Promoting Physical Activity And Preventing Falls
Because PD is a chronic progressive disorder, it is probable that sustained exercise is necessary to maintain benefits. Indeed, follow-up data from a number of human exercise interventions have demonstrated a gradual return to baseline abilities after the supervised intervention is finished.,,
Because weekly intervention with a physical therapist, throughout the entire course of PD, is neither realistic nor desirable, patients need to take responsibility for their physical activity and exercises. Methods have been developed, based on theories of behavior, for improving exercise habits. Strategies include exploration of the patient’s beliefs about exercise and barriers to regular exercise and discussing the possibility of looking at things differently to change beliefs and overcome barriers. Together, the clinician and patient then establish reasonable goals that the patient thinks are attainable they build on those goals as exercise habits improve. Regular follow-up appointments also are important to monitor progression and provide support to the patient.
What Causes Parkinson’s Disease
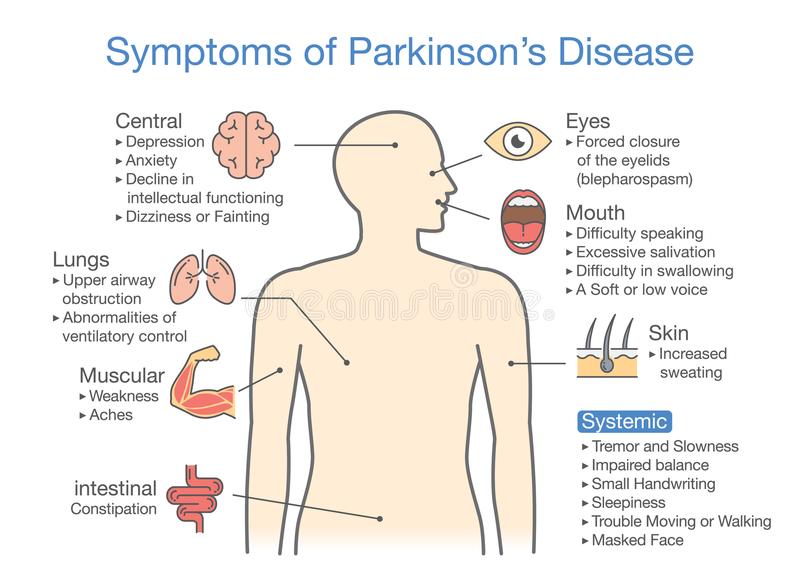
Parkinson’s disease occurs when nerve cells, or neurons, in an area of the brain that controls movement become impaired and/or die. Normally, these neurons produce an important brain chemical known as dopamine. When the neurons die or become impaired, they produce less dopamine, which causes the movement problems of Parkinson’s. Scientists still do not know what causes cells that produce dopamine to die.
People with Parkinson’s also lose the nerve endings that produce norepinephrine, the main chemical messenger of the sympathetic nervous system, which controls many functions of the body, such as heart rate and blood pressure. The loss of norepinephrine might help explain some of the non-movement features of Parkinson’s, such as fatigue, irregular blood pressure, decreased movement of food through the digestive tract, and sudden drop in blood pressure when a person stands up from a sitting or lying-down position.
Many brain cells of people with Parkinson’s contain Lewy bodies, unusual clumps of the protein alpha-synuclein. Scientists are trying to better understand the normal and abnormal functions of alpha-synuclein and its relationship to genetic mutations that impact Parkinsons disease and Lewy body dementia.
How Can People Cope With Parkinson’s Disease
While PD usually progresses slowly, eventually daily routines may be affectedfrom socializing with friends to earning a living and taking care of a home. These changes can be difficult to accept. Support groups can help people cope with the diseases emotional impact. These groups also can provide valuable information, advice, and experience to help people with PD, their families, and their caregivers deal with a wide range of issues, including locating doctors familiar with the disease and coping with physical limitations. A list of national organizations that can help people locate support groups in their communities appears at the end of this information. Individual or family counseling may also help people find ways to cope with PD.
People with PD may also benefit from being proactive and finding out as much as possible about the disease in order to alleviate fear of the unknown and to take a positive role in maintaining their health. Many people with PD continue to work either full- or part-time, although they may need to adjust their schedule and working environment to accommodate their symptoms.
