Warning Disclaimer Use For Publication
WARNING: Please DO NOT STOP MEDICATIONS without first consulting a physician since doing so could be hazardous to your health.
DISCLAIMER: All material available on eHealthMe.com is for informational purposes only, and is not a substitute for medical advice, diagnosis, or treatment provided by a qualified healthcare provider. All information is observation-only. Our phase IV clinical studies alone cannot establish cause-effect relationship. Different individuals may respond to medication in different ways. Every effort has been made to ensure that all information is accurate, up-to-date, and complete, but no guarantee is made to that effect. The use of the eHealthMe site and its content is at your own risk.
If you use this eHealthMe study on publication, please acknowledge it with a citation: study title, URL, accessed date.
Parkinson Disease And The Risk Of Epileptic Seizures
Katharina Gruntz MD
Basel Pharmacoepidemiology Unit, Division of Clinical Pharmacy and Epidemiology, Department of Pharmaceutical Sciences, University of Basel, Basel, Switzerland
Basel Pharmacoepidemiology Unit, Division of Clinical Pharmacy and Epidemiology, Department of Pharmaceutical Sciences, University of Basel, Basel, Switzerland
Claudia Becker PhD
Basel Pharmacoepidemiology Unit, Division of Clinical Pharmacy and Epidemiology, Department of Pharmaceutical Sciences, University of Basel, Basel, Switzerland
Boston Collaborative Drug Surveillance Program, Lexington, MA
Boston University School of Public Health, Boston, MA
Basel Pharmacoepidemiology Unit, Division of Clinical Pharmacy and Epidemiology, Department of Pharmaceutical Sciences, University of Basel, Basel, Switzerland
Boston Collaborative Drug Surveillance Program, Lexington, MA
Hospital Pharmacy, University Hospital Basel, Basel, Switzerland
Katharina Gruntz MD
Basel Pharmacoepidemiology Unit, Division of Clinical Pharmacy and Epidemiology, Department of Pharmaceutical Sciences, University of Basel, Basel, Switzerland
Basel Pharmacoepidemiology Unit, Division of Clinical Pharmacy and Epidemiology, Department of Pharmaceutical Sciences, University of Basel, Basel, Switzerland
Claudia Becker PhD
