Why Was This Study Needed
Approximately 127,000 people in the UK have Parkinsons disease, around two people in every 1,000. It mostly affects adults over the age of 50.
Parkinsons disease is a progressive neurological condition that causes increasing disability. People experience, amongst other problems, muscle stiffness, slow movements and tremors.
There is no cure for Parkinsons disease, but treatment can control symptoms. Levodopa is the main drug used to improve movement. It can cause side effects, such as jerky movements, and might become less effective. Therefore, treatment is sometimes delayed to avoid side effects.
Earlier research has suggested that levodopa might slow down the worsening of the disease itself, as well as relieving symptoms. This study aimed to demonstrate whether this was the case and chart the development of any symptoms over almost 18 months.
Treatment Of Late Stage Complications Of Parkinson’s Disease
Postural hypotension
Levodopa and dopamine agonists worsen postural hypotension and it may be necessary to lower the dose of levodopa or withdraw the agonist. Treatment is difficult, but patients should be advised to sleep with the head of the bed raised by one or two bricks and to add salt to their diet. Fludrocortisone can then be added at a dose of 0.1 mg in the morning, increasing if necessary up to 0.5 mg in the morning. If these measures are ineffective, the alpha agonist midodrine 10-20 mg four hourly can be useful but it is experimental and only available via the Special Access Scheme. Patients treated for postural hypotension need to have electrolytes, renal function and supine blood pressures closely monitored.
Parkinsonian psychosis, depression and dementia
Psychotic symptoms such as visual hallucinations and persecutory delusions occur most commonly in the setting of dementia, which may be mild and therefore easily missed. Most drugs for Parkinson’s disease make these symptoms worse. Depression is also common and requires treatment in its own right.
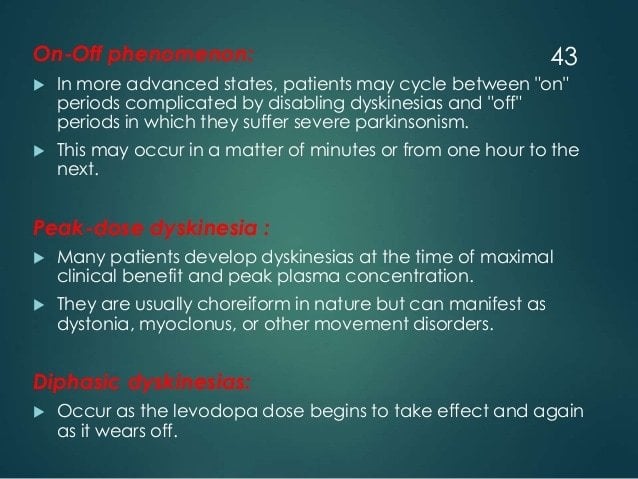
Motor Fluctuations And Dyskinesia
For the treatment of motor features of tremor, bradykinesia, and rigidity associated with Parkinson’s disease, dopaminergic therapies are initially effective however, motor fluctuations eventually complicate therapy and can cause significant disability and impair quality of life. Sustained-release carbidopa/levodopa and bromocriptine have not been found to reduce off time.
Risk factors for motor complications include disease severity, younger age at onset of Parkinson’s disease, high levodopa dosage, and longer disease duration. The motor fluctuations usually are addressed with levodopa adjustments as well as adjunctive medications or surgery as discussed below.
You May Like: Parkinson’s Disease And Cbd
Parkinsons Treatment For Motor Symptoms
The majority of medications developed specifically to treat Parkinsons disease target common motor symptoms. Many of these treatments are designed to increase the level of the dopamine, a neurotransmitter that transfers signals between nerve cells. Dopamine is involved in regulating signals for movement, which is reduced in the brains of Parkinsons disease patients.
