What Is Deep Brain Stimulation Or Dbs
Deep brain stimulation, or DBS, is often described as a pacemaker for the brain. It works much like a pacemaker, sending electrical signals to the brain instead of the heart. DBS is primarily utilized for patients who have Parkinsons disease, dystonia, or essential tremor, and who cant adequately control their disease with medication. Before any patient is considered for the surgery, they are evaluated by the U-M interdisciplinary team. That team includes a neurosurgeon, neurologist, clinical neuropsychologist, speech pathologist, social worker, and other team members who ensure that you and your family understand the procedure and discuss your expectations and concerns.
Its important to understand that DBS does not offer a cure for your disease, but a way to manage it more effectively. It can offer many benefits, including the need to take less medication and therefore experience fewer medication side effects.
Testing Before Deep Brain Stimulation
For patients with Parkinsons disease, the doctor must confirm that the PD is levodopa-responsive and determine which symptoms are most likely to respond to DBS and discuss these with the patient.
To accomplish these two objectives, the movement disorders neurologist will examine the patient in the absence of his or her PD medications, then again after having taken them. Seeing the effect of PD medications on the movement and non-motor symptoms helps the physician and patient identify good target symptoms for DBS.
A cognitive assessment can help determine a persons ability to participate in the procedure, which involves providing feedback to the doctor during surgery and throughout the neurostimulator adjustment process. This assessment also informs the team of the risk of having worsened confusion or cognitive problems following the procedure.
