The Importance Of Early Diagnosis
Early detection and diagnosis is important because the treatments for PD are more effective in the early stages of the disease. In addition, physical therapy and exercise, which greatly improve symptoms and delay progression of the disease, are much easier to perform in the early stages.
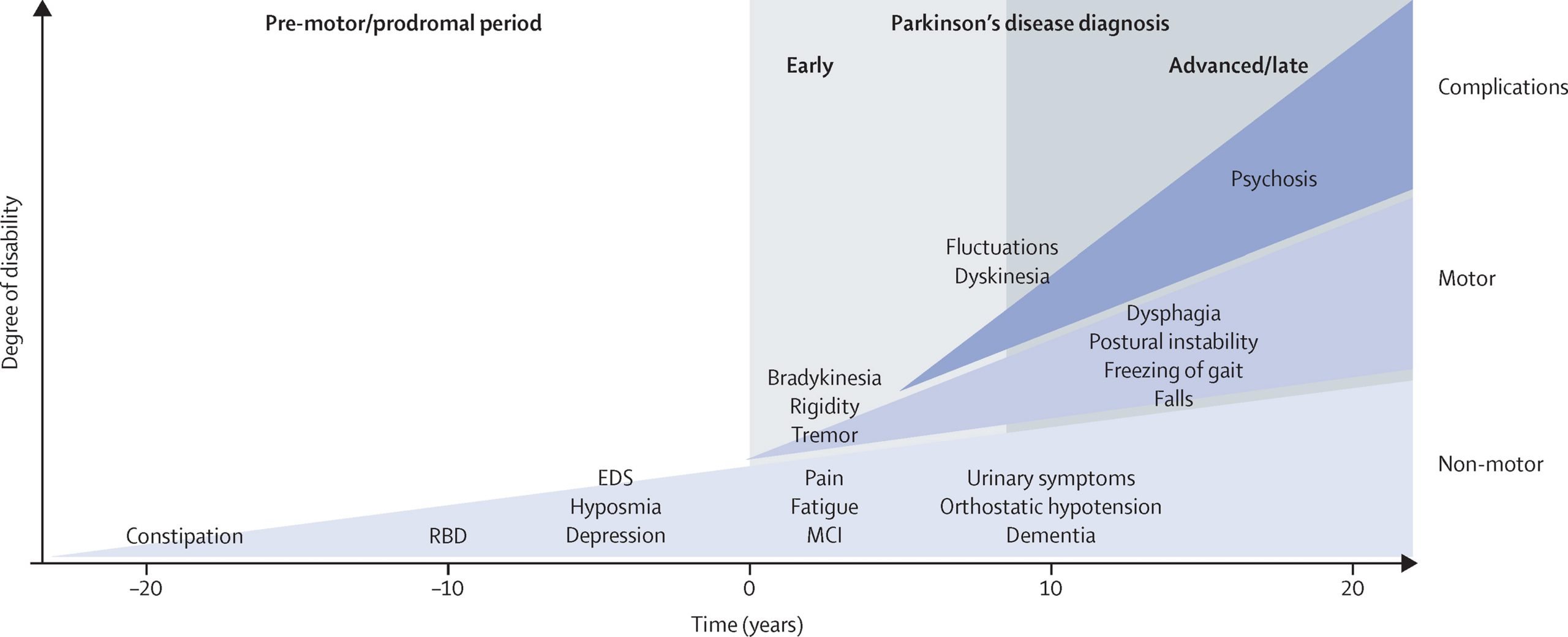
Current diagnosis is made through the presence of motor symptoms however, researchers have found that by the time motor symptoms occur, over 60% of all dopamine neurons in the basal ganglia of the brain have been damaged. Non-motor symptoms become apparent in people with PD long before motor symptoms, including sleep disturbances and loss of the sense of smell.3
Active areas of research include looking for markers in the blood, urine, or cerebral spinal fluid that reliably detect PD, called biomarkers. In addition, brain imaging tests that have high sensitivity for detecting PD are also being actively researched.4
Support For People Living With Parkinsons Disease
While the progression of Parkinsons is usually slow, eventually a persons daily routines may be affected. Activities such as working, taking care of a home, and participating in social activities with friends may become challenging. Experiencing these changes can be difficult, but support groups can help people cope. These groups can provide information, advice, and connections to resources for those living with Parkinsons disease, their families, and caregivers. The organizations listed below can help people find local support groups and other resources in their communities.
