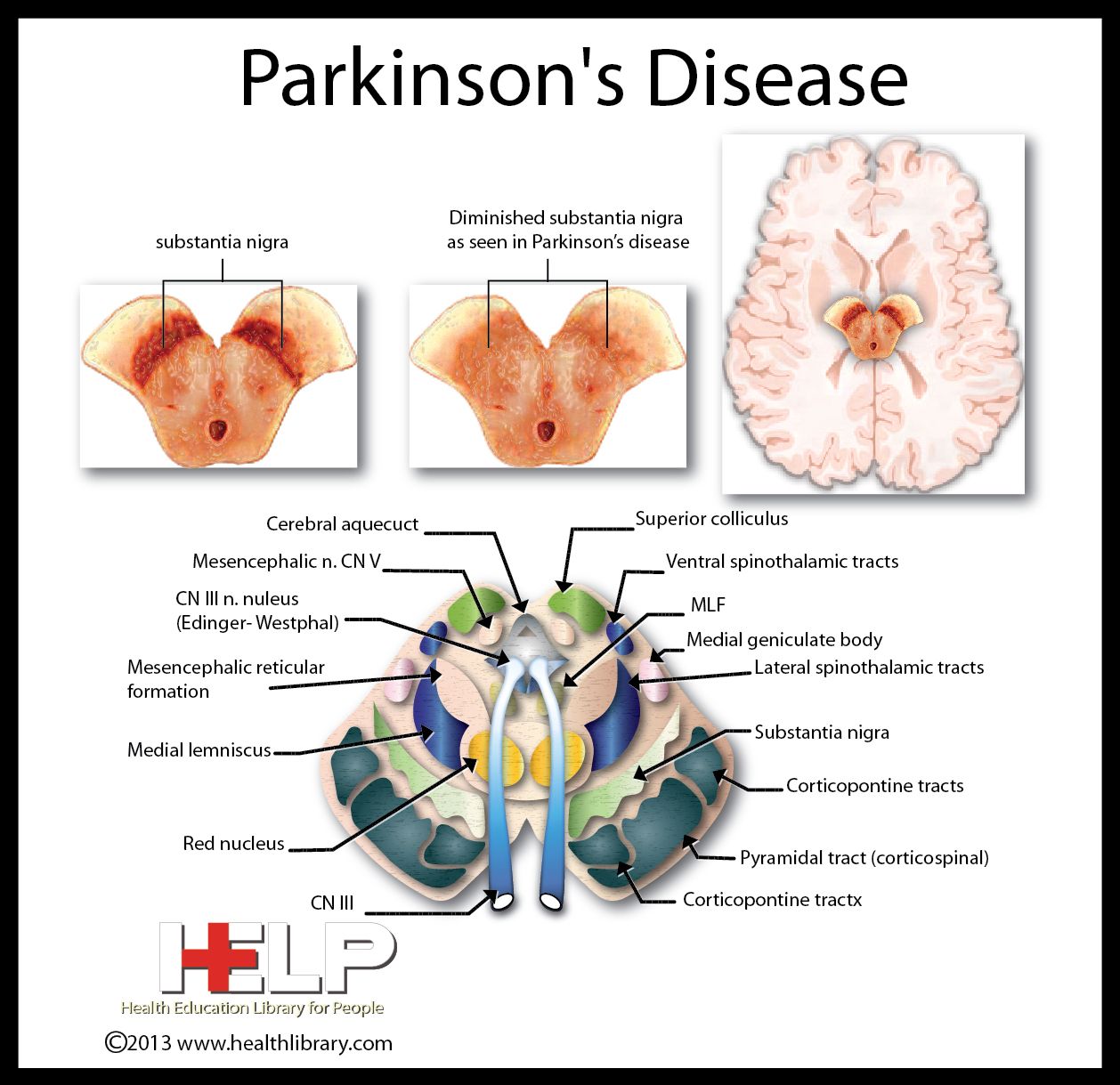
Doctors don’t yet know the exact cause of Parkinson’s disease dementia, but they think it has to do with an accumulation of a protein called alpha-synuclein. When it builds up in the brain, it can create clumps called “Lewy bodies” in nerve cells, causing them to die.
The death of those cells usually results in the motor symptoms typically associated with Parkinson’s disease. As Parkinson’s disease progresses, those Lewy bodies may eventually damage the brain and cause problems with memory and thinking.
While many people with Parkinson’s disease experience cognitive changes, not all of them will go on to develop dementia. It’s estimated that between 50% and 80% of individuals with the disease eventually develop Parkinson’s disease dementia, usually in the later stages of the disease.
Core Features Of Probable Pdd
The primary defining feature of PDD is dementia that develops in the setting of established PD . Therefore, the critical first step in the diagnosis process is to identify idiopathic PD, prior to the development of dementia. For a diagnosis of PDD, two core features must be present: a diagnosis of PD according to the Queen Square Brain Bank criteria and PD developed prior to the onset of dementia .
In this case, a dementia syndrome is defined as impairment in at least two cognitive domains and cognitive deficiency severe enough to impair daily life that must be independent of impairment because of PD motor symptoms. The MDS Task Force recommended that the Mini-Mental State Examination may be useful as a screening instrument for identifying cognitive impairment in PDD patients the MMSE is a simple and universally applied scale that can be easily and quickly performed in the clinical setting . An MMSE score of 25 or below is proposed as the cut-off for identifying clinically significant cognitive impairment in this population .