Also Check: Physical Symptoms Of Parkinson’s Disease
Management Of Musculoskeletal Sequelae
Schenkman and Butler were among the first investigators to propose that physical therapy interventions targeting sequelae such as weakness, loss of range, and reduced aerobic capacity could assist some people with PD to improved balance, gait, and function. This concept recognizes that people with PD can develop sequelae to the disorder that might contribute substantially to their difficulty with activities and participation in societal roles. By using physical therapy interventions to reduce the sequelae, it should be possible to improve function despite the primary central nervous system disorder affecting the basal ganglia. Schenkman and colleagues have conducted a number of laboratory experiments designed to test whether improved flexibility, muscle strength , and cardiovascular condition can improve task performance, including gait, postural control, and overall function. Not all of these studies focused on gait specifically. We contend that the findings are of importance because these factors are intimately related to gait. Studies are under way to measure outcomes of gait more specifically.
Whichever approach to exercise is used, to sustain benefits, individuals should continue exercising at least a few times per week as part of their daily routine. They should be reassessed by a physical therapist at least annually in the early stages of the disease and more often in later stages of the disease to progress their exercise program.
What Is Parkinson’s Disease
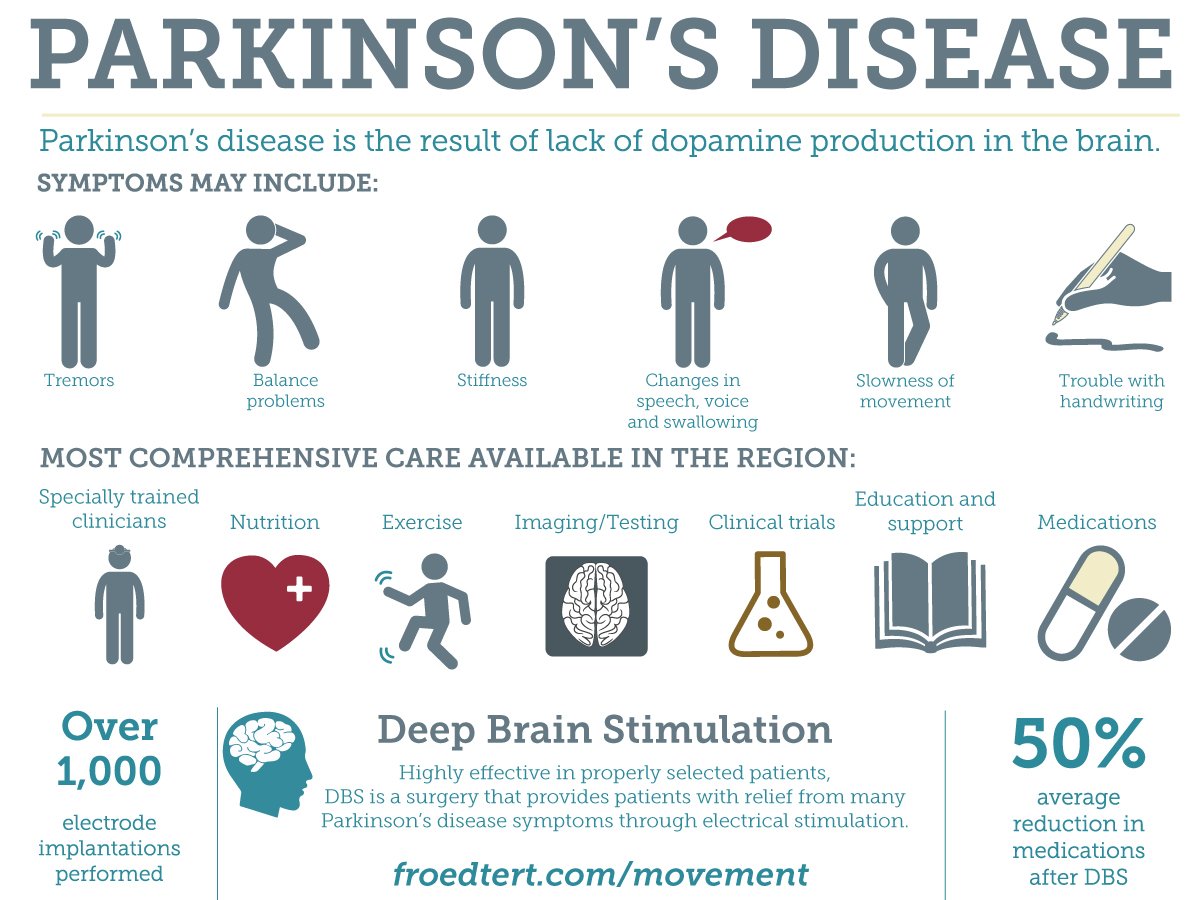
Parkinsons disease is movement disorder of the nervous system that worsens over time. As nerve cells in parts of the brain weaken or are damaged or die, people may begin to notice problems with movement, tremor, stiffness in the limbs or the trunk of the body, or impaired balance. As these symptoms become more obvious, people may have difficulty walking, talking, or completing other simple tasks. Not everyone with one or more of these symptoms has PD, as the symptoms appear in other diseases as well.