Symptomatic And Neuroprotective Therapy
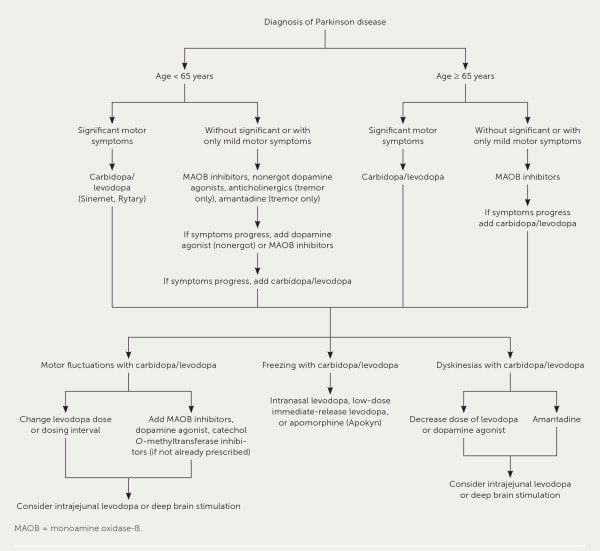
Pharmacologic treatment of Parkinson disease can be divided into symptomatic and neuroprotective therapy. At this time, there is no proven neuroprotective or disease-modifying therapy.
Levodopa, coupled with carbidopa, a peripheral decarboxylase inhibitor , remains the gold standard of symptomatic treatment for Parkinson disease. Carbidopa inhibits the decarboxylation of levodopa to dopamine in the systemic circulation, allowing for greater levodopa distribution into the central nervous system. Levodopa provides the greatest antiparkinsonian benefit for motor signs and symptoms, with the fewest adverse effects in the short term however, its long-term use is associated with the development of motor fluctuations and dyskinesias. Once fluctuations and dyskinesias become problematic, they are difficult to resolve.
Monoamine oxidase -B inhibitors can be considered for initial treatment of early disease. These drugs provide mild symptomatic benefit, have excellent adverse effect profiles, and, according to a Cochrane review, have improved long-term outcomes in quality-of-life indicators by 20-25%.
Neuroprotective therapy aims to slow, block, or reverse disease progression such therapies are defined as those that slow underlying loss of dopamine neurons. Although no therapy has been proven to be neuroprotective, there remains interest in the long-term effects of MAO-B inhibitors. Other agents currently under investigation include creatine and isradipine.
Also Check: Interventions For Parkinson’s Disease
What Are The Implications
According to this research, levodopa is unlikely to affect the progression of Parkinsons disease in the first year and a half following diagnosis.
Symptoms had improved to the same extent by 80 weeks and side effects were similar, suggesting people can start treatment as early as they need to for symptomatic relief.
This supports current practice in giving levodopa when clinically needed. There is no cure for Parkinsons disease, and further research is in progress to develop disease-modifying agents.
Whats The Difference Between Vascular Parkinsonism And Parkinsons
As the name implies, vascular parkinsonism is caused by cerebrovascular disease which affects the blood supply to the brain. Vascular parkinsonism is caused by one or more small strokes, while Parkinsons is caused by a gradual loss of nerve cells. One major difference from Parkinsons is that its not progressive, while Parkinsons becomes worse with time. Another difference is that there are no tremors in vascular parkinsonism.
For more information on vascular parkinsonism, read this journal article.
Read Also: Parkinson’s Disease And Essential Tremor
Treatment Of Neurobehavioral Features
Treatment of cognitive deficits associated with PD is as challenging as the treatment of Alzheimers disease and other dementias. While the general assumption has been that cognitive deficits are a feature of late-stage PD, clinically inapparent cognitive changes on neuropsychiatric testing may be found . With the introduction of cholinesterase inhibitors such as donepezil , rivastigmine , and galantamine and the NDMA antagonist memantine , it is possible that cognition, orientation and language function will improve, and that such improvement will lead to a meaningful improvement in function. Both donepezil and rivastigmine improve cognition to the same effect, but donepezil is better tolerated . The largest and best-designed study of rivastigmine in dementia associated with PD involved 541 patients enrolled in a 24-week randomized, multicenter, double-blind clinical trial . The patients had a relatively mild dementia , with onset of dementia about 2 years after onset of PD symptoms. The mean ADAS-cog score, the primary efficacy variable, improved by 2.1 points in the rivastigmine group, compared to 0.7 in the placebo group , and the MMSE improved by 0.8 in the rivastigmine group and worsened by 0.2 in the placebo group . At the end of the study, 55.5% were receiving 9 to 12 mg. The adverse effects that were significantly more frequent in the rivastigmine group were nausea, vomiting, dizziness, and tremor.
