What Else Do We Know
As scientists try to learn what’s at the root of Parkinson’s, they’re looking far and wide to pick up clues where they can.
They’ve found that people with Parkinson’s tend to have something called Lewy bodies in their brain. These are unusual clumps of a protein called alpha-synuclein. The protein itself is normal, but the clumps are not. And they’re found in parts of the brain that affect sleep and sense of smell, which could explain some symptoms of Parkinson’s not related to movement.
Your gut may also have a part in it, as some of its cells make dopamine, too. Some doctors think that this might be where the earliest signs of Parkinson’s show up, but that idea needs more research.
Show Sources
/6symptoms Of Parkinson’s Disease
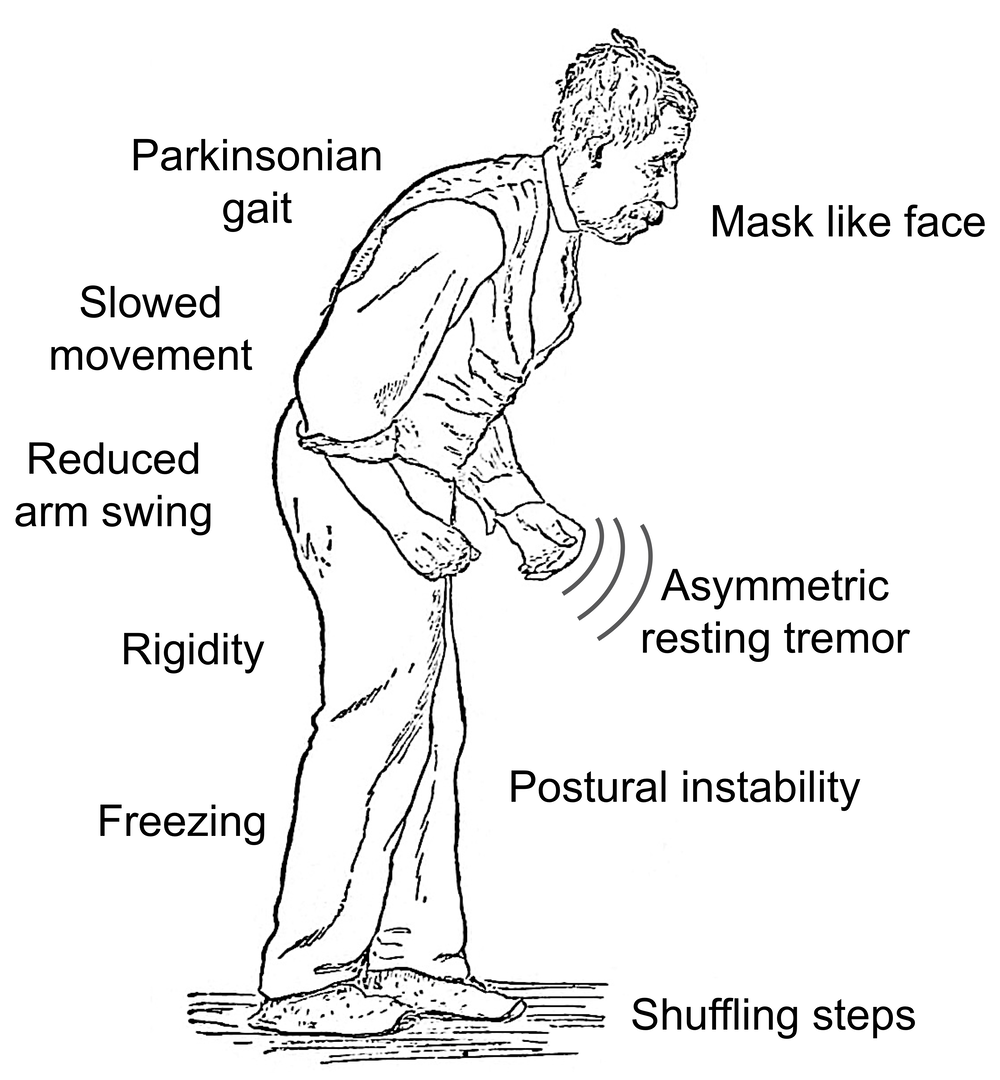
One of the early signs of Parkinson’s disease are tremors. These usually begin in the limbs, hands or fingers. Parkinson’s disease may also slow your movement, whether in walking or performing your everyday simple tasks. Muscle stiffness can happen in any part of the body, and can also be painful. You may experience decreased ability to perform unconscious movements like blinking, smiling or swinging your arms when walking. Your posture may become stooped and you may also experience problems in balancing your body. There can be changes in your speech as well.