No cure for PD exists today, but research is ongoing and medications or surgery can often provide substantial improvement with motor symptoms.
Read Also: Parkinson’s Disease And Vision Problems
Pathogenesis Of Parkinsons Disease
A number of mechanisms have been implicated in PD pathogenesis, with -synuclein aggregation central to the development of the disease. Multiple other processes are thought to be involved, with several studies suggesting that abnormal protein clearance, mitochondrial dysfunction, and neuroinflammation play a role in the onset and progression of PD. However, the relationship between these pathways remains unclear.
Treatments For Parkinson’s Disease And Related Disorders
While there is no known cure for Parkinson’s disease, there are medications and surgical procedures ablation and gamma knife surgeries) designed to improve symptoms. Physical, occupational, and speech therapy may also be beneficial. Our team of physicians and nurse practitioners will work with you to determine which course of disease management is best.
Watch the following segment from Your Fantastic Mind, which focuses on therapies for Parkinsons disease:
Don’t Miss: How Long Does A Parkinson’s Patient Live
Parkinsonism & Related Disorders
Parkinsonism & Related Disorders publishes the results of basic and clinical research contributing to the understanding, diagnosis and treatment of all neurodegenerative syndromes in which Parkinsonism, Essential Tremor or related movement disorders may be a feature.
Regular features will include: Review Articles, Point of View articles, Full-length Articles, Short Communications, Case Reports and Letter to the Editor.
Topics covered will include:
What Are The Symptoms Of The Disease
The four primary symptoms of PD are:
- Tremor. Tremor often begins in a hand, although sometimes a foot or the jaw is affected first. The tremor associated with PD has a characteristic rhythmic back-and-forth motion that may involve the thumb and forefinger and appear as a pill rolling. It is most obvious when the hand is at rest or when a person is under stress. This tremor usually disappears during sleep or improves with a purposeful, intended movement.
- Rigidity. Rigidity , or a resistance to movement, affects most people with PD. The muscles remain constantly tense and contracted so that the person aches or feels stiff. The rigidity becomes obvious when another person tries to move the individuals arm, which will move only in ratchet-like or short, jerky movements known as cogwheel rigidity.
- Bradykinesia. This slowing down of spontaneous and automatic movement is particularly frustrating because it may make simple tasks difficult. The person cannot rapidly perform routine movements. Activities once performed quickly and easilysuch as washing or dressingmay take much longer. There is often a decrease in facial expressions.
- Postural instability. Impaired balance and changes in posture can increase the risk of falls.
Read Also: Can Vyvanse Cause Parkinson’s
Evidence Supporting The Efficacy Of Physical Therapy For Gait Disorders
A previous systematic review of therapies for PD has been published, and Kwakkel et al published a subsequent critical review of the literature on physical therapy for PD. The systematic review produced equivocal results, having been performed at a time when few controlled trials of physical therapy for PD had been published. The review by Kwakkel et al identified 23 randomized controlled trials investigating the effects of physical therapy on function in people with PD. Only 3 of these studies targeted gait disorders.,, An additional 6 studies measured gait- and mobility-related outcomes from programs directed toward improving posture and balance.,, These studies were of moderate methodological quality and demonstrated some benefits of physical therapy for gait and mobility. The interventions tested and outcome measures used varied markedly, making between-study comparisons difficult. Interventions included cueing, mental rehearsal, exercises, and cycling. As suggested by Kwakkel et al, the quality of physical therapy research in PD has improved in the last decade, yet gaps in the evidence base for specific interventions remain.