Multiple System Atrophy Formerly Called Shy
As predicted by the name of this parkinsonism, multiple system atrophy affects multiple systems of the body. It affects both the motor skills movement system and the involuntary system of the body. Though the symptoms can often be treated with medications, there is no cure. In addition, there are no drugs that are able to slow the progress of MSA.
Read Also: Cluster Headaches Parkinson’s Disease
Dementia With Lewy Bodies
Of people with dementia, the type of parkinsonism called dementia with Lewy bodies is the second most common cause of dementia, after Alzheimers disease in the elderly. Many are diagnosed at first with Alzheimers disease due to memory or cognitive disorders and then later as dementia with Lewy bodies as the motor symptoms common to Parkinsons progress.
Lewy bodies are abnormal deposits of protein on the nerve cells in the brain. If the production of dopamine, a neurotransmitter, produced by those nerve cells is disrupted due to the buildup of Lewy bodies on those cells, too little dopamine is produced, which can cause the symptoms of Parkinsons.
Family History Tops List Of Risk Factors For Pd
While PD occurs in less than 1% of the population 40 years of age, its prevalence increases with age, becoming significantly higher by age 60 years, with a slight predominance toward males.4
A variety of factors increase the risk of developing PD. A well-conducted meta-analysis showed that the strongest risk factor is having a family member, particularly a first-degree relative, with a history of PD or tremor.5 Repeated head injury, with or without loss of consciousness, is also a factor 5 risk increases with each occurrence.6 Other risk factors include exposure to pesticides, rural living, and exposure to well water.5
Researchers have conducted several studies regarding the effects of elevated cholesterol and hypertension on the risk of PD, but results are still without consensus.5 A study published in 2017 reported a significantly increased risk of PD associated with having hepatitis B or C, but the mechanism for the associationincluding whether it is a consequence of treatmentis unknown.7
You May Like: Parkinson’s And Marriage Breakdown
Motor And Nonmotor Symptoms Of Pd
At its core, PD is characterized by four cardinal symptoms: bradykinesia, rigidity, resting tremor, and postural instability.4 Along with these typical motor symptoms come many nonmotor symptoms with significant associated morbidity and mortality. These include autonomic dysfunction, disorders of sleep and wakefulness, cognitive dysfunction and dementia, mood disorders, and psychosis.5 These nonmotor symptoms of PD are responsible for a significant proportion of hospitalizations, with psychosis reportedly accounting for 24% of hospital admissions in patients with PD.6 This fact signifies the importance of properly managing patients with PD psychosis on both an inpatient and an outpatient basis.6
Whats The Difference Between Corticobasal Degeneration And Parkinsons
The main difference between CBD and Parkinsons is that it usually starts on one side with the gradual loss of use of one hand or leg , and there may be little flicks of involuntary muscle jerks. Walking and balance difficulties usually occur later in CBD than in Parkinsons. Also, in CBD, a person may have trouble with purposeful movements, such as buttoning a shirt or cutting food.
For more information on corticobasal degeneration, read this information page.
