Colin Powell Had Been Treated For A Cancer That Severely Impairs The Immune System Lowering Coronavirus Vaccine Effectiveness
Colin L. Powell, the former secretary of state and chairman of the Joint Chiefs of Staff who died Monday of what his family described as complications from covid-19, had been treated for the blood cancer known as multiple myeloma and was due to get a coronavirus booster shot when he suddenly became ill and was hospitalized, his longtime assistant, Peggy Cifrino, said Monday.
Powell, who was 84, received his second Pfizer shot in February but was immunocompromised as a result of his cancer and suffered from Parkinsons disease, Cifrino said in an interview. Multiple myeloma is a blood cancer that severely impairs the immune system, lowering the effectiveness of vaccines.
He was actually scheduled to receive his booster when he fell ill last week, Cifrino said. He couldnt go to his appointment. He thought he was just not feeling quite right, and he went to the hospital.
Cifrino said Powell had been successfully treated for cancer for two or three years.
Obviously it was a factor with his compromised immune system when he got the covid, Cifrino said.
The family and Cifrino, who has worked for Powell for 28 years, did not release details about precisely which treatments doctors employed on Powell in recent days at Walter Reed National Military Medical Center in Bethesda, Md.
The factory of antibodies is not working the way it should in patients under treatment for the disease, Parekh said.
Specialized Immune Cells May Improve Early Detection Of Parkinsons Disease
Jennifer Goldman, 98 MD, MS, professor in the Ken and Ruth Davee Department of Neurology, of Physical Medicine and Rehabilitation, and Section Chief of Parkinsons Disease and Movement Disorders at Shirley Ryan AbilityLab, was a co-author of the study published in Nature Communications.
An elevated presence of specialized immune cells called alpha-synuclein reactive T-cells were found in patients prior to developing motor symptoms and receiving a diagnosis of Parkinsons disease, suggesting that increased reactivity of these cells may be present long before clinical diagnosis, according to a recent study in Nature Communications.
The findings may be used to improve early detection of Parkinsons disease by indicating increased reactivity of the cells prior to the appearance of motor symptoms and clinical diagnosis, as well as help understand the role of the immune system and inflammation in the pathogenesis of the disease.
Early detection of Parkinsons disease, in its prodromal or early clinically symptomatic stages, provides an opportunity to intervene at its earliest stages and potentially affect disease progression or disease symptomatology. These findings may ultimately lead to novel treatments for Parkinsons disease that modulate the immune system, said Jennifer Goldman, 98 MD, MS, professor in the Ken and Ruth Davee Department of Neurology and a co-author of the study.
Tracing The Origin And Progression Of Parkinsons Disease Through The Neuro
Study Rationale: While inflammation of the brain caused by immune cells has been implicated in Parkinsons disease , it is unknown whether these cells attacking the brain initiate the disease. Moreover, there is new evidence that bacteria in the gut may actually trigger the immune system leading to disease initiation via the peripheral nerves that connect the gut with the brain. Our studies will integrate cutting-edge technologies in humans and pre-clinical models to determine whether the disease is mediated by immune cells recognizing alpha-synuclein, a key brain protein implicated in PD.
Hypothesis: We hypothesize that in a subset of cases, PD is initiated by an autoimmune event involving recognition of alpha-synuclein in the gut, and that interactions between the immune system and the peripheral and central nervous systems establish the disease in the brain.
Impact on Diagnosis/Treatment of Parkinsons Disease: This work will reveal fundamental mechanisms that account for the initiation and progression of PD, uncovering disease- and tissue-specific profiles of autoreactive T cells and overall T cell surveillance that will lead to the discover of perturbed immune pathways in PD with potential application in the development of immunomodulatory therapies.
Leadership
Yale University
Project Outcomes
Neuro-immune Interactions | 2020
Don’t Miss: Parkinson’s And Bad Taste In Mouth
Parkinson’s And The Immune System
Medicine
Ruhr-University Bochum
image: Professor J& ouml rg Tatzelt, Professor Konstanze Winklhofer, Nikolas Furthmann and Dr. Verian Bader belong to the team of authors of the publication.view more
The team was thus able to provide further evidence that there are interfaces between the nervous system and immune system. The researchers hope that the protagonists or antagonists of this signalling pathway may be suitable for therapeutic interventions. They report on this in the cover story in the journal Science Signaling on 4 February 2020.