Medicines For Parkinsons Disease
Medicines can help treat the symptoms of Parkinsons by:
- Increasing the level of dopamine in the brain
- Having an effect on other brain chemicals, such as neurotransmitters, which transfer information between brain cells
- Helping control non-movement symptoms
The main therapy for Parkinsons is levodopa. Nerve cells use levodopa to make dopamine to replenish the brains dwindling supply. Usually, people take levodopa along with another medication called carbidopa. Carbidopa prevents or reduces some of the side effects of levodopa therapy such as nausea, vomiting, low blood pressure, and restlessness and reduces the amount of levodopa needed to improve symptoms.
People living with Parkinsons disease should never stop taking levodopa without telling their doctor. Suddenly stopping the drug may have serious side effects, like being unable to move or having difficulty breathing.
The doctor may prescribe other medicines to treat Parkinsons symptoms, including:
- Dopamine agonists to stimulate the production of dopamine in the brain
- Enzyme inhibitors to increase the amount of dopamine by slowing down the enzymes that break down dopamine in the brain
- Amantadine to help reduce involuntary movements
- Anticholinergic drugs to reduce tremors and muscle rigidity
Don’t Miss: Anxiety In Parkinson’s Disease
Testing For Parkinsons Disease
There is no lab or imaging test that is recommended or definitive for Parkinsons disease. However, in 2011, the U.S. Food and Drug Administration approved an imaging scan called the DaTscan. This technique allows doctors to see detailed pictures of the brains dopamine system.
A DaTscan involves an injection of a small amount of a radioactive drug and a machine called a single-photon emission computed tomography scanner, similar to an MRI.
The drug binds to dopamine transmitters in the brain, showing where in the brain dopaminergic neurons are.
The results of a DaTscan cant show that you have Parkinsons, but they can help your doctor confirm a diagnosis or rule out a Parkinsons mimic.
How Is It Diagnosed
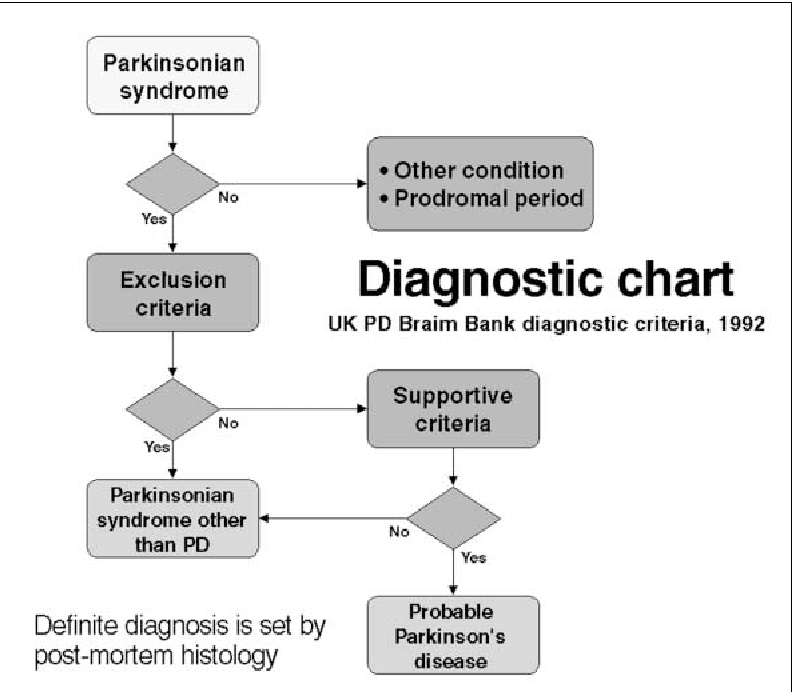
Diagnosing Parkinson’s disease is mostly a clinical process, meaning it relies heavily on a healthcare provider examining your symptoms, asking you questions and reviewing your medical history. Some diagnostic and lab tests are possible, but these are usually needed to rule out other conditions or certain causes. However, most lab tests aren’t necessary unless you don’t respond to treatment for Parkinson’s disease, which can indicate you have another condition.
Also Check: What Happens With Parkinson’s
Documentary To Follow Jeremy Paxman’s Journey Since Parkinson’s Diagnosis
12:24
Jeremy Paxman is working on a documentary that will examine how his recent Parkinson’s disease diagnosis is impacting his life.
Putting Up With Parkinsons will follow the 72-year-old broadcaster and University Challenge host from his formal diagnosis 18 months ago.