Read Also: Parkinson’s And Physical Therapy
How To Diagnose Pd
The diagnosis of PD is still largely a clinical one, as there is no definitive test able to confirm the diagnosis during life, with the exception of gene testing in a reduced number of cases. PD is a disease combining clinically defined parkinsonism with specific pathological findings, namely, dopaminergic neuron loss in the region of substantia nigra pars compacta, as well as the presence of intraneuronal Lewy bodies , although there are a few notable exceptions to this with regard to the pathological diagnosis. From a practical perspective, the first step for the diagnosis of PD is careful history taking. Thorough questioning of the patient and family should be performed, trying to define which symptoms emerged and their sequence, as well as perceived anatomical involvement. Inquiry about the presence of premotor symptoms including sleep-related REM sleep behavior, loss of smell, and constipation can be helpful if present. Drug intake history, both past and present, especially concerning drugs able to cause parkinsonian symptoms, is paramount. Likewise, possible exposure to environmental toxics should also be searched for . Past and present medical disorders should be systematically recorded. Family history is also an important stage, and should include neurological disorders in other family members, as well as inquiry about ethnic ancestry as monogenic forms of PD are more prevalent in some .
What Is Parkinson Disease
Parkinson disease is a movement disorder. It can cause the muscles to tighten and become rigid This makes it hard to walk and do other daily activities. People with Parkinsons disease also have tremors and may develop cognitive problems, including memory loss and dementia.
Parkinson disease is most common in people who are older than 50. The average age at which it occurs is 60. But some younger people may also get Parkinson disease. When it affects someone younger than age 50, it’s called early-onset Parkinson disease. You may be more likely to get early-onset Parkinson disease if someone in your family has it. The older you are, the greater your risk of developing Parkinson disease. It’s also much more common in men than in women.
Parkinson disease is a chronic and progressive disease. It doesn’t go away and continues to get worse over time.
Don’t Miss: L Tyrosine For Parkinson’s
Parkinson’s Disease Dementia Follow
A person with Parkinson’s disease and dementia requires regular checkups with his or her health care professional.
- These checkups allow the health care professional to see how well treatment is working and make adjustments as necessary.
- They allow detection of new problems of cognition, mood, or behavior that could benefit from treatment.
- These visits also give the family caregiver an opportunity to discuss problems in the individual’s care.
Eventually, the person with Parkinson’s disease and dementia will likely become unable to care for himself or herself or even to make decisions about his or her care if the patient lives long enough with Parkinson’s disease and dementia.
- It is best for the person to discuss future care arrangements with family members as early as possible, so that his or her wishes can be clarified and documented for the future.
- A health care professional can advise patients and caregivers about legal arrangements that should be made to ensure that these wishes are observed.
Parkinson’s disease dementia prevention
There is no known way of preventing dementia in Parkinson’s disease. However, patients with Parkinson’s disease are urged to continue to exercise and live a healthy lifestyle as this may delay or reduce the onset of dementia, although there is no good data to indicate this will occur.
Parkinson’s disease dementia prognosis
Lewy Body Dementia Vs Parkinsons Disease Dementia
Diagnoses of Lewy body dementia include dementia with Lewy bodies and Parkinsons disease dementia. Symptoms in both of these diagnoses can be similar.
Lewy body dementia is a progressive dementia caused by abnormal deposits of a protein called alpha-synuclein in the brain. Lewy bodies are also seen in Parkinsons disease.
The overlap in symptoms between Lewy body dementia and Parkinsons disease dementia include movement symptoms, rigid muscles, and problems with thinking and reasoning.
This seems to indicate that they could be linked to the same abnormalities, though more research is needed to confirm that.
The later stages of Parkinsons disease have more severe symptoms that may require help moving around, around-the-clock care, or a wheelchair. Quality of life can decline rapidly.
Risks of infection, incontinence, pneumonia, falls, insomnia, and choking increase.
Hospice care, memory care, home health aides, social workers, and support counselors can be a help in later stages.
Parkinsons disease itself isnt fatal, but complications can be.
Research has shown a median survival rate of about
Don’t Miss: How Do You Get Parkinson’s
Coping With Alzheimers And Parkinsons Disease
Living with both Alzheimers disease and Parkinsons disease is extremely challenging. The dementia of Alzheimers combined with the movement effects of Parkinsons can make self-care especially difficult.
Rivastigmine is the only medication that is specifically approved for the treatment of Parkinsons dementia. Additionally, you may need medication for the motor symptoms of Parkinsons disease and medication to help with other symptoms, such as dry skin.
What’s The Difference Between Memory Loss And Parkinson’s Dementia
Alzheimer’s dementia and Parkinson’s disease can both affect a person’s memory, but not in the same way.
Generally speaking, Parkinson’s dementia is not associated with the sort of memory loss that comes with Alzheimer’s, the most common form of dementia. Put differently: It doesn’t typically impact a person’s ability to absorb and store new memories or information the way Alzheimer’s does.
“You can learn , but it’s difficult to retrieve the information that you have in your brain,”Irene Litvan, MD, director of the Movement Disorder Center at the University of California, San Diego, tells Health. “You may not know where the cassette is, but if somebody asks you, ‘Where were you when you lost it?’ You can say, ‘Oh, I was there.'”
RELATED: Here’s How a Doctor Explains the Difference Between Alzheimer’s and Dementia
But that’s not to say Parkinson’s disease dementia doesn’t affect memory at all. On the contrary, some people with Parkinson’s dementia do indeed experience short- and long-term memory loss. They might also forget how to perform simple tasks, like how to run the dishwasher. And since Parkinson’s can affect people in different ways, there’s no way to tell whether someone with the disease will experience memory loss related to dementia.
Recommended Reading: How Do They Test For Parkinson’s Disease