How Are The Gut And Brain Connected
In a previous blog, we discussed how the ENS is directly connected to the brain through the vagus nerve which travels between the two. We highlighted a theory that suggests that Lewy bodies , the pathologic hallmark of PD, develop first in the ENS and then can migrate to the brain via the vagus nerve. The brain and the gut also communicate via the bloodstream as well, through alterations in inflammatory signals, neurotoxins and neuroprotective factors. One of the elements that contributes to both these communication channels between the gut and the brain is the gut microbiome.
Dive Deep: The Link Between Parkinsons And The Gut
We have discovered for the first time a biological link between the gut microbiome and Parkinsons disease. Sarkis Mazmanian, Caltech
Since we launched our podcast episodes on the neuroscience of Parkinsons and a Parkinsons diagnosis, weve had requests for more information on the link between Parkinsons and the gut.
While great strides have been made in determining the origins of Parkinsons in the body and the link between Parkinsons and the gut, there is still a long way to go.
If youre interested in learning more about this topic, weve rounded up some of the best articles and newest research on the subject so you can dive deep.
Does Parkinsons Begin in the Gut? May 8, 2018
Around half of the people diagnosed with Parkinsons experienced constipation prior to their diagnosis and before their first motor-symptoms began, which makes the move toward more studies that focus on the link between the gut and Parkinsons an exciting one. Especially when you consider what it could mean for treating Parkinsons in the future. This article outlines the workings of the gut-brain highway, the role inflammation plays in Parkinsons and some of the treatments currently being tested.
To learn more about inflammation and viruses that infect and replicate bacteria in those with Parkinsons, read this. And for more on inflammatory bowel disease, read this.
The Gut-Brain Axis in Parkinsons Disease: Possibilities for Food-Based Therapies December 15, 2017
The Gastrointestinal Tract And Parkinsons
As promised in a previous blog, I now return to the topic of the gastrointestinal tract and Parkinsons disease . As most of you know, GI symptoms are very common in PD. We will discuss what those symptoms are, why they occur, and the current research that links what is happening in the gut to theories as to why PD occurs at all. Many of you have suggested gut-related topics for this blog including a discussion of symptoms such as bloating and constipation, and a discussion of the use of probiotics in PD. I will address these issues as well. Submit additional topics that you would like to read about here.
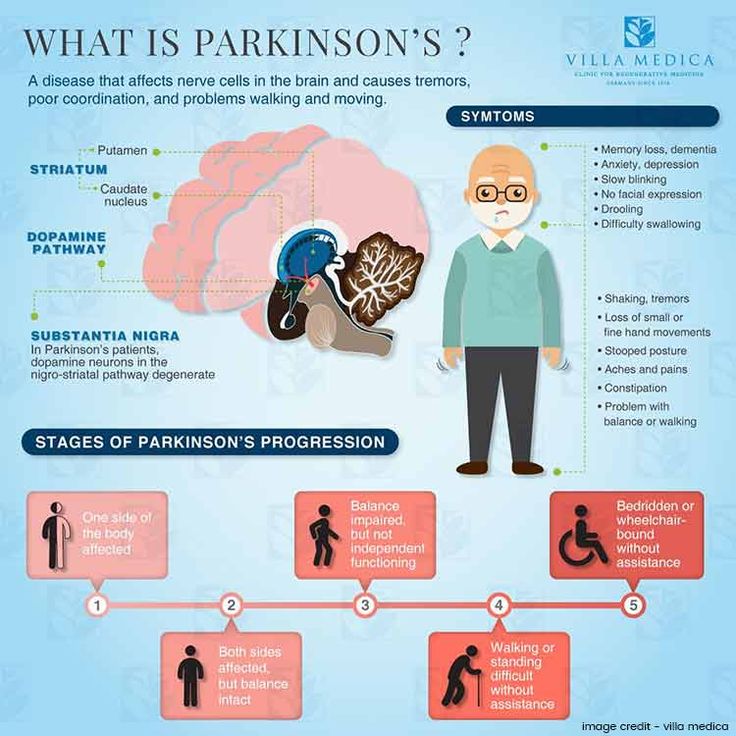
GI symptoms can be among the most bothersome of the non-motor symptoms of PD. Constipation is the most common of these symptoms, affecting 80-90% of people with PD. APDA has a helpful brochure with practical tips to prevent and treat constipation in PD.
GI pathology in Parkinsons disease however, can involve the entire GI tract and includes sialorrhea and dysphagia . In addition, delayed gastric emptying, in which the digestive contents are held up in the stomach and do not move normally into the small intestine, can cause sensations of nausea and bloating.
The gut has its own nervous system
The gut as a biomarker
Entry to the brain
How do Lewy bodies propagate?