He will allow cameras into his life as he looks at how the condition is impacting him and will meet experts leading research into potential treatments.
The one-off, 60-minute special will see Paxman speak to the president of Parkinsons UK, Jane Asher, attend an English National Ballet therapy dance class and learn to play bowls. He will also observe a brain dissection.
Born in Leeds, Paxman started his career in 1972 on the BBCs graduate trainee programme, working in local radio and reporting on the Troubles in Belfast.
Shortly after moving to London in 1977, he transferred from Tonight to investigative flagship programme Panorama, before stints on the Six OClock News and BBC Ones Breakfast Time.
He became a presenter of Newsnight in 1989, a position he would hold until June 2014 during which time he interviewed high-profile figures from politics and culture.
Paxman has also presented University Challenge since 1994, making him the longest-serving current quizmaster on UK TV.
What Are The Symptoms
The best-known symptoms of Parkinson’s disease involve loss of muscle control. However, experts now know that muscle control-related issues aren’t the only possible symptoms of Parkinson’s disease.
Motor-related symptoms
Motor symptoms which means movement-related symptoms of Parkinsons disease include the following:
Additional motor symptoms can include:
- Blinking less often than usual. This is also a symptom of reduced control of facial muscles.
- Cramped or small handwriting. Known as micrographia, this happens because of muscle control problems.
- Drooling. Another symptom that happens because of loss of facial muscle control.
- Mask-like facial expression. Known as hypomimia, this means facial expressions change very little or not at all.
- Trouble swallowing . This happens with reduced throat muscle control. It increases the risk of problems like pneumonia or choking.
- Unusually soft speaking voice . This happens because of reduced muscle control in the throat and chest.
Non-motor symptoms
Several symptoms are possible that aren’t connected to movement and muscle control. In years past, experts believed non-motor symptoms were risk factors for this disease when seen before motor symptoms. However, theres a growing amount of evidence that these symptoms can appear in the earliest stages of the disease. That means these symptoms might be warning signs that start years or even decades before motor symptoms.
Non-motor symptoms include:
Stages of Parkinsons disease
Also Check: Electronic Implant For Parkinson’s
Passive Manipulation Of Limbs
To test for the presence of rigidity, we need to passively manipulate the limbs of the patient. However, If the disease is in its early stage or the symptoms are well controlled with medications, we may not be able to see rigidity. We will need to use some activation maneuvers, that basically consist in performing repetitive movements with the limb contralateral to the one that is being tested.
Also, there are two types of rigidity:
– Lead-pipe rigidity: where the tone is uniformly and smoothly increased throughout the entire range of movement
– Cogwheel rigidity: where a tremor is superimposed on the hypertonia, making the movement irregular due to intermittent increase and reduction of tone
Upper Extremity Testing
For the upper extremity the most sensitive joint where to check for rigidity is the wrist. To uncover rigidity, passively rotate the wrist and feel for a resistance to the movement. It is very important that the arm of the patient is fully relaxed when rotating the wrist. To do this, place your proximal hand under the patients forearm, while your distal hand grabs and rotates the wrist of the patient. When rigidity is present, the range of motion will be preserved but you will feel a resistance in performing the movement.
Wrist rotation with activation maneuver.
It is also possible to test for rigidity in the elbow by passively flexing and extending the forearm.
Elbow flexion-extension with activation maneuver.
Lower Extremity Testing
Ological Limitations Of The Diagnostic Studies
When interpreting the literature about diagnosis, the following methodological issues should be considered:
- lack of long-term prospective clinical and pathological as a reference standard
- lack of operational definitions such as defining specialists or clinical diagnostic criteria
- unclear whether investigators were blinded to initial diagnosis
- sample sizes necessarily limited by the number of cases available with neuropathological outcomes
- trial age groups are often young as studies were performed by neurologists who see a younger population of people with PD
- most studies included people with established disease lasting some years
- varying geographical locations
- some studies are in specialised units and may not reflect the diagnostic accuracy of other units in the UK
- exclusion of some studies using magnetic resonance volumetry and magnetic resonance spectroscopy as they lacked appropriate population, intervention and outcome criteria
- lack of statistical details of diagnostic accuracy such as sensitivity, specificity and positive predictive values
- lack of economic evaluations of SPECT.