Autosomal Recessive Juvenile Pd
Some familial forms of PD with autosomal recessive inheritance present very early onset and show both typical and atypical PD symptoms. In 1998, mutations in parkin were identified in Japanese families, and now represent the major cause of young-onset parkinsonism. These patients present with typical motor symptoms and good response to L-dopa, but also slow-course, prominent dystonia, DA neuron loss in the SNc with sporadic LB and absence of non-motor symptoms . These differences suggest a more restricted pathology to the SNc and basal ganglia with minor contribution of -syn pathology.Parkin encodes a widely expressed E3 ubiquitin ligase, a key regulator of protein degradation by the proteasome, suggesting a mechanistic connection with GBA. The FBXO7 gene encodes another E3 ubiquitin ligase implicated in autosomal recessive juvenile PD. Mutations in FBXO7 are less common than those in parkin, disease progresses more rapidly, and symptoms include dementia, dystonia and motor neuron degeneration.
You May Like: Cialis And Parkinson’s Disease
Medicines For Parkinson’s Disease
Medicines prescribed for Parkinson’s include:
- Drugs that increase the level of dopamine in the brain
- Drugs that affect other brain chemicals in the body
- Drugs that help control nonmotor symptoms
The main therapy for Parkinson’s is levodopa, also called L-dopa. Nerve cells use levodopa to make dopamine to replenish the brain’s dwindling supply. Usually, people take levodopa along with another medication called carbidopa. Carbidopa prevents or reduces some of the side effects of levodopa therapysuch as nausea, vomiting, low blood pressure, and restlessnessand reduces the amount of levodopa needed to improve symptoms.
People with Parkinson’s should never stop taking levodopa without telling their doctor. Suddenly stopping the drug may have serious side effects, such as being unable to move or having difficulty breathing.
Other medicines used to treat Parkinsons symptoms include:
- Dopamine agonists to mimic the role of dopamine in the brain
- MAO-B inhibitors to slow down an enzyme that breaks down dopamine in the brain
- COMT inhibitors to help break down dopamine
- Amantadine, an old antiviral drug, to reduce involuntary movements
- Anticholinergic drugs to reduce tremors and muscle rigidity
How Is Parkinsons Disease Diagnosed
There are currently no specific tests that diagnose PD. The diagnosis is based on:
- medical history and a neurological examination
- blood and laboratory tests, to rule out other disorders that may be causing the symptoms
- brain scans to rule out other disorders. However, computed tomography and magnetic resonance imaging brain scans of people with PD usually appear normal.
In rare cases, where people have a clearly inherited form of PD, researchers can test for known gene mutations as a way of determining an individuals risk of developing the disease. However, this genetic testing can have far-reaching implications and people should carefully consider whether they want to know the results of such tests.
Also Check: Parkinson’s Disease And Vision
Clinical History And Testing
Diagnostic tests can be used to establish some features of the condition and distinguish them from symptoms of other conditions. Diagnosis may include taking the person’s , a physical exam, assessment of neurological function, testing to rule out conditions that may cause similar symptoms, brain imaging, to assess cognitive function,, or myocardial scintigraphy. Laboratory testing can rule out other conditions that can cause similar symptoms, such as abnormal , , , or vitamin deficiencies that may cause symptoms similar to dementia.
Dementia screening tests are the and the . For tests of attention, , , and can be used for simple screening, and the Revised Digit Symbol Subtest of the may show defects in attention that are characteristic of DLB. The , and are used for evaluation of executive function, and there are many other screening instruments available.
If DLB is suspected when parkinsonism and dementia are the only presenting features, PET or SPECT imaging may show reduced dopamine transporter activity. A DLB diagnosis may be warranted if other conditions with reduced dopamine transporter uptake can be ruled out.
Since 2001, – has been used diagnostically in East Asia , but not in the United States. MIBG is taken up by nerve endings, such as those that innervate the heart, and is for scintigraphy with radioactive 123iodine. Autonomic dysfunction resulting from damage to nerves in the heart in patients with DLB is associated with lower cardiac uptake of 123I-MIBG.