Recommended Reading: On-off Phenomenon
Add A Digestive Detoxifying Elixir
An easy way to prepare your gut for the day is to drink a combination of raw apple cider vinegar , lemon, and warm water first thing in the morning on an empty stomach.
Raw apple cider vinegar is a scientifically proven antifungal, helps stabilize blood sugar, and stimulates digestion while lemons are high in Vitamin C. These help kick-start the detoxification of the liver, allowing it to produce bile and move toxins into your stool.
RECIPE:
8 ounces of warm water
Juice from ¼ of a lemon
-
Combine and chug. Swish some water around your mouth and teeth after to help with the taste and protect your tooth enamel.
Can Altering The Microbiome Improve Parkinsons Symptoms
With the awareness that the microbiome may play a role in PD, came the idea that altering the microbiome may help with PD symptoms. While there is still a lot of research to be done, there have been some small, but promising findings so far.
Probiotics, or particular strains of bacteria that are ingested in order to alter the gut microbiome, have been studied to help PD symptoms. A number of small studies suggest that probiotics may improve constipation in people with PD, which is a common problem for many people with the disease.
As mentioned above, treatment of Helicobacter pylori and SIBO typically requires antibiotics, which are drugs designed to kill particular bacteria. Antibiotics can be helpful, but are only considered if a particular gut organism is being targeted. Otherwise, antibiotics can kill both good and bad bacteria, and potentially be detrimental to the overall health of the gut microbiome.
Another idea that has been considered is fecal transplantation, a technique in which fecal matter from a healthy person is delivered to the gut of a person with PD, with the goal of restoring a less PD-like microbiome. Only case reports and very small studies have been reported so far in the literature, but this may be an area worth exploring. There are a few additional studies underway which you can read about here:
Also Check: Parkinson’s Double Vision
Influence Of Age Diet Coffee And Smoking On The Gut Microbiota Composition
The age-related changes in the gut microbiota, in particular a decreased diversity of species, together with other factors including impaired gut motility, impaired gut-blood barrier, and suppressed immune function may be linked to the age-related neurodegeneration. Recent studies reported a great inter-individual variation among elderly regarding the gut microbiota composition, and a significant relationship between microbiota, diet and institution or community living. The gut microbiota-related mechanisms could also explain the differences in PD prevalence between rural and urban environment, between countries or even sexes. Fiber-rich diet enhances the growth of colonic bacteria that produce SCFA, which have systemic anti-inflammatory effect. Therefore, intervention studies with probiotics and prebiotics offer promising way to bring benefits in elderlys health.
Gut Microbiome And Metabolic Changes In Parkinson’s Disease
With increased accessibility to next-generation sequencing technologies, there has been an expansion of studies showing significant, albeit varying, differences in the gut microbiome in PD compared to non-PD controls. These have recently been reviewed by Lubomski et al., ,
Interestingly, several 16S rRNA gene-sequencing studies have shown significantly reduced abundances of butyrate-producing bacteria in PD fecal samples compared to controls.- These findings were supported by a quantitative real-time polymerase chain reaction study targeting butyrate synthesis genes and a gas chromatography study demonstrating significantly reduced fecal levels of short-chain fatty acids in PD patients versus controls. SCFAs are thought to play a key role in microbiotaâgutâbrain crosstalk, in part via the regulation of bloodâbrain barrier integrity, neuronal survival, inflammatory cascades, and endocrine signaling. Butyrate in particular is a major energy substrate for the colonic epithelium and acts to improve gut barrier function. Being a histone deacetylase inhibitor , butyrate has been found to exert neuroprotective actions in experimental PD models,, including the mitigation of PD motor impairment and dopaminergic cell death.-
Recommended Reading: Weighted Silverware
Leaky Blood Brain Barrier And Parkinson’s Disease
which explains how both the blood brain barrier and the gut lining can lose their protective functions in a variety of ways. Given that leaky gut and leaky brain are both heavily implicated in the disease, the road blocks between chemicals produced in the gut reaching the brain is not so assured for people with Parkinson’s. For example, unusually high levels of histamine, which is naturally produced in the gut as part of digestion, have been found in the brains of people with PD
Effects Of Bacterial Metabolites And Components On Pd
The GI tract is an important location for the host immune system to communicate with microbes, and healthy individuals maintain a balance between tolerance for commensals and immunity against pathogens. During intestinal dysbiosis, the metabolites or components of pathogenic bacteria may cause inflammation, combined with metabolic changes in the symbiotic bacteria that regulate inflammation, which, together, result in PD pathology.
You May Like: Diseases Similar To Parkinsons
How The Gut Can Help Diagnose Parkinsons
Dr. Scheperjans explains the motivation for the study, saying, Better understanding the role of the gut in will help us to understand the origin of the disease and to improve treatments.
There is accumulating evidence that at least in some patients, the origin of the disease may lie in the gut with possible involvement of abnormal protein aggregates, local inflammation, and the gut microbiome.