Basel Pharmacoepidemiology Unit, Division of Clinical Pharmacy and Epidemiology, Department of Pharmaceutical Sciences, University of Basel, Basel, Switzerland
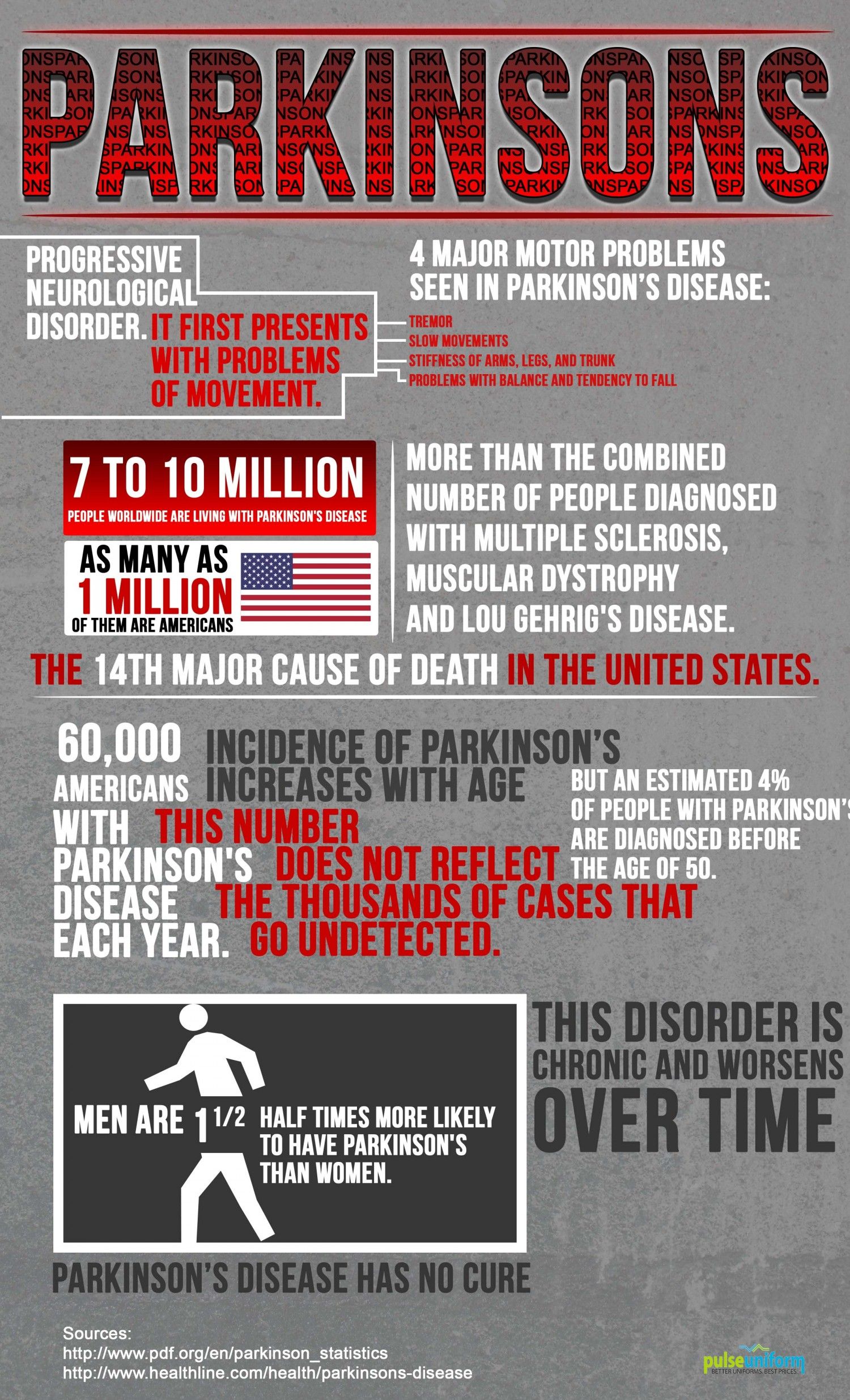
Why Does Parkinsons Occur More In The Elderly
The biggest risk factor for PD is age. While the exact cause remains unknown, scientists believe PD results from a combination of genetic and external factors. It is important to note that many genetic or external factors remain to be discovered and require more scientific research.1
PD affects multiple areas of the body and brain. Death of nerve cells in a brain region called the substantia nigra pars compacta is largely responsible for motor symptoms. These symptoms include tremor, rigidity, and loss of spontaneous movement.
Dopamine is a chemical messenger that transmits signals for producing smooth, purposeful movement. Research has shown that the substantia nigra pars compacta shows more loss of neurons than other areas of the brain. These neurons appear to be more sensitive to some toxins. Many of these toxins target an organelle in neurons called mitochondria which are responsible for generating ATP, the source of energy in a cell.
In addition, during aging, there is a decline in the function of the organelles that clear up and remove damaged proteins in neurons. Also, over time, there is a build up of the alpha-synuclein protein which forms Lewy bodies that damage neurons.
You May Like: Weighted Silverware
How To Manage Symptoms At The End Of Life
At the end of life, good practice is to plan for any potential symptoms that may arise. The most common symptoms anticipated are pain, dyspnoea, nausea and vomiting, agitation, anxiety, delirium and noisy respiratory secretions.18 For patients with PD particular considerations should be given to the more commonly used medicines, specifically anticholinergics and antidopaminergics. These are usually prescribed for treatment of respiratory secretions and nausea and vomiting. Alternatives are available for respiratory secretions, and include glycopyrronium, in preference to hyoscine hydrobromide. Although this is an anticholinergic, only a small proportion crosses the blood brain barrier.