What Else Causes Parkinsons
- exposure to toxins
- post-infectious encephalitis
Although doctors do not know exactly what causes Parkinsons disease, they do have a good idea of whats happening inside the brain when someone has the condition.
A part of the brain called the basal ganglia houses neurons that produce dopamine. Dopamine is a neurotransmitter responsible for many functions in the body, like the smooth movement of muscles.
In people with Parkinsons disease, dopamine-producing neurons die or become impaired in their function. As a result, there is less dopamine available in the brain.
Another neurotransmitter called norepinephrine may also be affected in people with Parkinsons disease. This is a neurotransmitter that controls heart rate, blood pressure, and other bodily functions.
Recommended Reading: What Are The Side Effects Of Parkinson’s Disease
Whats The Connection Between Parkinsons And Infections
Some severe viral and bacterial infections lead to encephalitis, which is a dangerous condition that causes inflammation in the brain. Encephalitis can cause Parkinson-like symptoms. This has led researchers to explore the connections between viral infections and Parkinsonism.
To date, this research has been limited. Its possible that infections play a role in the development of Parkinsons disease, but researchers have yet to find any clear connections.
Viruses being investigated include:
To be clear, getting one of these viruses does not mean that you will get Parkinsons disease. Researchers are trying to determine if infectious illnesses may change something in a persons body that makes them more vulnerable to the condition.
Researchers are trying to see if there are connections between illnesses in earlier life and increased risks for Parkinsons disease.
According to a 2019 review of studies , there is some evidence suggesting that:
- People who get the flu vaccination may be less likely to get Parkinsons disease than people who dont.
- People with higher levels of the herpes simplex virus in their bodies may have more severe Parkinsons disease symptoms.
- People with Parkinsons are more likely to have had the Epstein-Barr virus than the general population.
- People with a history of hepatitis C may be more likely to get Parkinsons disease than others.
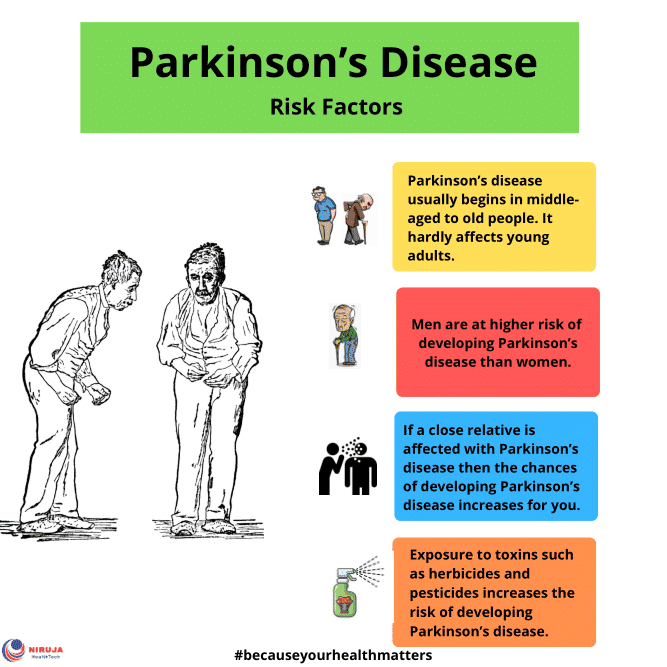
Risk factors for Parkinsons disease include:
Economic Burden Of Parkinson
The cost of Parkinson’s, including treatment, social security payments and lost income from an inability to maintain employment, is estimated to be nearly $25 billion dollars per year in the United States alone. Medication costs for an individual with Parkinson’s disease average $2,500 per year and therapeutic surgery can cost up to $100,000 dollars per patient.
Read Also: What Does Parkinson’s Disease Do
How Is Parkinsons Disease Diagnosed
No single test exists to diagnose Parkinsons disease. Doctors rely on a physical examination and your symptom history to help make a diagnosis. They will look specifically for motor-related symptoms, such as how you walk.