Genes protect nerve cells against cell death
The Parkin gene protects nerve cells against functional impairment and cell death. It particularly ensures that mitochondria, cell organelles that are responsible for energy production, remain intact and that damaged mitochondria are removed. PACRG is located next to the Parkin gene in the genome. Both genes share what is called a promotor, which regulates the expression of the genes. Parkin and PACRG are thus expressed in a similar pattern.
“Little has been known about PACRG so far, so we investigated what functions this gene has,” says Konstanze Winklhofer. Her team found that, unlike Parkin, PACRG has no influence on the elimination of damaged mitochondria, but, like parkin, is able to protect nerve cells from cell death.
Parkin and PACRG regulate a signalling pathway of the innate immune system
Funding
Original publication
Press contact
Scientists Link Immune Cells To Parkinson’s Disease Onset

- Date:
- La Jolla Institute for Immunology
- Summary:
- A new study adds increasing evidence that Parkinson’s disease is partly an autoimmune disease. In fact, the researchers report that signs of autoimmunity can appear in Parkinson’s disease patients years before their official diagnosis.
A new study co-led by scientists at the La Jolla Institute for Immunology adds increasing evidence that Parkinson’s disease is partly an autoimmune disease. In fact, the researchers report that signs of autoimmunity can appear in Parkinson’s disease patients years before their official diagnosis.
The research could make it possible to someday detect Parkinson’s disease before the onset of debilitating motor symptoms — and potentially intervene with therapies to slow the disease progression.
The study, published in the April 20, 2020, issue of Nature Communications, was co-led by LJI professor Alessandro Sette, Dr. Biol. Sci, and Professor David Sulzer, Ph.D., of the Columbia University Medical Center.
Scientists have long known that clumps of a damaged protein called alpha-synuclein build up in the dopamine-producing brain cells of patients with Parkinson’s disease. These clumps eventually lead to cell death, causing motor symptoms and cognitive decline.
The researchers hope to study more Parkinson’s patients and follow them over longer time periods to better understand how T cell reactivity changes as the disease progresses.
Story Source:
Also Check: Is Thumb Twitching A Sign Of Parkinson’s
An Interplay Between Stress And Immune System
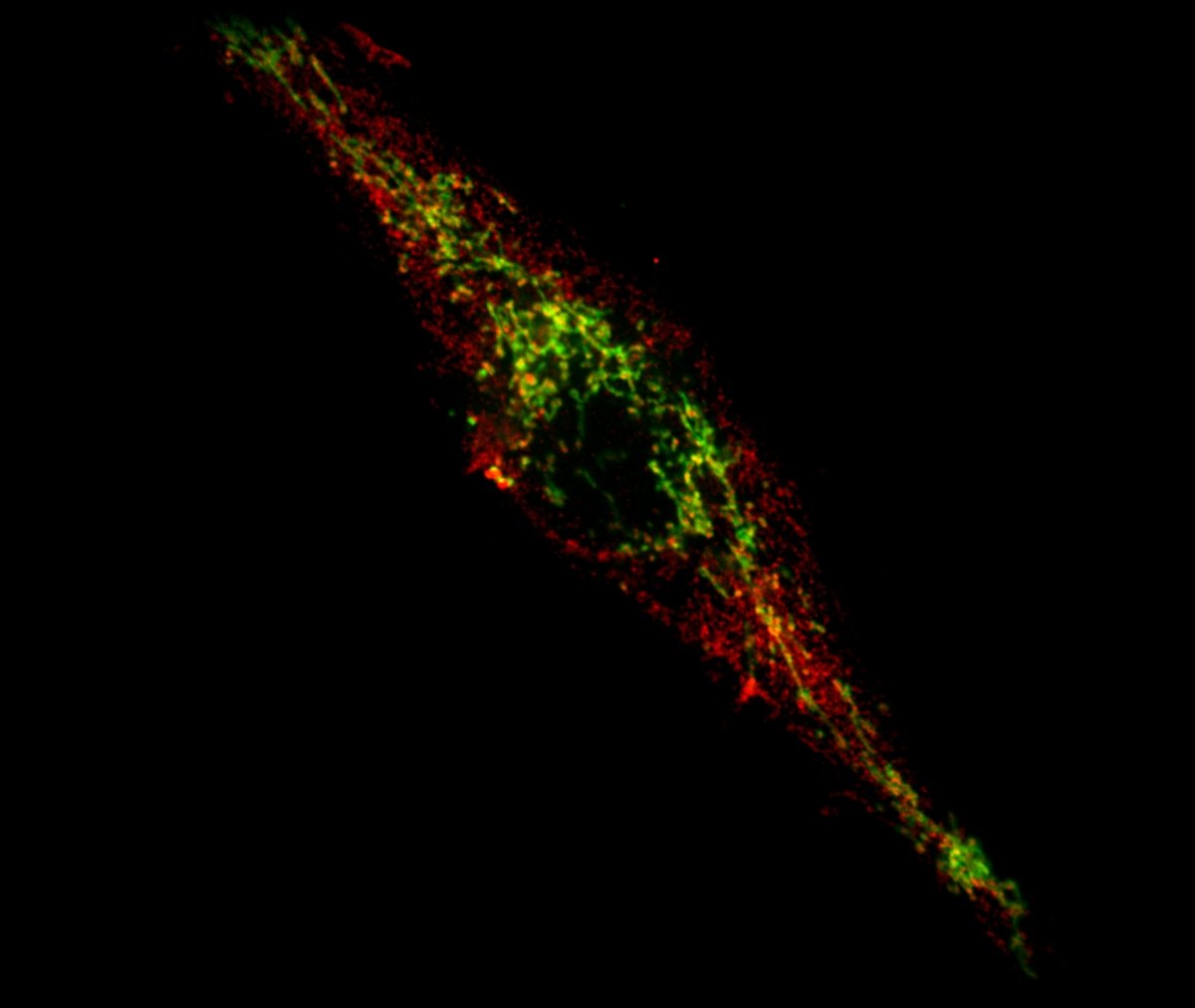