For nausea and vomiting, ondansetron,19 cyclizine, domperidone have all been suggested in PD.20 However, ondansetron has been shown to be inferior to domperidone in the pre-treatment of apomorphine.21 Cyclizine has anticholinergic properties and may exacerbate confusion, especially when comorbid psychosis or cognitive impairment are present. Levomepromazine, although it has antidopaminergic effects, has been shown to be effective for nausea with rotigotine in a case report.22
Agitation, dyspnoea and pain can all be managed with the same anticipatory medications as recommended.20 Specifically relating to PD, several case reports have supported the intraoperative use of midazolam, during sedation, for tremor and dyskinesias,23,24 as well as for agitation at the end of life.20
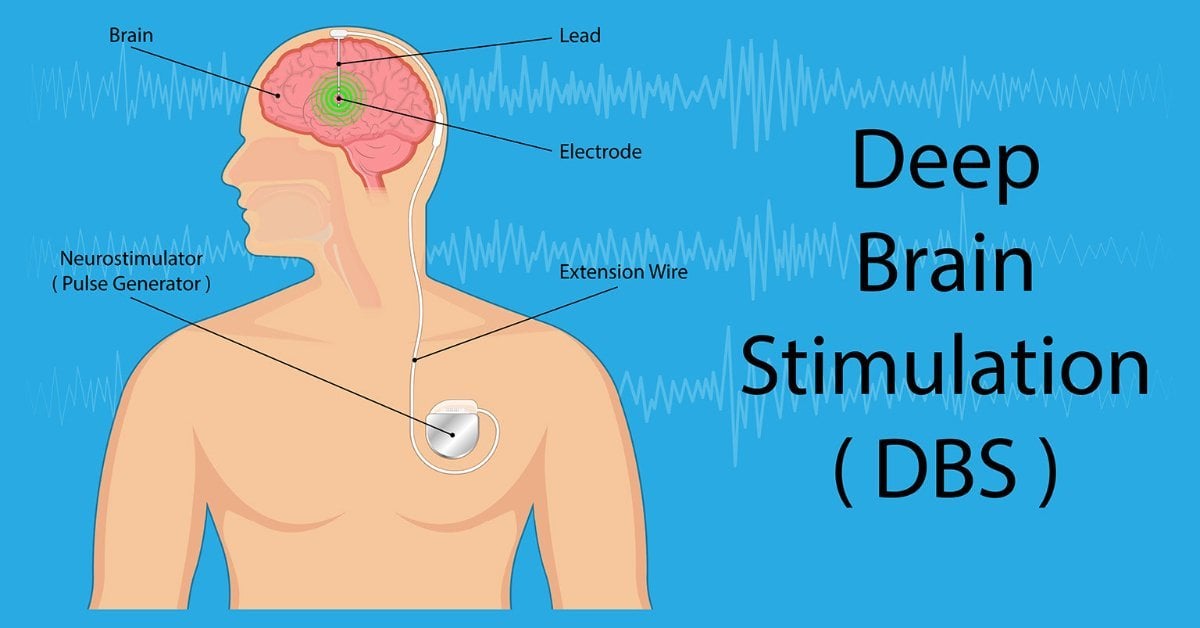
What To Do With Deep Brain Stimulation At The End Of Life
Deep brain stimulation uses an Implantable Pulse Generator, usually placed in the infraclavicular area, connected to leads within the brain. There is a remote programmer, and also a charging unit in the case of a rechargeable device, which are given to the patient and their carer. It improves dyskinesias and also has a levodopa sparing effect.37
Deactivation of DBS may lead to increased symptom burden as mentioned in the section above and so awareness of features of PHS should be considered if there is failure at the end of life. Supportive treatment should be given if possible,38 and anticipation of symptoms of distress from rigidity and fever.
After death, deactivation of the device with the patients handheld programmer is required before removing the pulse generator and battery in the case of a cremation.
Also Check: Cleveland Clinic Parkinson’s Bicycle Study 2017
What Is Parkinsons Disease
Parkinsons disease is a nervous system disease that affects your ability to control movement. The disease usually starts out slowly and worsens over time. If you have Parkinsons disease, you may shake, have muscle stiffness, and have trouble walking and maintaining your balance and coordination. As the disease worsens, you may have trouble talking, sleeping, have mental and memory problems, experience behavioral changes and have other symptoms.