Your doctor may run some tests to rule out other potential causes of your symptoms, like stroke. Tests could include imaging tests, blood tests, and more. Doctors may even prescribe Parkinsons disease medications to see if a persons symptoms improve.
If a person has a considerable family history of Parkinsons disease, its possible that doctors may be able to conduct genetic testing. But this is costly and uncommon.
/6preventing Parkinson’s Disease Symptoms
Parkinsons disease is a neurological movement disorder triggered by a loss of dopamine. Dopamine’s role is to send messages to the part of your brain that controls movement and coordination. Symptoms start slowly at first, but as the disease progresses, it can greatly impact your routine activities. The disease usually develops in middle or late life, most commonly around age 60 or older.
Even though the risk increases with time, a new study has identified an activity that could help halt symptoms and modify the associated risks.
Don’t Miss: Meds Used To Treat Parkinson’s
Increased Risk Of Parkinson’s Disease In Patients With Schizophrenia Spectrum Disorders
Clinical Neurosciences, University of Turku and Neurocenter, Turku University Hospital, Turku, Finland
Correspondence to: Dr. Tomi Kuusimäki, Division of Clinical Neurosciences, Turku University Hospital, Hämeentie 11, POB 52, FIN-20521, Turku, Finland E-mail:
Haidar Al-Abdulrasul MD
Clinical Neurosciences, University of Turku and Neurocenter, Turku University Hospital, Turku, Finland
Department of Neurology, Helsinki University Hospital and Department of Clinical Neurosciences , University of Helsinki, Helsinki, Finland
School of Pharmacy, University of Eastern Finland, Kuopio, Finland
Kuopio Research Centre of Geriatric Care, School of Pharmacy, University of Eastern Finland, Kuopio, Finland
School of Pharmacy, University of Eastern Finland, Kuopio, Finland
Kuopio Research Centre of Geriatric Care, School of Pharmacy, University of Eastern Finland, Kuopio, Finland
Centre for Medicine Use and Safety, Faculty of Pharmacy and Pharmaceutical Sciences, Monash University, Melbourne, Victoria, Australia
Clinical Neurosciences, University of Turku and Neurocenter, Turku University Hospital, Turku, Finland
Correspondence to: Dr. Tomi Kuusimäki, Division of Clinical Neurosciences, Turku University Hospital, Hämeentie 11, POB 52, FIN-20521, Turku, Finland E-mail:
Haidar Al-Abdulrasul MD
Clinical Neurosciences, University of Turku and Neurocenter, Turku University Hospital, Turku, Finland
Are You At Risk Of Parkinson’s Disease These Four Unusual Signs Could Be Clues
Do you move around a lot during your sleep? Or have you lost your sense of smell? New insights into Parkinson’s disease suggest that these might be the early signs of changes in the brain that mean you are at greater risk of developing Parkinson’s.
When people talk about Parkinson’s disease, the image that most often comes to mind is of an elderly person who shakes and has trouble moving. And, in the later stages of Parkinson’s, this is often true. Bradykinesia and tremor are two of the most important symptoms of the disease.
But research over the last 15 years has begun to shed light on some of the changes and symptoms that happen much earlier in the disease, sometimes long before the changes in movement that most people associate with Parkinson’s. So what are these early warning signs that you might be at increased risk of developing Parkinson’s? Here are four of the most common ones.
1. Loss of sense of smell
A common recollection by people who are diagnosed with Parkinson’s is that they remember changes in their sense of smell several years before developing any tremor or other movement problems. But many people might not even recognize that their sense of smell is bad. It is only when tested that we see that up to 90 percent of people living with Parkinson’s have lost their sense of smell.
2. Restless nights
3. Constipation
4. Anxiety and depression
You May Like: Average Age Of Parkinson’s Diagnosis
Who Is Most At Risk For Parkinsons Disease
Parkinsons disease is a progressive movement disorder that affects an estimated 1 million people in the U.S. With PD, nerve cells in the brain break down or die. Many of these nerve cells produce dopamine, a chemical messenger in the brain. This causes abnormal brain activity and impairs movement along with other PD symptoms. Risk factors include age, heredity, and gender. Some of these are clear others are not. Lets look at who is at most risk for developing Parkinsons disease.