Connection between immune and stress responses. The immune system and the stress response are linked through various players, such as interleukins, cytokines, and various hormones. This link between these systems can be important in the pathophysiology of several diseases, such as AD. Created with BioRender.com.
Another important mediator in the response to stress is the ATP/P2X7R-NLRP3 inflammasome pathway, sensed by the innate immune system. Recently, it was reported that administration of antagonists of P2X7 receptors blocked the release of stress-induced cytokines through this cascade, reducing the inflammatory response and being an interesting treatment approach for stress-related disorders such as MDD . Furthermore, in the gene coding this receptor, a single nucleotide polymorphism was associated with an increased risk of depression . In another study, when depressive behaviors in mice were reversed, colony-stimulating factor 1 reversed dystrophy in microglia in the hippocampal area, demonstrating the role between microglial functional changes and depression-like behaviors .
The connection between stress and immune functions makes this an interesting subject of research, important for future studies to gain a better understanding and, thus, new advances in medicine .
From Cancer Associations To Altered Immunity In The Pathogenesis Of Parkinsons Disease
Study Rationale: Parkinsons disease is characterized by premature death of dopamine-producing neurons in the brain cancer is characterized by overgrowth of dividing cells. Despite being very different, Parkinsons disease and cancer both have immune dysfunctions. Cancer occurs when the immune system fails to safeguard, and immune therapy holds new hope for cancer treatment. Parkinsons disease has also been related to immune dysregulation. Moreover, Parkinsons disease and cancer can in fact be caused by the same gene alterations. Two genes, LRRK2 and Parkin, are among such genes.
Hypothesis: We bring together a team of experts in the fields of Parkinsons disease and cancer to borrow sophisticated approaches from cancer research to collaboratively test a hypothesis that immune dysregulation is the reason why alterations in LRRK2 and Parkin can cause both Parkinsons disease and cancer, with a focus on Parkinsons disease in this proposed work.
Study Design: We will use dopamine-producing neurons derived from Parkinsons disease patient stem cells, mouse models with genetically modified LRRK2 and Parkin to modulate and characterize their immune signatures in both the periphery and the brain. In addition, we will perform immune profiling in samples from patients with Parkinsons disease or cancer.