Therefore, further studies into the role of the gut in are important and may reveal new possibilities for diagnosis and treatment, he explains.
In their review, Dr. Scheperjans and colleagues identified four main takeaways:
Furthermore, the study authors appreciate that in the next few decades, the gut microbiota will play a special role in the development of new therapies for Parkinsons. Such therapies can include dietary changes, the use of pro- and prebiotics, and fecal transplants.
Our understanding and appreciation of the importance of the gut-brain connection in grown rapidly in recent years, says Dr. Scheperjans.
We are confident that the coming 2 decades of microbiome-gut-brain-axis research will see an even accelerated development in this area that will reshape our understanding of the pathogenesis of , he adds.
Changes in the gut might be utilized to diagnose earlier new therapies targeting these changes might slow disease progression, reduce constipation, and improve gut function in patients who have already been diagnosed.
Dr. Patrik Brundin, Ph.D.
Gut Inflammation Linked To The Development Of Parkinson Disease
A Danish study of patients with inflammatory bowel disease and Parkinson disease found that patients with IBD had a 22% increased risk of developing PD over patients without IBD. The study, published in Gut, examined all Danish residents aged 15 years or older from 1977 to 2014 in the largest and longest population-based study of links between enteric inflammation and PD.1
A growing body of research points to the role of the gut-brain axis in the development of PD, with inflammation, irritable bowel syndrome, leaky gut, and altered gut microbiota observed in the gut, often years before the onset of symptoms of PD.2 The disease is strongly associated with the accumulation of Lewy bodies, which are eosinophilic deposits that occur within cell cytoplasm and are composed of a misfolded protein, alpha-synuclein. Some research points to the gut as the origin of the misfolded protein, spreading via the vagus nerve into the brain.3 In one study, alpha-synuclein injected in the gut walls of rats migrated to the brain stem through the vagus nerve at a rate estimated to be from 5 to 10 mm per day, thus providing startling evidence of the gut-brain connection.4 In fact, Lewy pathology can be detected in the gut of patients with PD as many as 20 years before their diagnosis via motor symptoms.5 Moreover, increases in intestinal alpha-synuclein are also strongly correlated with changes in gut microbiota that lead to inflammation and elevated permeability of the gut barrier.6
Don’t Miss: On Off Phenomenon
Specific Pathogens As Potential Triggering Factors
Helicobacter pylori: The potential role of Helicobacter pylori in PD, both with regard to the pathogenesis of PD itself and the development of motor symptoms fluctuation, remains controversial. Gastric ulcers, strongly related to HP infection, have been associated with PD since 1960s. Based on the observation of an age-associated increase in the levels of antibodies against HP in PD patients, Dobbs et al proposed that HP infection predisposes to autoimmunity that results in neuronal damage leading to eventual parkinsonism. In fact, HP infection may increase the risk of PD. Nielsen et al showed that prescription of HP eradication drugs and proton pump inhibitors five or more years prior to the diagnosis of PD were associated with 45% and 23% increase in the PD risk, respectively. At the same time eradication of HP infection has been shown to ameliorate symptoms of PD. Currently, HP eradication in PD patients treated with L-dopa is recommended as it may improve the bioavailability of the drug and reduce motor fluctuation.
Moreover, there is an increased mortality from PD amongst livestock farmers, which has been associated with Helicobacter suis being the most common zoonotic Helicobacter in man. That observation is supported by the recent finding that a significantly higher frequency of Helicobacter suis is observed in patients with idiopathic parkinsonism then in control patients.
Braak And The Gut Theory
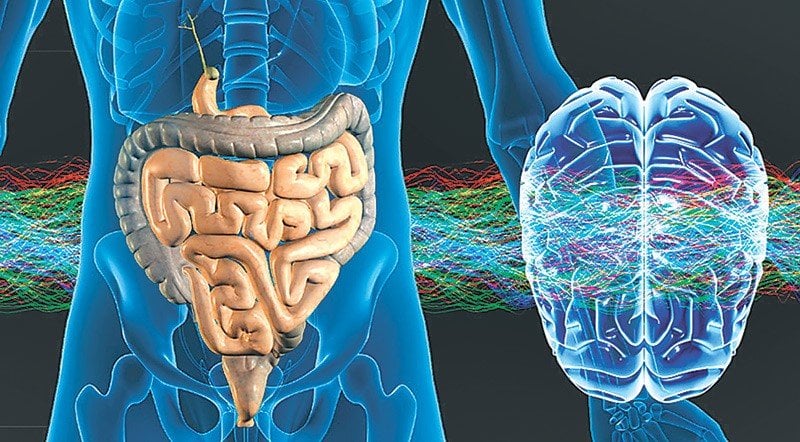
The onset of sporadic PD is unknown, but the Braak hypothesis offers to explain a mechanism for this. Braak et al. proposed the dual-hit theory which suggests that sporadic PD starts in two placesthe neurons of the olfactory system and the gastrointestinal tract . This review will only focus on the GIT aspect of Braaks theory and will only briefly touch upon the involvement of the olfactory network. Braak hypothesized that a foreign pathogen, either bacterial or viral, triggers a response which leads to LP that affects the olfactory and GIT system . Subsequently, neurons allow the retrograde transmission of alpha-synuclein enriched LB to the CNS from the olfactory and the vagus nerve, respectively. The transmission of alpha-synuclein pathology is believed to spread across the nervous system through a prion-like fashion .