Parkinsonism With Tau Pathology
The tauopathies with secondary parkinsonism include frontotemporal dementia and AD, in which parkinsonism is a consequence of the late-stage spread of pathology . Although tau pathology is critical in AD, AD seems to be triggered by A oligomers and tau mutations never cause AD. However, tau mutations can cause some forms of the complex FTDs, namely frontotemporal dementia with parkinsonism in chromosome 17. The complex genetics and pathology of FTD will not be discussed in further detail here. These two conditions are placed at the other end of the continuum of the parkinsonian disorders due to their lower overlap with PD .
Interestingly, two tauopathies with parkinsonism are caused by environmental factors . Although no longer prevalent, influenza infections can cause postencephalitic parkinsonism with tau pathology in the SNc. Amyotrophic lateral sclerosis/parkinsonism with dementia complex of Guam is linked to the consumption of the cycad fruit in the Pacific island of Guam. However, the specific toxin responsible for this pathology has not been clearly identified and the disease has almost disappeared in recent years. These environmental links are important because they highlight the high vulnerability of these circuits and may contribute to the identification of the cellular mechanisms triggering these complex pathologies.
You May Like: On Off Phenomenon In Parkinson’s Disease
What Genes Are Linked To Parkinsons Disease
Several genes have been definitively linked to PD:
- SNCA. This gene, which makes the protein alpha-synuclein, was the first gene identified to be associated with Parkinsons. Research findings by the National Institutes of Health and other institutions prompted studies of the role of alpha-synuclein in PD, which led to the discovery that Lewy bodies seen in all cases of PD contain clumps of alpha-synuclein. This discovery revealed the link between hereditary and sporadic forms of the disease.
- LRRK2. Mutations in LRRK2 were originally identified in several English and Basque families as a cause of a late-onset PD. Subsequent studies have identified mutations of this gene in other families with PD as well as in a small percentage of people with apparently sporadic PD. LRRK2 mutations are a major cause of PD in North Africa and the Middle East.
- DJ-1. This gene normally helps regulate gene activity and protect cells from oxidative stress and can cause rare, early forms of PD.
- PRKN . The parkin gene is translated into a protein that normally helps cells break down and recycle proteins.
- PINK1. PINK1 codes for a protein active in mitochondria. Mutations in this gene appear to increase susceptibility to cellular stress. PINK1 has been linked to early forms of PD.
- GBA . Mutations in GBA cause Gaucher disease , but different changes in this gene are associated with an increased risk for Parkinsons disease as well.
Establishing Pd Research Priorities
The NINDS-organized Parkinsons Disease 2014: Advancing Research, Improving Lives conference brought together researchers, clinicians, patients, caregivers, and nonprofit organizations to develop 31 prioritized recommendations for research on PD. These recommendations are being implemented through investigator-initiated grants and several NINDS programs. NINDS and the NIHs National Institute of Environmental Health Sciences held the Parkinsons Disease: Understanding the Environment and Gene Connection workshop to identify priorities for advancing research on environmental contributors to PD.
Research recommendations for Lewy Body Dementia, including Parkinsons disease dementia, were updated during the NIH Alzheimers Disease-Related Dementias Summit 2019 .
Recommended Reading: 1st Sign Of Parkinson’s
What Causes The Disease
The precise cause of PD is unknown, although some cases of PD are hereditary and can be traced to specific genetic mutations. Most cases are sporadicthat is, the disease does not typically run in families. It is thought that PD likely results from a combination of genetics and exposure to one or more unknown environmental factors that trigger the disease.
The protein alpha-synuclein. The affected brain cells of people with PD contain Lewy bodiesdeposits of the protein alpha-synuclein. Researchers do not yet know why Lewy bodies form or what role they play in the disease. Some research suggests that the cells protein disposal system may fail in people with PD, causing proteins to build up to harmful levels and trigger cell death. Additional studies have found evidence that clumps of protein that develop inside brain cells of people with PD may contribute to the death of neurons.
Genetics. Several genetic mutations are associated with PD, including the alpha-synuclein gene, and many more genes have been tentatively linked to the disorder. The same genes and proteins that are altered in inherited cases may also be altered in sporadic cases by environmental toxins or other factors.
Environment. Exposure to certain toxins has caused parkinsonian symptoms in rare circumstances . Other still-unidentified environmental factors may also cause PD in genetically susceptible individuals.