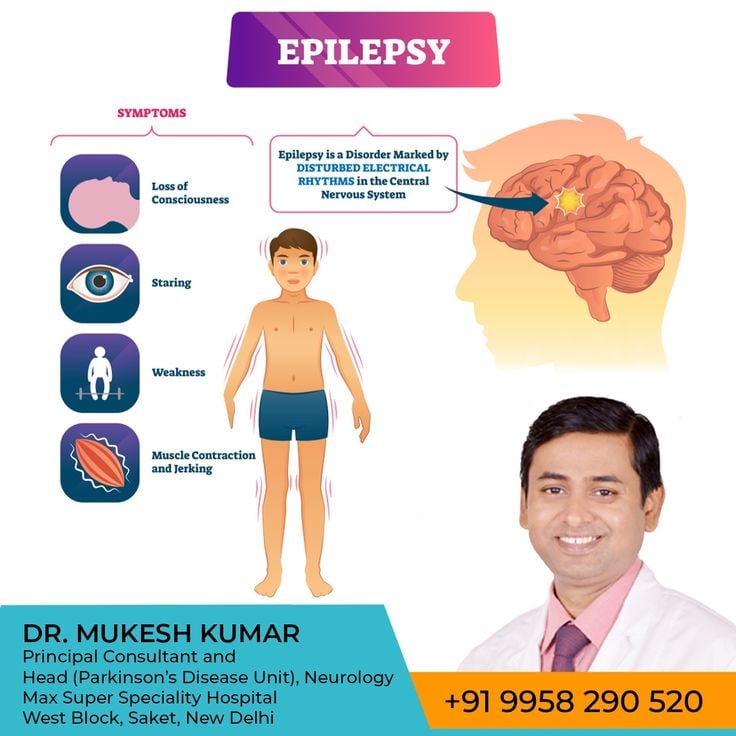
Epilepsy: More Common Than You Think
One in 26. 45,000 people. 160,000 new cases. Your colleague. Your neighbor. Your friend. Your sibling. Your parent. Your spouse. Your child. You.
You may be surprised to learn that one in 26 people will develop epilepsy during their lifetime. In northeastern New York alone, more than 45,000 people are living with epilepsy. And annually, more than 160,000 new cases of epilepsy are diagnosed in the United States.
These statistics often shock people who are unfamiliar with epilepsy. It is far more common than you think. In fact, epilepsy affects more people than muscular dystrophy, multiple sclerosis, cerebral palsy, and Parkinsons COMBINED.
Chances are, someone in your life has been or will be affected by epilepsy.
Along with the talented and experienced neurologists and physicians in our region, the Epilepsy Foundation of Northeastern New York is an invaluable resource for those living with epilepsy and their family members and caregivers. If you or a loved one is affected by epilepsy, the Foundation is here for you. Take a moment to read through the services they provide and call 456-7501 with any questions you may have.
Service Coordination/Case Management
Information and Referral
Recommended Reading: Sam Waterston Tremor
Zonisamide With Levodopa May Reduce Risk Of Dementia Other Parkinsons
The standard treatment for Parkinsons is levodopa and its derivatives, used to replace the dopamine loss seen in patients with the disease. While these medications are generally effective at controlling symptoms, over time they almost always lead to dyskinesia as a side effect. It also is common for people treated with these medicines to experience off time, when their symptoms are not being fully controlled by the therapy.
Zonisamide was originally developed to treat epilepsy, but research has shown it also may be beneficial for people with Parkinsons. In Japan, the therapy is approved to treat Parkinsons and is marketed as Trerief.
Now, researchers at Fukuoka University and from Sumitomo Dainippon Pharma the company that developed zonisamide conducted an analysis of clinical trial data to understand the medications effect on off time and dyskinesia.
The team analyzed data for 212 patients who participated in one of two Japanese clinical trials, in which participants were given either a placebo or zonisamide at doses of 25 or 50 mg per day for 12 weeks, or about three months. The mean patient age was 63.7 and the mean disease duration was just over 11 years. About a third of participants were male. All were being treated with levodopa.
The lower dosage of zonisamide was associated with a slight reduction in off time, but the difference from placebo was not statistically significant.
Neurodegeneration With Brain Iron Accumulation
Neurodegeneration with brain iron accumulation patients present with a progressive extrapyramidal syndrome associated with iron deposition in the basal ganglia. The two main syndromes are outlined here, although there are additional syndromes including neuroferritinopathy and aceruloplasminemia. The most common of the NBIA disorders is pantothenate kinase-associated neurodegeneration , resulting from mutations on the PANK2 gene, accounting for 50%. The classic syndrome manifests in early childhood with a combination of pyramidal and extrapyramidal features . PKAN can also rarely present in early adulthood. There are typical MRI findings, with a central hyperintensity with surrounding low signal on T2 images in the globus pallidus, giving the so-called eye-of-the-tiger sign .