Leadership
The University of Houston
Project Outcomes
Neuro-immune Interactions | 2020
Also Check: How Long Does A Person Live With Parkinson’s Disease
Vagus Nerve Gut And Peripheral Inflammation
As a direct consequence of the findings of the PNS degeneration in PD, studies regarding gut-brain axis and microbiota influence in neurodegeneration have been of interest. Interestingly, in the rAAV- -syn rodent model, overexpression of -syn in the SN led to enteric nervous system changes and altered microbiota , while in transgenic -syn PD model the microbiota influenced the neurodegeneration process . Indeed, changes in microbiota have been related to PD , but also to RBD, suggesting that this might be a factor of very early relevance . The influence of microbiota on shaping the immune system has long been known, but this is a novel exciting concept within the PD field . The relevance of the gastrointestinal track has also been investigated in epidemiological studies suggesting that the risk and incidence of PD is lower in those persons that underwent vagotomy or appendectomy earlier in life . Within this context, inflammatory events in the digestive tube seem of high relevance, particularly due to the enrichment of -syn of the myenteric plexus of the appendix and the presence of macrophages with engulfed -syn in the area . This is also supported by the relation of PD with IBD . Inflammation and dysbiosis, will result into a leaky gut wall that may cause immune activation that promotes neurodegeneration .
Peripheral Immunity In Parkinsons Disease: Evidence For Monocyte Involvement And Infiltration
The presence of -syn pathology in the periphery and the peripheral neuropathy in PD supports a more holistic affection of the nervous system in PD . This peripheral -syn pathology occurs early as it is also seen in RBD patients, prodromal PD . Since the antigenicity of -syn is true for both microglia and monocytes an innate immune response is expected to occur both in the brain and periphery, and their cross-talk will shape the integrated immune response in PD . Accordingly we have shown that, in RBD patients, TLR4 expression in blood monocytes directly correlated to the immune brain activation and indirectly to the dopaminergic neurotransmission as shown by PET , therefore supporting an early central and peripheral immune response, and a cross talk between brain and periphery that associates to the neurodegenerative event. However, it is unclear how much of this is exerted from the periphery or through recruitment and infiltration.
Changes in monocyte subpopulations in Parkinsons disease
Functional changes in monocytes in Parkinsons disease: abnormal activation, phagocytosis and proliferation
Read Also: Does David Brooks Have Parkinson’s
T Cells In The Midbrain Of Pd Patients
Perhaps as a result of peripheral inflammation, changes in lymphocyte subtype populations, and BBB breakdown, T cells can infiltrate the affected brain regions of PD patients. First reported by the McGeers in 1988, CD3+ cells, a marker for T cells, were detected within the CNS of PD brains . Brochard et al. showed that both CD4+ and CD8+ T cells, but not B and natural killer cells, infiltrated the SN of PD patients and were present at much far greater levels than in healthy controls. These T cells were located near blood vessels and neuromelanin-containing dopaminergic neurons . The presence of T cells in the region affected in the disease suggests a targeted extravasation, rather than a random consequence of increased BBB permeability by peripheral inflammation. If T cells that had escaped self-tolerance circulate in the blood of PD patients, it is plausible that they could infiltrate into the brain permitted by a leaky BBB. The causal role of infiltrating T cells is further elucidated in studies from mouse models of PD.
Sign Up For The Latest From Science News
Headlines and summaries of the latest Science News articles, delivered to your inbox
Thank you for signing up!
There was a problem signing you up.
Patients with Parkinsons experience tremors and slowed movement, among other symptoms. Scientists dont know exactly what causes Parkinsons, but during the disease, many nerve cells located in a region of the brain called the substantia nigra die. These neurons release dopamine, a chemical messenger that is sent to other parts of the brain to coordinate movement. Little blobs known as Lewy bodies, primarily made of a protein called alpha-synuclein, also build up in these neurons.
One of the immune systems jobs is to distinguish between the bodys own components and foreign substances, such as bacteria and viruses. Certain types of immune cells capture proteins and present them to T cells, which figure out, Is it self? Or is it nonself? Does it come from bacteria, a virus or some kind of invader? Sulzer says. In autoimmune disorders, the immune system makes an error in judgment.