Also Check: Can Parkinsons Be Reversed With Exercise
Overview Of Pdp Management
Physical Versus Emotional Control:The intertwining pathophysiology of psychosis and PD through dopaminergic pathways presents healthcare professionals and patients with the unfortunate choice between physical and emotional stability. Dopaminergic agents that treat the symptoms of PD and maintain physical control are predominately associated with the triggering of psychosis symptoms through D2-receptor activation.9,11 This swing to emotional instability could be broadly treated in one of two ways. One option is to stop the anti-PD agent however, this is not feasible for most patients because physical instability and motor symptoms would return. Alternatively, an antipsychotic could be added, but nearly all typical and atypical antipsychotics work via D2-receptor antagonism, potentially tipping the scale toward physical instability. Accordingly, methods used in practice involve dose reduction of offending agents, as tolerated, or the use of an atypical antipsychotic with low D2-receptor affinity.9,11
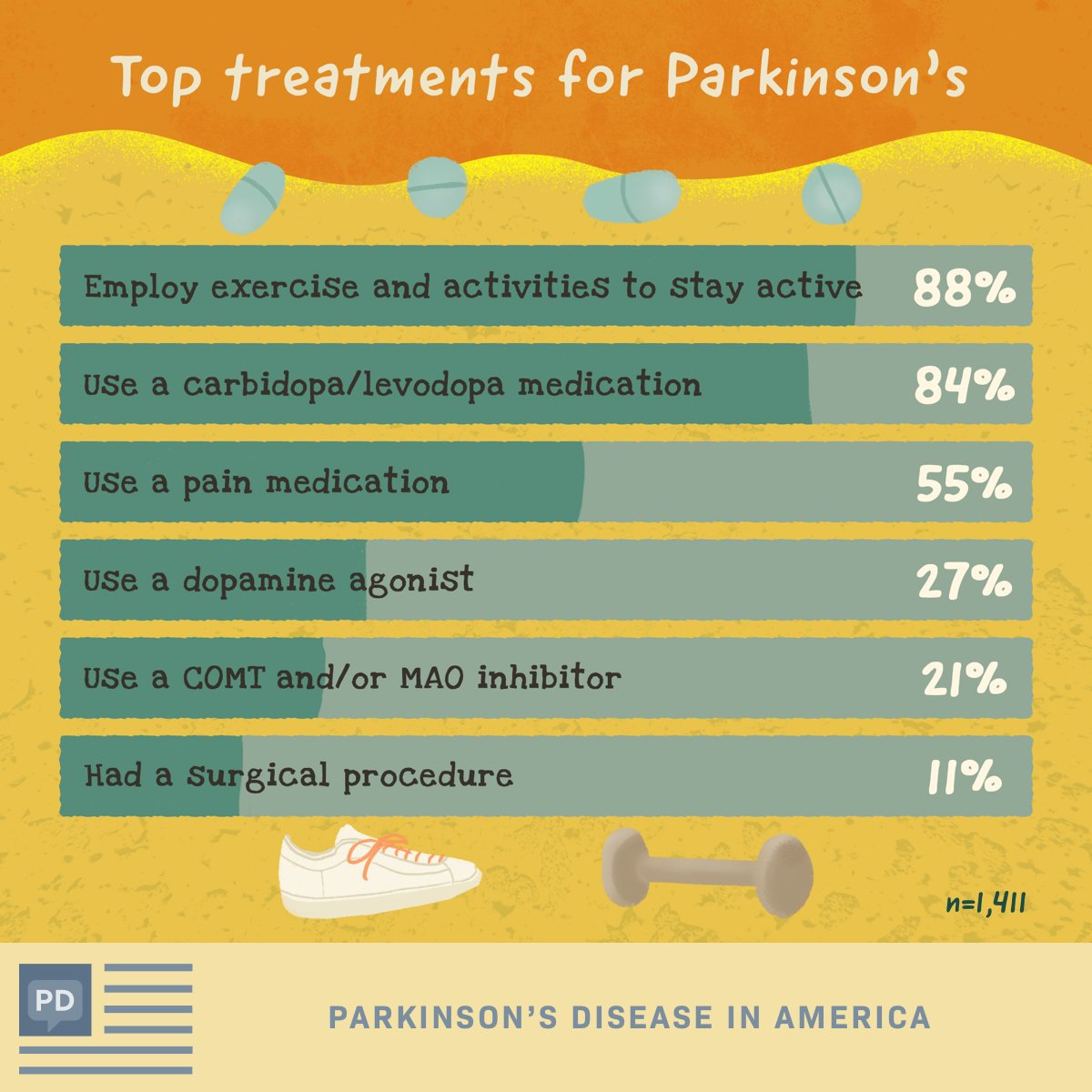
Common Drugs For Parkinson’s Disease
Levodopa and carbidopa . Levodopa is the most commonly prescribed medicine for Parkinsonâs. Itâs also the best at controlling the symptoms of the condition, particularly slow movements and stiff, rigid body parts.