The second main type of NBIA is PLA2G6-associated neurodegeneration . When onset occurs in infancy, PLAN causes progressive motor and mental retardation with cerebellar ataxia, seizures, and pyramidal signs. However, onset can occur later in life which leads to an atypical syndrome that may mimic PD, with rest tremor, rigidity, and bradykinesia and a good response to levodopa. However, patients also exhibit additional features including eye-movement abnormalities and pyramidal signs .
You May Like: Prayer For Parkinson’s Disease
Parkinsons As A Disease Of Neuronal Connectivity
The clinical manifestations of neurodegenerative disorders have been traditionally described from an impaired neuronal circuitry perspective.14 Technological advancements have led to a surge of studies investigating the impact PD has on neural excitability and connectivity utilizing electroencephalogram , neuromodulation techniques, imaging modalities, and graph-analytical methods. Although the field of PD has been somewhat slower to incorporate these concepts compared to other disease models, clinicians now generally acknowledge the complex, multifaceted nature of the disease and the need to pursue multidimensional approaches to study it.
To further establish the clinical applicability of connectome network dysfunction, studies have demonstrated that circuit-specific modulatory therapies, such as repetitive TMS, can alleviate various symptoms of PD, from memory and motor symptoms to depression in PD.31â34 Although from a therapeutic standpoint, there is much to streamline and corroborate with respect to repetitive TMS paradigms and methodologies, there is no denying the potential to providing individualized circuit-specific modulatory therapies.35
How Is Parkinsons Disease Diagnosed
Diagnosing Parkinsons disease is sometimes difficult, since early symptoms can mimic other disorders and there are no specific blood or other laboratory tests to diagnose the disease. Imaging tests, such as CT or MRI scans, may be used to rule out other disorders that cause similar symptoms.
To diagnose Parkinsons disease, you will be asked about your medical history and family history of neurologic disorders as well as your current symptoms, medications and possible exposure to toxins. Your doctor will look for signs of tremor and muscle rigidity, watch you walk, check your posture and coordination and look for slowness of movement.
If you think you may have Parkinsons disease, you should probably see a neurologist, preferably a movement disorders-trained neurologist. The treatment decisions made early in the illness can affect the long-term success of the treatment.
You May Like: Parkinson’s Hallucinations Commercial
What Are The Important Points Regarding Apomorphine At The End Of Life
Apomorphine is a dopamine agonist, which is given as a subcutaneous infusion either continuously or intermittently and also as single subcutaneous injections. An overview of studies into apomorphine use shows improvement in motor off periods and in dyskinesias.39
Apomorphine has side-effects similar to other dopaminergic medication but also notably nausea and vomiting. Ondansetron is not recommended for nausea in patients using apomorphine due to adverse effects.21
Subcutaneous apomorphine has been used at the end of life in a patient with advanced PD although with the recommendation that this is by a healthcare professional experienced in its use.40
What Are The Symptoms Of Parkinsons Disease
Symptoms of Parkinsons disease and the rate of decline vary widely from person to person. The most common symptoms include:
Other symptoms include:
- Speech/vocal changes: Speech may be quick, become slurred or be soft in tone. You may hesitate before speaking. The pitch of your voice may become unchanged .
- Handwriting changes: You handwriting may become smaller and more difficult to read.
- Depression and anxiety.
- Sleeping disturbances including disrupted sleep, acting out your dreams, and restless leg syndrome.
- Pain, lack of interest , fatigue, change in weight, vision changes.
- Low blood pressure.
Don’t Miss: Parkinson Bicycle Cleveland Clinic
Treatment For People With Dementia And Epilepsy
Researchers are still learning about the brain and how seizures and Parkinsonâs disease, Alzheimerâs and other kinds of dementia affect one another.
When it comes to treatment, there is good news. Studies have found that epilepsy drugs help reduce seizure activity in people with dementia and this boosts the quality of life.