A fundamental aspect of Braaks theory is the movement of alpha-synuclein from the enteric nervous system to the CNS via the vagus nerve and dorsal motor nucleus of vagus within the medulla oblongata . The ENS is a network of neurons within the gut wall which works separately from the CNS . The ENS consists of two plexuses, myenteric and submucosal, and has a number of different roles including regulating motility, mucosal blood flow and water transport . The vagal nerve plays an important part in functions of the body, e.g., stimulating salivation, gut peristalsis, and bladder contraction .
Don’t Miss: Pfnca Wellness Programs
Does Parkinsons Begin In The Gut
A growing body of evidence links the neurodegenerative disease to the gastrointestinal tract, opening new possibilities for treatment
The earliest evidence that the gut might be involved in Parkinsons emerged more than 200 years ago. In 1817, the English surgeon James Parkinson reported that some patients with a condition he termed shaking palsy experienced constipation. In one of the six cases he described, treating the gastrointestinal complaints appeared to alleviate the movement-related problems associated with the disease.
Since then, physicians have noted that constipation is one of the most common symptoms of Parkinsons, appearing in around half the individuals diagnosed with the condition and often preceding the onset of movement-related impairments. Still, for many decades, the research into the disease has focused on the brain. Scientists initially concentrated on the loss of neurons producing dopamine, a molecule involved in many functions including movement. More recently, they have also focused on the aggregation of alpha synuclein, a protein that twists into an aberrant shape in Parkinsons patients. A shift came in 2003, when Heiko Braak, a neuroanatomist at the University of Ulm in Germany, and his colleagues proposed that Parkinsons may actually originate in the gut rather than the brain.
Exploring The Link Between Parkinsons Disease And Gut Health
Research at IPAN is finding growing evidence of a relationship between Parkinsons disease and gut health. Find out how you can get involved.
The impact of our gut bacteria on our overall health is an area of science that is generating a lot of interest. While it may seem unlikely that something in our gut can influence physiological processes in the brain, there is increasing evidence to show that it is possible.
IPAN PhD student Nathan Nuzum is specifically investigating the relationship between gut bacteria and Parkinsons disease.
He says not only is it likely that there is a relationship, but that this connection between our gut bacteria and brain may be modifiable through lifestyle factors like diet.
What we know about our gut bacteria and Parkinsons disease so far
Nathans systematic review on gut bacteria and Parkinsons disease found in nine of the 13 included studies that gut bacteria capable of producing a particular short chain fatty acid, butyrate, were less abundant in the Parkinsons groups compared to the groups without Parkinsons.
Nathan said this difference in butyrate-producing bacteria is relevant because of the health promoting functions of butyrate, including maintaining the health of our intestinal walls and providing anti-inflammatory actions within the immune system.
What role might diet play in this pathway?
But what impact might our dietary choices have on the different types of bacteria in our gut and the compounds that they produce?
Read Also: Parkinson’s Bike Therapy
Data Retrieval And Zotu Picking
Raw reads were downloaded from SRA or the European Nucleotide Archive . Adapters were removed using the bbtools suit. Data were analyzed using Lotus and the UNOISE3 algorithm for zOTUs calculation, bundled in a new Lotus version , currently under development. Due to the technical variability among datasets the filtering parameters used by the sdm program called by Lotus, were adjusted for each dataset independently and are reported in the supplementary materials . For the datasets of Petrov et al. and Weis et al., we had to decrease the accepted minimum error due to the low quality of the sequencing data . 16S-based functional predictions were obtained using the default settings in picrust2 and the Metacyc database. In this analysis, the dataset of Qian et al. was not included, as with the default cutoffs the sequences aligned poorly with the reference database used. Count tables for species, genera, families, and functional predictions were then analyzed using R v3.6.2 and processed using the phyloseq R package. We then retained all samples with > 4500 reads, as well as taxa with > 5 counts and predicted functionalities with > 20 counts in at least 2.5% of the samples. These filtration steps left a total of 1211 and 1121 samples for the taxonomic and predicted-function data, respectively. Enterotypes were predicted using rarefied relative abundances of genera via the web-platform.