Levodopa works when your brain cells change it into dopamine. Thatâs a chemical the brain uses to send signals that help you move your body. People with Parkinsonâs donât have enough dopamine in their brains to control their movements.
Sinemet is a mix of levodopa and another drug called carbidopa. Carbidopa makes the levodopa work better, so you can take less of it. That prevents many common side effects of levodopa, such as nausea, vomiting, and irregular heart rhythms.
Sinemet has the fewest short-term side effects, compared with other Parkinsonâs medications. But it does raise your odds for some long-term problems, such as involuntary movements. An inhalable powder form of levodopa and the tablet istradefylline have been approved for those experiencing OFF periods, OFF periods can happen when Parkinsonâs symptoms return during periods between scheduled doses of levodopa/carbidopa.
People who take levodopa for 3-5 years may eventually have restlessness, confusion, or unusual movements within a few hours of taking the medicine. Changes in the amount or timing of your dose will usually prevent these side effects.
Dopamine agonists. These drugs act like dopamine in the brain. They include pramipexole , rotigotine , and ropinirole , .
Recommended Reading: Does Weed Help With Parkinson’s
Aan Releases Recommendations On Treatment Of Parkinson’s Disease
Am Fam Physician. 2007 Mar 15 75:922-924.
-
Guideline source: American Academy of Neurology
-
Literature search described? Yes
-
Evidence rating system used? Yes
-
Available at:
Parkinson’s disease is the second most common neurodegenerative disease and is characterized by bradykinesia tremor at rest rigidity and abnormalities of balance, posture, and gait. Its etiology remains unknown in most patients. Recommendations from the Quality Standards Subcommittee of the American Academy of Neurology discuss the following aspects of this condition in a collection of articles in the April 2006 issue of Neurology: diagnosis and prognosis neuroprotective strategies and alternative therapies treatment and evaluation and treatment of depression, psychosis, and dementia in patients with Parkinson’s disease.
Whats The Difference Between Dementia With Lewy Bodies And Parkinsons
In dementia with Lewy bodies, dementia always appears first. There can also be changes in alertness as well as visual hallucinations. However, because of the presence of Lewy bodies throughout the entire brain, characteristics of this disease not only include cognitive characteristics, but also physical, sleep, and behavioral changes. As the disease progresses, the motor symptoms common to Parkinsons such as tremor, slowness, stiffness, and walking and balance problems will appear.
For more information on dementia with Lewy bodies, visit www.lbda.org.
Also Check: Loss Of Balance Parkinson Disease
When Is It Best To Start The Parkinsons Drug Levodopa
Earlier treatment with levodopa provides symptomatic relief to those with symptoms but does not appear to slow Parkinsons disease from progressing. Therefore, timing is best determined by symptoms.
The treatment of Parkinsons disease is complex. Levodopa is the main drug used to reduce tremors and muscle stiffness. Whether it modifies the course of the disease or becomes less effective over time is debated, and it can have side effects, so patients and clinicians sometimes prefer to delay starting treatment.
This Dutch trial involved 445 participants with a recent diagnosis of Parkinsons disease, enrolled over five years. About half took levodopa for 80 weeks, and half placebo for the first 40 weeks and levodopa for the last 40 weeks. There was no difference in symptoms between the groups at the end of the study.
This evidence supports current guidance to start levodopa when symptoms begin to affect the quality of life and confirm that it has insufficient impact on disease progression to justify earlier treatment.