Recommended Reading: Neil Diamond Parkinson’s Disease
Fecal Sample Collection And Sequencing
In accordance with our previous study, each participant was asked to collect a fecal sample in the morning using fecal collection containers. The containers were transferred on ice and stored at 80°C prior to processing. The DNA was extracted from 200mg samples using the QIAamp ® Fast DNA Stool Mini Kit following the manufacturers instructions. Microbial composition was determined by 16S rRNA gene sequencing of DNA extracted from stool by amplifying the V3V4 regions. DNA was checked by running the samples on 1.2% agarose gels. Polymerase chain reaction amplification of 16S rRNA genes was performed using general bacterial primers with two-step amplicon library building on the Novaseq platform.
At the same time, we calculated the total bacteria load with 3 replicates by using quantitative real-time PCR. The PCR product of the target microbiota gene was used as a standard control, followed by amplification using the TaKaRa® SYBR PremixTaq kit according to the manufacturers instructions. PCR amplification was performed using the same general primers . The reaction conditions were as follows: pre-denaturation at 95°C for 30s, denaturation at 95°C for 10s, annealing at 55°C for 30s, extension at 72°C for 30s , and final extension at 72°C. Standard curves were set up by serially diluting plasmid of a pMD18-T vector with the appropriate insert from 107 to 1012 target gene copies µl1 for each primer set. The details were described in Supplementary Information.
Definition And Differential Diagnosis
There are many manifestations of but the classical diagnostic symptoms are:
- slowness and poverty of movement
- stiffness
The physical signs of include:
- slowness of movement
- rest tremor.
At diagnosis, these signs are usually unilateral, but they become bilateral as the disease progresses. Later in the disease additional signs may be present including postural instability , cognitive impairment and orthostatic hypotension .
There is no single way to define Parkinsons disease or what is often called idiopathic Parkinsons disease in order to differentiate it from other causes of parkinsonism, such as multiple system atrophy and progressive supranuclear palsy .
is traditionally defined, pathologically, by the finding of Lewy bodies and degeneration of catecholaminergic neurones at post-mortem. Using a pathological definition of PD is problematic for a number of reasons:
- A pathological diagnosis is not practical in life.
- Lewy body inclusions in catecholaminergic neurones are seen in individuals without clinical evidence of it is presumed that these are pre-clinical cases.
- Lewy bodies have not been found in otherwise typical individuals with with Parkin mutations, although such rare young-onset genetic cases of PD might be said not to have idiopathic PD.
In recent years, attempts to define genetically have become possible with the discovery of monogenic forms of the disease. However, such families account for a very small proportion of cases.
Common causes of tremor.
Recommended Reading: Glove For Parkinson’s Tremors
Mri In Parkinson’s Testing
One of the more common tests done during a neurologic workup is an MRI scan and one may think that in the investigation of a disease that affects the brain such as Parkinsons, this imaging test would be a necessity. In the context of Parkinsons disease, however, an MRI is not particularly helpful. It looks at the structure of the brain which, for all intents and purposes, appears normal in this disease. An MRI may, however, be indicated when symptoms appear in younger people or if the clinical picture or the progression of symptoms is not typical for Parkinsons. In these situations, MRI can be used to rule out other disorders such as stroke, tumors, hydrocephalus , and Wilsons Disease .
How Soon After Treatment Will I Feel Better And How Long Will It Take To Recover
The time it takes to recover and see the effects of Parkinson’s disease treatments depends strongly on the type of treatments, the severity of the condition and other factors. Your healthcare provider is the best person to offer more information about what you can expect from treatment. The information they give you can consider any unique factors that might affect what you experience.
You May Like: Probiotics For Parkinson’s Disease
What Is Essential Tremor And How Is It Different To A Parkinsons Tremor
A tremor is a rhythmical, involuntary movement that affects a part of the body, such as the hand.
Essential tremor is the most common type of tremor. Its most noticeable when your hands are doing something and it usually affects both the right and left sides of the body equally. Essential tremors often lessen when your body is resting.
Unlike an essential tremor, a Parkinsons tremor is most obvious when the affected body part is resting and tends to be less noticeable with movement. It usually starts on one side of the body and may progress to the other side as Parkinsons develops.
The time it takes to get a diagnosis can vary from person to person. Some people may receive a diagnosis of Parkinsons quite quickly, but for others it may be a long process. This can be due to a number of things, including your medical history, your age and what symptoms you have.
Your specialist may wish to rule out other causes of your symptoms first and see how you respond to treatment. This may take some time, and, as already mentioned, there is currently no definitive test for Parkinsons.