Some hospitals also perform an occupational therapy review or speech, language and swallowing assessment. A psychiatrist may examine the person to determine if a condition such as depression or anxiety requires treatment before the DBS procedure.
Read Also: Adaptive Silverware For Parkinsons
Which Brain Targets Should Be Used To Implant The Dbs Lead
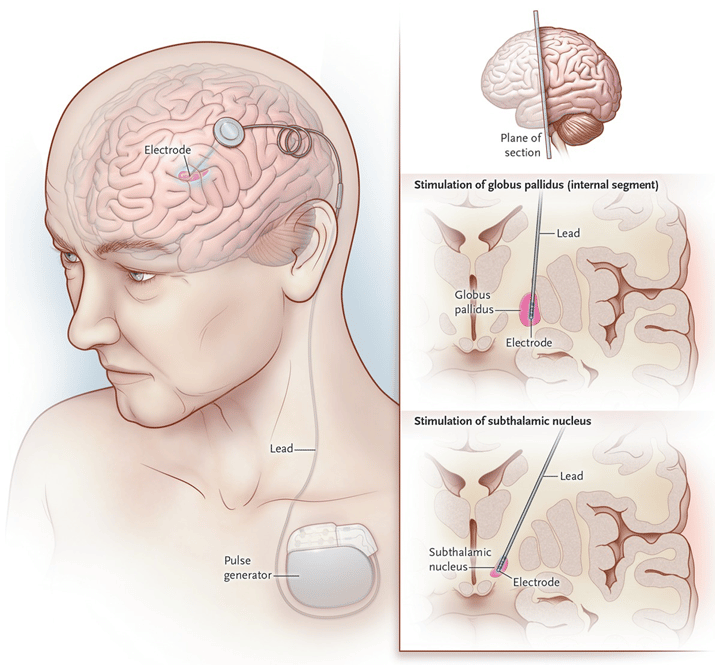
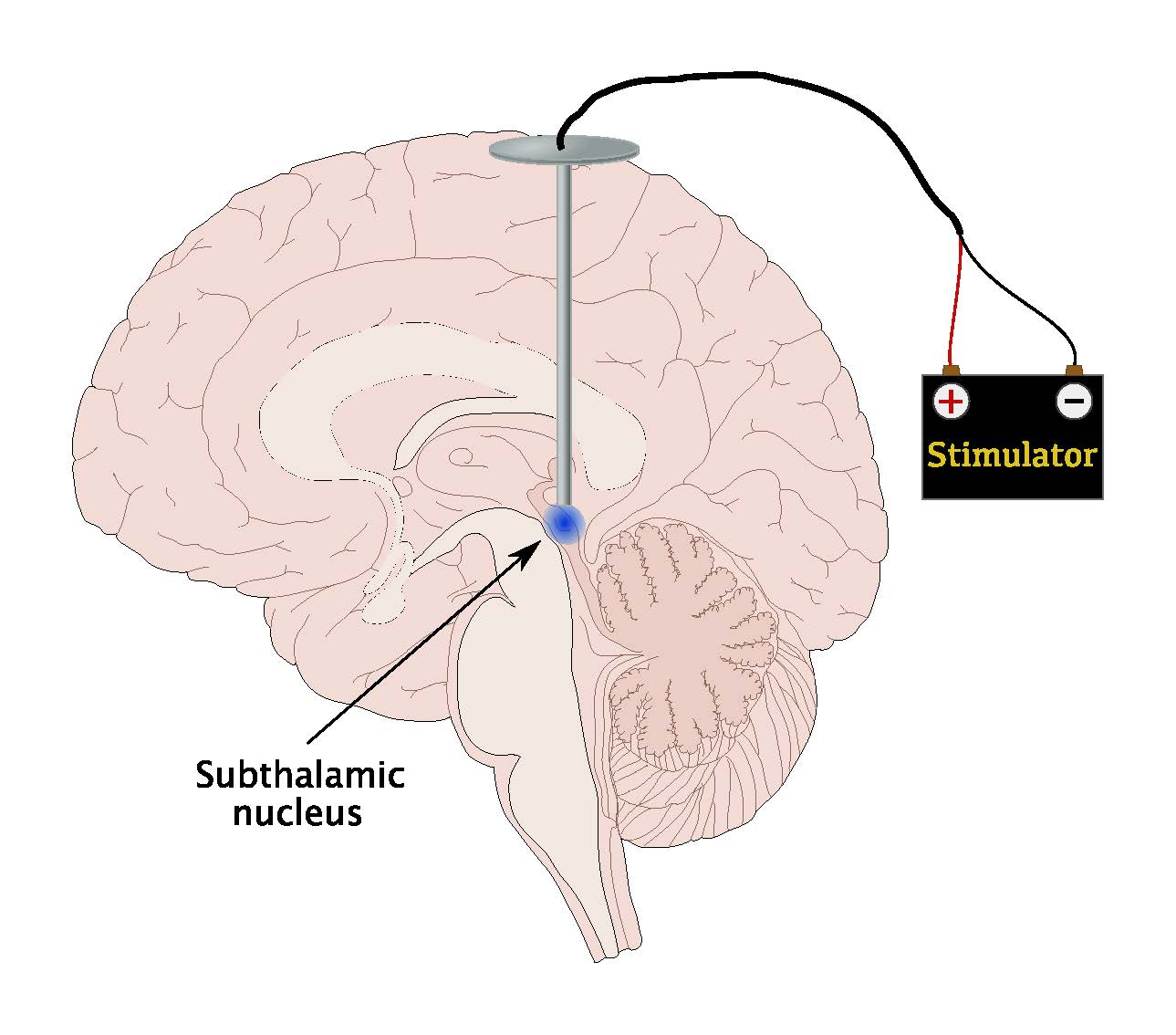
- There are three brain targets that the FDA has approved for use in Parkinsons: the subthalamic nucleus and the globus pallidus interna are the most common.
- The target choice should be tailored to a persons individual needs.
- There are many ongoing studies that will help refine target choice for individual people.
- Although the picture is not yet clear on the issue of target choice, the STN seems to provide more medication reduction, while GPi may be slightly safer for language and cognition.
Read Also: Improving Balance In Parkinson’s Disease
What Happens During The Procedure
In the operating room, your scalp will be injected with numbing medication. Your head will be placed in a frame to keep it from moving. Small holes will be drilled into your scalp to allow the implantation of electrodes.
Youll be awake during surgery so you can respond to questions and move particular areas of your body when prompted. This, along with imaging tests, helps pinpoint the areas of the brain where symptoms originate. This is where electrodes will be placed.
Electrodes may be implanted on one or both sides of your brain. The neurostimulator will be implanted under the skin near your collarbone or lower in your chest. Leads will go underneath your skin from head to shoulder, connecting the electrodes to the neurostimulator. The tiny holes in your skull will be closed.
After surgery, youll be monitored for complications. Youll spend at least 24 hours in the hospital, but longer if you have complications.