Indeed, the two pieces of alpha-synuclein were essentially recognized as foreign by T cells in Parkinsons patients, Sulzer says. He speculates that the autoimmune response contributes to the progression of the disease, rather than the start, as its triggered by the inability to properly break down alpha-synuclein.
Questions or comments on this article? E-mail us at
A version of this article appears in the issue of Science News.
Recommended Reading: Physical Therapy For Parkinson’s Disease
Thanks For Signing Up
We are proud to have you as a part of our community. To ensure you receive the latest Parkinsons news, research updates and more, please check your email for a message from us. If you do not see our email, it may be in your spam folder. Just mark as not spam and you should receive our emails as expected.
Parkinsons Disease And Autoimmunity
This autoimmune component of PD may only be one piece of a larger puzzle. It has long been suspected that immune alterations are an important part of the development of PD, says Maureen Leehey, MD, professor of neurobiology at the University of Colorado School of Medicine in Aurora, CO. She notes previous research that has linked ibuprofen use in mid-life with lower PD risk. And studies have shown that in the early stages, but not the late stages, there is activation of immune fighting cells in the brains of persons with PD, Dr. Leehey says. I think that immune alterations are an important part of the progression of central nervous system damage in PD.
This isnt the first research being done on Parkinsons and autoimmunity there have been multiple studies in this vein in recent years. In 2017, the same researchers from La Jolla and Columbia University identified a specific protein that drives the T cell response in early Parkinsons disease. Further work has suggested that Parkinsons could be triggered by bacterial infection.
Paredes explains that changes in the gut bacteria population can cause chronic inflammation that might influence Parkinsons symptoms. An April 2020 study in Nature Genetics theorized that Parkinsons may start in the gut, due to evidence that neurons in the gut are directly associated with the onset of disease.
Don’t Miss: Using Cbd For Parkinson’s Disease
Does The Immune System Play A Role In Parkinsons Disease
Member for
HealthCentral
Parkinsons disease is widespread and well-studied, but its origins remain somewhat of an enigma to the medical establishment. Yet, as of now, there is no cure for PD, in part because the root cause is still a mystery, explains James Beck, PhD, Chief Scientific Officer at the Parkinsons Foundation in Miami, FL. We know that 10 to 15% of people who develop PD have a genetic mutation that predisposes them to the disease, but even then, we do not fully understand how their disease starts.
The Connection With Innate Immunity And Antigen Presenting Cells
Microglia are the primary immune cells of the CNS and act as both resident phagocytic and antigen presenting cell to provide an active immune defense . Microgliosis is characterized by microglia proliferation, change in morphological state from ramified to amoebic, and the presence of several inflammatory markers, such as CD68 . Microglial activation is an important potential player in PD-associated inflammation and immune reactivity. Neurons do not express Class II, while microglia are MHC Class II expressing antigen-presenting cells. MHC Class II present peptides derived from extracellular proteins , and cells of the monocyte lineage such as microglia are particularly apt at internalizing aggregated proteins and presenting peptides derived from exogenous proteins in the context of class II MHC molecules. They therefore represent a strong candidate for MHC class II restricted presentation of -syn peptides to T cells.
Recommended Reading: How Does Parkinson’s Disease Kill You
Activation Of Transposable Elements As A Trigger Of Neuroinflammation In Parkinsons Disease
Study Rationale: Inflammation is a common event in Parkinsons disease , but its source remains unclear. There are many candidates that could cause inflammation in the nervous system. One likely candidate involves the activity of transposable elements, which are viral-like gene fragments left over from viral infections. While transposable elements are normally inactive, certain stressors can reactivate these genes, leading to a potential immune response, including inflammation.
Hypothesis: This study will seek to determine whether transposable elements are active in tissues from patients with Parkinsons disease and whether this activity can induce inflammation in the nervous system.
Study Design: We will first look for evidence of transposable element activity using single-cell RNA sequencing of tissues from people with Parkinsons disease. This particular experiment will also allow us to determine whether patient cells that show more transposable element activity also show increased signs of inflammation. Because cells of the central nervous system can be grown in a laboratory culture system, we can also test whether manipulations that induce transposable element activity in these cells also causes an immune response that would result in inflammation. This would suggest that blocking transposon activity could block inflammation.
Leadership
Cambridge University
Project Outcomes
Neuro-immune Interactions | 2020