Anticholinergics For Early On
The first pharmacological agents used in PD therapy were anticholinergic drugs. They reduce the activity of acetylcholine by acting as antagonists at choline receptors, hoping to restore the balance between dopamine and acetylcholine levels that was disturbed by PD. These drugs have largely been replaced by L-DOPA and other centrally acting dopaminergic agonists, but they still remain available for use in the treatment of PD. Benztropine, biperiden, diphenhydramine, ethopropazine, orphenadrine, procyclidine, and trihexyphenidyl are included in this therapeutic class of drugs, though there is little pharmacokinetic information available on them because of their low plasma drug concentrations. Typically, anticholinergic drugs have a greater role in tremor-predominant PD and can be a monotherapy in early stages, but are usually done in adjunct with L-DOPA or other prescribed medications.
Also Check: Where Is The Lesion In Parkinson’s Disease
Manual Therapy And Exercise
Chiropractic manipulation, osteopathic manipulation, and Trager therapy have been suggested to benefit patients with Parkinson’s disease. No studies exist, however, to refute or confirm this position. The Alexander technique has shown some benefit and patient improvement has been noted in some studies.
Standard physical therapy, as well as occupational therapy, did result in improved functional outcomes, but the benefit was small and was not sustained when the exercise therapy stopped.
A Review On Parkinsons Disease Treatment
5214526Tori K. Lee Eva L. Yankee
Department of Biology, Angwin, CA 94508, USA .
Received:First Decision:Revised:Accepted:Available online:Academic Editors:Copy Editor:Production Editor:
© The Author 2021. Open Access This article is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, sharing, adaptation, distribution and reproduction in any medium or format, for any purpose, even commercially, as long as you give appropriate credit to the original author and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Recommended Reading: What Benefits Can You Claim For Parkinson’s Disease
The Evolution Of Treatments
The history of Parkinson’s disease is tightly linked to therapeutic interventions, ranging from serendipitous observations to controlled clinical trials of specifically designed agents.
Parkinson devoted a chapter of his monograph to considerations respecting the means of cure . In humility and perhaps with a vision toward current concepts of neuroprotection, he hoped for the identification of a treatment by which the progress of the disease may be stopped . To this end, he advocated very early therapeutic intervention when signs were largely confined to the arms without balance and gait impairments. Reflecting therapeutic approaches of the early nineteenth century, Parkinson recommended venesection, specifically advocating bloodletting from the neck, followed by vesicatories to induce blistering and inflammation of the skin. Small pieces of cork were purposefully inserted into the blisters to cause a sufficient quantity of purulent discharge . All these efforts were designed to divert blood and inflammatory pressure away from the brain and spinal cord, and in this way, decompress the medulla that Parkinson considered the seat of neurological dysfunction.
Medication Guidelines For Parkinson’s Disease
There is no one best mix of Parkinsonâs medicines. You and your doctor will have to try a few treatment approaches to figure out the best one for you.
But there are some general guidelines for taking your medication. Be sure to ask your doctor or pharmacist for any specific tips for your treatment.
Recommended Reading: Young Onset Parkinson’s Symptoms
Basics Of Parkinsons Disease
Parkinsons disease , or paralysis agitans, is a common neurodegenerative condition, which typically develops between the ages of 55 and 65 years. This disease was first named and described by James Parkinson in 1817. The progression of this disease is gradual and prolonged. It has a plausible familial incidence, although the estimates of these occurrences are low and usually sporadic. This disease is organized into two classifications: genetic and sporadic. Genetic PD follows Mendelian inheritance. Sporadic PD, which accounts for about 90% of all Parkinsons cases, is a more complex category in which the pathogenic mechanisms that underlie it are not yet fully understood. Nonetheless, it is known that the byzantine interactions of genetic and environmental influences play roles in the determination of sporadic PD. Several subtypes of PD exist. Each has its own set of causative factors and susceptibilities, pathology, and treatment courses. General risk factors, symptoms, and pathology will be discussed first, before addressing some of the subtypes.