Relationship Between Disrupted Neuronal Connectivity And Epileptic Seizures
Epilepsy is considered a disease of network dysfunction.47,48 At a microscopic level, both simple and complex partial seizures involve disruptions in the excitatory interactions between cerebral cortex pyramidal cells.49 From a neurophysiology view, the EEG-graphic representation of an epileptic event is characterized by the paroxysmal onset of hyper-synchronized sharp waves disrupting the neuronal background activity. This activity is often multifocal, reflecting a broader network dysfunction.50,51 Moreover, TMS studies demonstrate similar neurophysiologic features between epilepsy and PD characterized by a state of increased cortical excitability as indicated by reduced intra-cortical inhibition and increased intra-cortical facilitation observed in both patient populations.25,52â55 As mentioned before, in PD, cortical neurons innervating the basal ganglia become hyperexcitable, possibly as a compensatory mechanism following the incremental rise in the output threshold of striatal dopaminergic neurons. As such, it would not be surprising if this putatively maladaptive phenomenon may eventually lead to the generation of epileptiform activity. While epidemiologically, epilepsy-increased comorbidity in patients with PD remains questioned,13,56 our group published the largest case series of patients with PD with concomitant epilepsy57 raising the possibility that epileptic activity in these patients may indeed be under-diagnosed and under-recognized.
Read Also: On-off Phenomenon
Key Points About Absence Seizures
-
Absence seizures are seizures that generally last just a few seconds, and are characterized by a blank or absent stare.
-
Absence seizures usually occur in children between ages 4 to 14, but its possible to have an absence seizure at any age.
-
Absence seizures are easy to miss, but tests and an evaluation of symptoms can diagnose them.
-
Healthcare providers can usually help find the right mix of medications and lifestyle changes to manage absence seizures.
-
Without treatment, school performance, work, and relationships can suffer.
De Novo/early Stage Pd
A preliminary, open-label trial conducted in Japan suggested that a single administration of ZNS was efficacious in improving motor and sleep dysfunction in treatment-naive patients with early stage PD. Moreover, ZNS was recommended as adjunctive therapy in early stage/stable PD according to 2018 guidelines .
Read Also: Zhichan Capsule
Clinical Effectiveness Of Zonisamide
Murata et al. incidentally found that ZNS was effective in treating PD patients. Since then, several clinical trials have been performed to explore the effectiveness of ZNS for the treatment of PD. Based on adequate randomized controlled trials , ZNS is efficacious and safe as an adjunctive therapy in patients with PD . Additionally, the 2018 guideline has supported the use of ZNS for motor symptoms, especially for treating motor fluctuations . We review the clinical trials below further details are summarized in Table 2.
Table 2. Clinical trials on zonisamide effectiveness in the treatment of PD.
Causes Of Parkinson’s Disease
Parkinson’s disease is caused by a loss of nerve cells in part of the brain called the substantia nigra. This leads to a reduction in a chemical called dopamine in the brain.
Dopamine plays a vital role in regulating the movement of the body. A reduction in dopamine is responsible for many of the symptoms of Parkinson’s disease.
Exactly what causes the loss of nerve cells is unclear. Most experts think that a combination of genetic and environmental factors is responsible.
Also Check: Parkinson’s Double Vision
Dementia Alzheimers And Parkinsons Seizures
In recent years, several studies have been published which show that people with dementia diseases are more likely to have epileptic seizures than people who donât have these degenerative conditions:
- Parkinsonâs and epilepsy: One UK study found that people with Parkinsonâs disease were more than twice as likely to have epilepsy than people without Parkinsonâs.
- Alzheimerâs disease and epilepsy: Numerous studies have shown that people with Alzheimerâs are more likely to have seizures. One paper reported that over 40% of people with Alzheimerâs had epileptic activity in their brains.
What Symptoms Can Be Expected In Advanced Pd
- Pain 86%
- Shortness of breath 54%
- Problems in swallowing 40%14
In an analysis of 339 death certificates and medical notes in the UK, pneumonia was found to be a terminal event in 45%.13
Caregiver distress with choking and the risk of choking to death is also mentioned in a separate study in to experiences regarding all stages of PD.4
In a survey of symptoms and their association with quality of life, in those patients with advanced disease, uncontrolled pain, anxiety and hallucinations were significantly associated with poor quality of life.9
Seizures are also noted in a description of the last phase of Parkinsonian syndromes,15 and in retrospective studies of PD patients overall.16,17
These above symptoms often occur on the background of weight loss, pain, and cognitive impairment. It is important therefore to note which medications given at the end of life may exacerbate these symptoms, and which should be considered in anticipation of them.
You May Like: Fitflop Shoes For Parkinson’s
Can Parkinsons Disease Be Prevented
Unfortunately, no. Parkinsons disease is long-term disease that worsens over time. Although there is no way to prevent or cure the disease , medications may significantly relieve your symptoms. In some patients especially those with later-stage disease, surgery to improve symptoms may be an option.