Can Parkinson’s Disease Be Cured
No, Parkinson’s disease is not curable. However, it is treatable, and many treatments are highly effective. It might also be possible to delay the progress and more severe symptoms of the disease.
A note from Cleveland Clinic
Parkinson’s disease is a very common condition, and it is more likely to happen to people as they get older. While Parkinson’s isn’t curable, there are many different ways to treat this condition. They include several different classes of medications, surgery to implant brain-stimulation devices and more. Thanks to advances in treatment and care, many can live for years or even decades with this condition and can adapt to or receive treatment for the effects and symptoms.
Don’t Miss: World Parkinson’s Day 2022 Theme
Selected Scientific Articles By Our Researchers
Synergy of pandemics-social isolation is associated with worsened Parkinson severity and quality of life. Subramanian I, Farahnik J, Mischley LK. Social isolation was associated with greater patient-reported PD severity and lower quality of life, although it is unclear whether this is the cause or a consequence of the disease. NPJ Parkinsons Dis. 2020 Oct 8 6:28.
REM sleep behavior disorder in Parkinsons disease: effects on cognitive, psychiatric, and functional outcomes. Mahmood Z, Van Patten R, Nakhia MZ Twamley EW, Filoteo JV, Schiehser DM. Disordered sleep is linked to poorer mental function in patients with PD. J Int Neuropsychol Soc. 2020 Oct 26:894-905.
Characterizing dysbiosis of gut microbiome in PD: evidence for overabundance of opportunistic pathogens. Wallen ZD, Appah M, Dean MN, Sesler CL, Factor SA, Molho E, Zabetian CP, Standaert DG, Payami H. There is a significant overabundance of a cluster of opportunistic pathogens in the guts of persons with PD. NPJ Parkinsons Dis. 2020 Jun 12 6:11.
Neuropathology Of Parkinsons Disease
Macroscopically, the brain in idiopathic PD is often unremarkable with mild atrophy of the frontal cortex and ventricular dilation in some cases. The main distinctive morphological change in the PD brain is observed in transverse sections of the brainstem, where almost all cases present with loss of the darkly pigmented area in the substantia nigra pars compacta and locus coeruleus. This pigmentation loss directly correlates with the death of dopaminergic neuromelanin-containing neurons in the SNpc and noradrenergic neurons in the locus coeruleus . Cell death in the SNpc is mostly restricted to a specific group of neuromelanin-containing dopaminergic neurons, namely the A9 neurons, while other neuronal and glial cell types are largely spared .
Coronal section at the level of the substantia nigra pars compacta in a control and a PD brain stained by hematoxylin and eosin. In both sections, the dark brown cells are the neuromelanin-containing dopaminergic neurons.
You May Like: Ending Parkinson’s Disease A Prescription For Action
How Does Environment Come Into It
Your environment is a hard one to pin down. Partly, that’s because it covers a lot of ground. It’s everything that’s not your genes, which could mean where you live, what you eat, chemicals you’ve come into contact with, and more.
Not only that, but it could take years for the effects from something in your environment to show up. So far, doctors have a lot of clues but no smoking gun. So you could have people who live or work in an area around chemicals tied to Parkinson’s, but many of them don’t get it.
Some research shows links between Parkinson’s and:
- Agent Orange, a chemical used to destroy trees and crops in the Vietnam War.
- Certain chemicals used in farming, such as insecticides, herbicides, and fungicides.
- Some metals and chemicals used in factories, such as manganese, lead, and trichlorethylene .
These can come into play based on where you live, what you do for work, or if you served in the military. Sometimes, these chemicals seep into well water, so that’s one more way they can affect you.
Lewy Bodies And Alpha
In addition to the dopamine deficiency and neuronal loss, PD is also associated with a buildup of intracellular inclusions inside the neurons, called Lewy bodies. Studies have shown that the Lewy bodies are made mainly of a protein called alpha-synuclein.
They are not seen in brain imaging studies but have been detected in research studies that examine the brains of people who had PD and donated their own brains to science for the purpose of research. There is no known treatment or method of removing the Lewy bodies at this time.
In PD, Lewy bodies are found in the substantia nigra as well as other areas, including the amygdala and locus coeruleus , the raphe nucleus , and the olfactory nerve . The functions controlled by these regions can be impaired in PD, although the symptoms arent as noticeable as the tremors and muscle stiffness.