Some risks of surgery are:
- bad reaction to anesthesia
Recommended Reading: Zhichan Capsule
How Effective Is Dbs Therapy
Though DBS is considered an alternative, its a well-established, FDA-approved technique that has been used to treat Parkinsons and essential tremor for 30+ years.
Theres been a lot of studies over the years, said Dr. Sheth. Randomized trials have been presented in the top medical journals that show that for the appropriately chosen patient, DBS is more effective than the best medical therapy. So, in that appropriately chosen patient, DBS can be very successful at improving tremor for essential tremor and tremor stiffness, rigidity, and those other motor symptoms of Parkinsons disease.
One patient who has found success with DBS is Rudy Hardy.
Its made a profound difference in my life, said Hardy. A professional sports photographer and professor of criminal justice, Hardys life was controlled by Parkinsons. He tried medication initially, and though it seemed to work for a while, his tremors eventually worsened. Since undergoing DBS, Hardys symptoms are now almost completely undetectable. Watch Hardy talk about his experience with DBS below.
You May Like: If My Father Has Parkinson’s Will I Get It
Development Of A Patient
The focus of research on outcomes from medical procedures has shifted in recent years from purely objective scales to an emphasis on patients perceptions of potential outcome. The majority of clinicians, patients and caregivers report improvements following DBS surgery. Reports of improvement derived directly from questions asked to patients, clinicians and caregivers often fail to correlate. In addition, patient perceptions of outcome are often associated with non-motor factors, including anxiety, perceived social support and nonphysical domains of quality of life. Patients perceptions may thus be less associated with motor and physical factors. Clinicians perceptions seem to be more closely tied to motor symptoms and other physical factors. Finally, caregivers perceptions may not be correlated to many of the outcome variables we typically measure. The differences between patients , clinicians and caregivers all underscore the importance of anxiety, perceived social support and other non-motor factors as important considerations in preoperative DBS discussions .
What Conditions And Symptoms Can Dbs Treat
DBS can treat several conditions that affect your brain, including movement disorders, mental health conditions and epilepsy.
DBS has approval from the U.S. Food and Drug Administration to treat the following conditions:
It’s important to keep in mind that while the above conditions might benefit from DBS, experts still don’t know if this is the case. It usually takes years of research and clinical trials to determine if a medical procedure like DBS is helpful for conditions like these. While researchers are looking into them, DBS surgery to treat these conditions is not common.
Don’t Miss: Parkinson’s And Freezing Up
What Is Deep Brain Stimulation
Deep brain stimulation is a medical procedure that involves a mild electrical current delivered to a specific part of your brain. The electricity in that current stimulates the brain cells in that area, which can help several conditions. The current reaches your brain through one or more wires attached to a small device implanted underneath your skin near your collarbone.
How Is Deep Brain Stimulation Performed
Before the actual procedure begins, for most patients, a head frame is positioned on your head, which keeps your head still during brain imaging and is used to deliver the electrode to the target in the brain. Surgical pins or screws are used to secure the frame to your head. Sedation is typically given during this portion of the procedure.
Your neurosurgeon will implant the deep brain stimulation system in one to three stages.
First, a small hole is made in the skull. The leads, which have electrodes at the ends, are passed through this hole and surgically implanted in the areas of the brain identified as the site responsible for the movements caused by Parkinsons disease.
Most people with Parkinsons disease will require one lead placed on each side of the brain unless symptoms are mostly one-sided . Each side of the brain controls the opposite side of the body, so each lead is inserted on the opposite side of where symptoms are occurring. Sometimes this procedure is done in stages one lead is placed at one time followed by another surgery for the other side. In other patients, both leads are placed during the same operation. Many times patients are awake during lead insertion. An intraoperative MRI is also sometimes used to image the lead location.
You May Like: Social Security Blue Book Parkinsons
Read Also: Does Parkinson’s Disease Affect The Brain
What Are The Risks
No surgery is without risks. General complications of any surgery include bleeding, infection, blood clots, and reactions to anesthesia. Complications related to placement of the DBS lead include seizures, infection, and a 1% chance of bleeding in the brain.
Reasons for which you might need additional surgery include breakage of the extension wire in the neck parts may wear through the skin and removal of the device due to infection or mechanical failure. Additionally, the battery will need to be replaced every 2 to 5 years. Some DBS systems have a rechargeable battery that may last up to 9 years.