How you respond to treatment may help your specialist make a diagnosis. Keeping a diary or record of your symptoms will give the specialist more information to guide their decision.
Because the symptoms of Parkinsons are sometimes similar to other forms of parkinsonism, people can sometimes be misdiagnosed.
Looking For Signs Of Parkinsons
Your specialist will examine you to look for common signs of Parkinsons. You may be asked to:
- write or draw to see if your writing is small or gradually fades
- walk to see whether theres a reduction in the natural swing of your arm or in your stride length and speed
- speak to see if your voice is soft or lacks volume
The specialist will also look at and ask you about your:
- face to see if there is a masked look or if you have difficulty with facial expressions
- limbs to see if you have a tremor, any stiffness or slowness of movement
As well as examining you for any of the typical signs of Parkinsons, the specialist will also look for signs that may suggest a different diagnosis.
It may be helpful to take someone with you for support when seeing a specialist. Taking a list of questions you want to ask can also be useful so you dont forget to mention something you want to know about. If a healthcare professional says something you dont understand, dont be afraid to ask them to explain what they mean.
Don’t Miss: Treatment Of Tremor In Parkinson’s Disease
Likelihood Of Referral According To Final Diagnosis
Overall, 74% of all cases with a diagnosis of Parkinson’s disease had been seen by a specialist. However, when these cases were classified by final diagnosis , it was observed that, paradoxically, fewer cases with atypical disease had been seen by a specialist compared with those with classical Parkinson’s disease p = 0.02).
How Is Parkinson’s Disease Managed
Your doctors will tailor your treatment based on your individual circumstances. You will manage your condition best if you have the support of a team, which may include a general practitioner, neurologist, physiotherapist, occupational therapist, psychologist, specialist nurse and dietitian.
While there is no cure for Parkinson’s disease, symptoms can be treated with a combination of the following.
Read Also: Parkinson’s Disease Is The Result Of
Neurodegeneration With Brain Iron Accumulation
Neurodegeneration with brain iron accumulation patients present with a progressive extrapyramidal syndrome associated with iron deposition in the basal ganglia. The two main syndromes are outlined here, although there are additional syndromes including neuroferritinopathy and aceruloplasminemia. The most common of the NBIA disorders is pantothenate kinase-associated neurodegeneration , resulting from mutations on the PANK2 gene, accounting for 50%. The classic syndrome manifests in early childhood with a combination of pyramidal and extrapyramidal features . PKAN can also rarely present in early adulthood. There are typical MRI findings, with a central hyperintensity with surrounding low signal on T2 images in the globus pallidus, giving the so-called eye-of-the-tiger sign .
The second main type of NBIA is PLA2G6-associated neurodegeneration . When onset occurs in infancy, PLAN causes progressive motor and mental retardation with cerebellar ataxia, seizures, and pyramidal signs. However, onset can occur later in life which leads to an atypical syndrome that may mimic PD, with rest tremor, rigidity, and bradykinesia and a good response to levodopa. However, patients also exhibit additional features including eye-movement abnormalities and pyramidal signs .
Who Does It Affect
The risk of developing Parkinsons disease naturally increases with age, and the average age at which it starts is 60 years old. Its slightly more common in men or people designated male at birth than in women or people designated female at birth .
While Parkinsons disease is usually age-related, it can happen in adults as young as 20 .
Also Check: Parkinson’s Disease Education Handout
Molecular Imaging In Parkinson’s Disease
The diagnosis of PD relies on the clinical manifestation of cardinal motor symptoms, bradykinesia, and tremor at rest or rigidity . A positive response to dopaminergic drugs is supportive of the diagnosis. Single photon emission computed tomography or PET ligands that are specific for dopamine transporters indirectly enable the quantification of the deficit of dopaminergic nigrostriatal projections and can provide further support of diagnosis . Deficiencies of monoamine synthesis can be measured with dihydroxyphenylalanine which is a substrate for the enzyme aromatic amino acid decarboxylase in all monoaminergic neurons including noradrenergic neurons .
The role of deficits of noradrenaline in motor and non-motor symptoms is not clear and research on the noradrenergic system in PD patients has been hindered by lack of specific methods to visualize the noradrenergic neurons and projections in vivo. We have recently carried out PET studies to investigate the role of noradrenaline in non-motor symptoms in PD patients and these studies will form the basis of discussions in the paragraphs below.
Paul Johns BSc BM MSc FRCPath, in, 2014