Lewy bodies are also present in the brains of people who have Alzheimers disease and other types of dementia, and they are considered a sign of neurodegeneration.
Don’t Miss: Is Parkinson’s Disease Considered A Disability
Guide To Ltc Planning
From its inception, the goal of the National Care Planning Council has been to educate the public on the importance of planning for long term care. With that goal in mind, we have created the largest and most comprehensive source of long term care planning material available anywhere. This material — “Guide to Long Term Care Planning” — is free to the public for downloading and printing on all of our web sites. Learn More…
What Are The Risk Factors For Parkinsons
In some cases, genetic mutations have been identified in those with PD. However, factors that increase your risk include:
- Age Early onset PD is rare, and those affected start showing symptoms around 60 years of age.
- Heredity Having a family history of PD increases your risk a little, but having multiple family members with PD increases it a lot.
- Gender PD affects 50% more men than women.
There is no known prevention or cure for Parkinsons. Diagnosing PD involves taking a medical history and neurological examination. More work needs to be done through clinical research studies to answer these deficits and improve ways to manage PD.
Brain Matters Research is looking for participants to join upcoming clinical research studies for Parkinsons. Participating in a research study helps us better understand the condition so potential future options can be found. To learn more, call 374-8461, or visit our website.
References:
Recommended Reading: Gut Health And Parkinson’s Disease
What Raises Someone’s Risk For Parkinson’s
It’s a complex picture, but you may be more likely to get Parkinson’s based on:
Age. Since it mostly affects people 60 and older, your risk goes up as the years go by.
Family history. If your parent, brother, or sister has it, you’re a little more likely to get it.
Job. Some types of work, like farming or factory jobs, can cause you to have contact with chemicals linked to Parkinson’s.
Race. It shows up more often in white people than other groups.
Serious head injury. If you hit your head hard enough to lose consciousness or forget things as a result of it, you may be more likely to get Parkinson’s later in life.
Gender. Men get it more than women. Doctors aren’t sure why.
Where you live. People in rural areas seem to get it more often, which may be tied to chemicals used in farming.
Symptoms Of Parkinsons Disease
Parkinsons has four main symptoms:
- Tremor in hands, arms, legs, jaw, or head
- Muscle stiffness, where muscle remains contracted for a long time
- Slowness of movement
- Impaired balance and coordination, sometimes leading to falls
Other symptoms may include:
The symptoms of Parkinsons and the rate of progression differ among individuals. Early symptoms of this disease are subtle and occur gradually. For example, people may feel mild tremors or have difficulty getting out of a chair. They may notice that they speak too softly, or that their handwriting is slow and looks cramped or small. Friends or family members may be the first to notice changes in someone with early Parkinsons. They may see that the persons face lacks expression and animation, or that the person does not move an arm or leg normally.
People with Parkinson’s disease often develop a parkinsonian gait that includes a tendency to lean forward take small, quick steps and reduce swinging their arms. They also may have trouble initiating or continuing movement.
Symptoms often begin on one side of the body or even in one limb on one side of the body. As the disease progresses, it eventually affects both sides. However, the symptoms may still be more severe on one side than on the other.
You May Like: Last Stages Of Parkinson’s Before Death
Characteristics Of The Study Population
After exclusion of individuals with missing data or outliers, 503,497 participants were available for the present analyses. Among these participants, 603 had an incident PD event. Analyses of the associations of CVD risk factors with PD were restricted to the 480,950 participants with no prior history of CVD and included 521 PD cases . The mean duration of follow-up was 9 years in all participants.
Overall, 59.2% of participants were women, 56.0% lived in rural regions, 57.3% had an income less than or equal to 19,999 yuan, and 50.8% had a primary school education or lower. Mean age of PD cases was older than that of the general population , and cases had a lower level of education . Likewise, a higher proportion of PD cases were agricultural workers or were retired compared with the general population .
Most participants were never regular drinkers or occasional drinkers . However, PD cases reported lower mean levels of physical activity than all participants . While 61.2% of men were current smokers, only 5% of women smoked, hence, analyses of smoking were restricted to men. At baseline 5.9% of all participants had diabetes, 32% were overweight or obese , and 33.5% had hypertension.