DBS may also cause worsening of some symptoms such as speech and balance impairments. In some patients with Parkinsons, DBS may cause or worsen depression. If you develop any side effects from a stimulation adjustment, you need to return to the office for further programming.
Read Also: Similar To Parkinsons
Simultaneous Implantation Into Two Brain Sides Versus A Staged Approach
When considering a simultaneous versus staged approach to DBS, some explanation of the different approaches is required. Two DBS leads may be placed in the same intraoperative sitting , or alternatively they may be separated by days, weeks or months. Similarly, the batteries may be placed on the same day, or alternatively placed days, weeks or even a month following lead insertion. Although there is no data to support the utility for timelines of these various approaches, some DBS interdisciplinary teams feel that extended intraoperative time may be an important factor in increasing complications, particularly in the elderly patient , the frail patient or in the patient with multiple comorbidities. Some teams have also begun to exercise caution in operating on patients over 70 years of age, although this point is highly debatable among the experts.
Recommended Reading: Walking With Parkinson’s Disease
S For Assessing Personality Changes Following Dbs
Supplementary Table 1 gives detailed descriptions of studies included in our review, grouped according to primary methods. Most research used quantitative methods, while qualitative methods are growing increasingly common. There is an emerging trend for studies to assess patient valued characteristics using a mixed-methods approach. Across methods, most studies relied only on self-reports, though a few assessed caregiver or clinician perspectives.
Quantitative Methods
Quantitative research on personality change comes from meta-analyses and primary studies employing retrospective, cross-sectional, prospective, and randomized clinical trial designs. This research has some general limitations. Meta-analyses focused mainly on clinical measures of psychiatric symptoms rather than scales assessing normal range personality. Most retrospective, cross-sectional, and prospective studies included small sample sizes, limiting power to detect small- to moderate effect sizes. And there has been one RCT to date, which decreases the confidence with which causal claims can be made. Additionally, quantitative studies focused almost exclusively on dispositional traits rather than characteristic adaptations and narrative identity.
Qualitative Methods
Patient Valued Characteristics: A Mixed Methods Approach
Can I Use Electrical And Electronic Devices If I Have Dbs Devices Implanted
In general, electronic devices and appliances shouldnt cause any problems with the pulse generator. If they do, the most likely effect is that your pulse generator will switch off. This might not have an immediate effect, but sometimes youll notice that your symptoms get worse, or you’ll notice an unpleasant feeling or sensation.
In general, you should keep in mind the following:
- Your healthcare provider will give you two key items you should keep nearby whenever possible: an ID card and a patient programmer. The ID card can help you in situations with certain kinds of electronic devices like metal detectors or anti-theft scanners. The patient programmer allows you to turn the device on and off, plus adjust settings for the stimulation if needed.
- Home appliances, such as microwaves, computers, smartphones and other common electronics, shouldnt cause any kind of interference or problems with your pulse generator.
- Having one or more DBS leads and a pulse generator implanted in your body means you can’t have certain medical and diagnostic imaging procedures. The procedures you can’t have are magnetic resonance imaging scans, transcranial magnetic stimulation and diathermy.
Don’t Miss: What Are The Early Symptoms Of Parkinson’s
Research To Improve Deep Brain Stimulation
Researchers are working to improve upon existing DBS devices and methods to help treat more symptoms and more people. Some researchers are putting electrodes in a different area of the brain the pedunculopontine nucleus to treat walking and balance problems that don’t typically improve with present-day DBS. Others are developing a “smart” DBS device that can record a person’s unique brain signals and deliver electrical stimulation only when needed, such as when symptoms return, rather than continuously, as the current systems do. This could help reduce side effects such as numbness and weakness and lengthen the battery life of the neurostimulator, which would result in a longer time between battery replacement procedures.
Scientists also are planning to test deep brain stimulation in the first years after a Parkinson’s diagnosis to see if the therapy may slow or stop disease progression. Testing in Parkinson’s models showed the therapy may help protect brain cells, and a small human trial showed motor symptoms improved after early-stage DBS.
Parkinsons Disease Symptoms Creep In
Meanwhile, Craigs health deteriorated. By 2016, his ability to operate equipment that makes full-sized pickups look like Tonka trucks was no longer possible, and he went on disability. Walking became increasingly difficult, to the point that a walker, and, later, an electric wheelchair, came into play. An expert archer and bowhunter, Craig found himself unable to handle his bow. Other activities he loved camping, four-wheeling in the Black Hills, fishing with his grandson Hayden suddenly seemed out of reach. Fatigue and sleep problems, common Parkinsons symptoms, crept in. Making matters worse, the levodopa played havoc with his digestive system.
He couldnt eat, wouldnt eat, Susan recalled.
As so often happens, physical challenges brought psychological barriers, and justifiably. Craig couldnt walk into a store and be entirely sure he would be able to walk back out of it because, as he put it, my muscles would just stiffen up. Craig started skipping his grandsons youth baseball and basketball games games he loved to watch for the same reason. He increasingly ended up watching a lot of TV by himself.
I had no ambition. Things I really enjoyed, I didnt want to do anymore, Craig said.
Susan, working full-time as the treasurer of Weston County, never quite knew what to expect upon returning from work.
Also Check: Pfnca Wellness Programs
Recommended Reading: Parkinson’s Disease Latest News
Role Of The Funding Source
The sponsor and the participating centres designed and approved the protocol. Medtronic monitored the study and the data were entered into a validated database. A statistician employed by the company performed the statistical analysis based on specific requests of the investigators. Final data were made available to the authors who independent of the sponsor assessed the data analysis as well as the interpretation and writing of the results.
Living With A Stimulator
Once the DBS has been programmed, you are sent home with instructions for adjusting your own stimulation. The handheld controller allows you turn the stimulator on and off, select programs, and adjust the strength of the stimulation. Most patients keep their DBS system turned on 24 hours day and night. Some patients with essential tremor can use it during the day and turn off the system before bedtime. Your doctor may alter the settings on follow-up visits if necessary.
If your DBS has a rechargeable battery, you will need to use a charging unit. On average charging time is 1 to 2 hours per week. You will have a choice of either a primary cell battery or a rechargeable unit and you should discuss this with you surgeon prior to surgery.
Just like a cardiac pacemaker, other devices such as cellular phones, pagers, microwaves, security doors, and anti theft sensors will not affect your stimulator. Be sure to carry your Implanted Device Identification card when flying, since the device is detected at airport security gates.
Recommended Reading: How Long Do You Live With Parkinson’s Disease
A General Rule Is That Dbs Will Likely Improve Parkinsons Symptoms That Respond To Medication
The Evaluation prior to DBS Surgery
A team of experts, including a movement disorder specialist and a neurosurgeon , conduct an extensive assessment when considering DBS for someone. The evaluation consists of medication and symptom review, examination both on and off Parkinsons drugs, brain imaging, and oftentimes also detailed memory/thinking testing . If DBS is offered, its important to discuss the expected benefits as each persons experience is unique. Its also critical to discuss the potential surgical risks, including bleeding, stroke and infection.
The DBS Procedure and Device Programming
In DBS surgery, thin wires called electrodes are placed into one or both sides of the brain in specific areas that control movement. Usually a person remains awake during surgery so that he or she can answer questions and perform certain tasks to make sure that the electrodes are positioned correctly. However, some medical centers now are using brain imaging to guide the electrodes to the right spot while a person is asleep. Each method has its pros and cons and may not be suitable for everyone or available everywhere.
Once the electrodes are situated, they are connected to a battery-operated device that is typically placed under the skin below the collarbone. This device, called a neurostimulator, delivers continuous electrical pulses through the electrodes to decrease Parkinsons symptoms.
How DBS Works
Research on DBS
Who Should Consider Dbs
DBS is an option to consider if symptoms cant be adequately controlled by medication, are progressing, are becoming more difficult to manage, and are impacting quality of life. You may also want to consult your physician to see if DBS is the right treatment for you if:
- Medications no longer work as quickly or effectively as they used to.
- You have to take medications multiple times per day.
- You are taking progressively higher doses of medication for the same effect.
- Medications required to control symptoms result in unacceptable side effects such as hallucinations and/or dyskinesias.
- The side effects of medication have become intolerable.
Don’t Miss: Parkinson’s Dementia And Weight Loss