Complex Exercises Reverse Gait Freezing In Parkinsons Disease Study
A challenging physical training program has helped reverse the symptom of gait freezing in study participants with Parkinsons disease, according to investigators from Brazil.
People with freezing of gait cannot move their feet forward despite the intention to walk, a problem that not only interferes with daily functioning but can lead to falls. Researchers at the University of São Paulo recently tested a 12-week exercise protocol that stimulates motor and cognitive skills at the same time.
The 32 study participants, who had stage 3 or 4 Parkinsons disease, performed adapted resistance training exercises that combined instability, weight lifting, motor coordination and cognitive demands. The exercises were done concurrently to create the complexity necessary to stimulate significant brain changes, explained doctoral candidate Carla da Silva Batista.
This demands considerable effort from the patient and confidence on the part of the trainer, who will invariably have to give patients some support so they dont fall, Batista said.
Significant functional improvements were found following the trial, including a 60% reduction in gait freezing and a 70% reduction in motor symptoms. Measurements of brain activity before and after the training program also showed changes in the brain regions linked to gait freezing, and enhanced brain activity and plasticity in the regions affected by Parkinsons disease, the researchers reported.
How Does Anxiety Cause Freezing Of Gait
Recently, imaging studies have begun to identify neural correlates associated with freezing behaviour. Although these studies did not focus on inducing anxiety to provoke freezing of gait, it is interesting that decreases in activation were found in the medial prefrontal cortex, left anterior insula and left ventral striatum during motor arrests compared to walking . Although these regions are involved in an array of functions such as the cognitive control network , these areas also have a well-established role in emotional processing . A recent review highlighted that nearly 60% of emotional induction studies reported activation of the insula , and furthermore the insula has been suggested to participate in evaluation of distressing thoughts and interoceptive emotional responses . Imaging results have also shown that Freezers have significantly less BOLD signal in the bilateral anterior insula and bilateral ventral striatum compared to Non-Freezers during simulated walking in virtual reality with increased cognitive load . Taken together, these results align with the current findings and theoretical framework suggesting that dysfunctional processing of emotional information in the ventral striatum might be one explanation of the current results showing that anxiety increased freezing of gait.
Techniques To Overcome Freezing
Physical therapy and occupational therapy can be helpful to reduce or overcome freezing episodes. Physical therapy focuses on the physical rehabilitation of people recovering from injuries or disease with the goal of restoring mobility, as well as educating patients on managing their condition to maintain long-term benefits. Occupational therapy also deals with rehabilitation and motion but is focused more on enabling the person to engage in daily activities as seamlessly as possible. Occupational therapists also suggest adaptations and modifications to the persons environment.3
There are several techniques that can help people with PD overcome freezing, including:
As with any symptom, patients who experience freezing episodes should mention this to their neurologist who is managing their care. The neurologist may make changes to medication or provide a referral to a physical or occupational therapist.
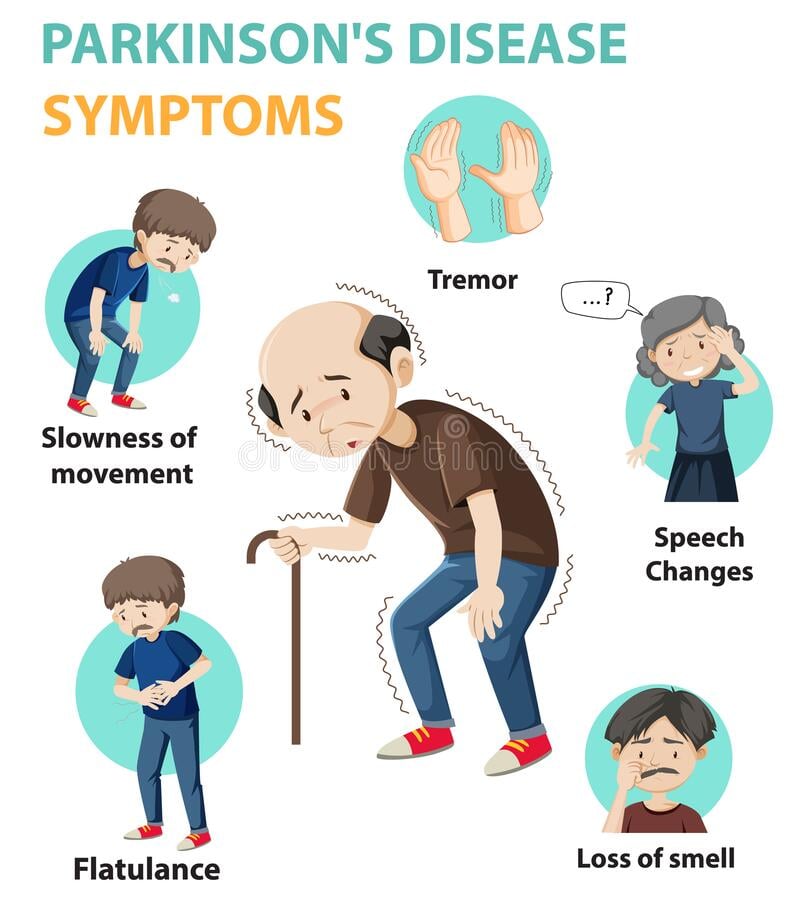
Recommended Reading: Classic Signs Of Parkinson’s Disease
Summary Of Pharmacological Treatments For Fog
Continuous subcutaneous apomorphine infusion is reversible and more convenient than LCIG, but the result of one small study was disappointing. The efficiency of subcutaneous apomorphine infusion on FOG needs to be tested in future studies. It is worth noting that several studies supported that the DA increased the risk for FOG , physicians should take caution while prescribing DA for PD patients with FOG. There was lack of strong evidence that oral amantadine can improve FOG and two double-blind, randomized, placebo-controlled studies found that intravenous amantadine had no beneficial effect on FOG . L-DOPS plus entacapone were shown to be effective in improving FOG, but whether L-DOPS alone could improve FOG needed further studies . An underlying loss of cholinergic function contributes to freezing, but the recently double blind placebo-controlled study did not find FOG improvement after acetylcholinesterase inhibitor rivastigmine treatment , although a previous open label controlled study showed positive results under another acetylcholinesterase inhibitor galantamine treatment. Botulinum toxin and Atomoxetine are ineffective according to the clinical evidence.
Parkinsons Disease: Stimulation Of Brain Feet May Help People Overcome Freezing Episodes
During a freezing episode, a patient feels like their feet are stuck to the ground for a few seconds or more while they are trying to take a step. You can be walking or trying to stand up from a chair and your body does not respond anymore to your commands, said Francesco Cecchini, co-founder and CEO of Gondola Medical Technologies in Switzerland. Patients can very often fall following a freezing episode.
Furthermore, when other people are around, the inability to move is more likely to occur and can be more intense. In Sanvitos case, having colleagues stare at him during a meeting would result in a more extreme episode.
More than half of people with advanced Parkinsons disease experience freezing of gait but existing treatments dont work for everyone and have limitations. Medication helped Sanvito, for example, but the effect would wear off so he had to plan his work agenda around his pill schedule.
In some cases, physiotherapy can also alleviate the symptom, especially if combined with cues such as stepping sideways first or timing steps to a rhythmic beat. And deep brain stimulation a procedure where two electrodes are implanted in the brain and stimulated with electrical impulses can provide relief but requires major surgery and can cause discomfort.
Brain mechanisms
A portable device that stimulates two areas of the foot could help prevent freezing of gait episodes. Image credit: Gondola MedTech SA
Connectivity
Also Check: What Benefits Can You Claim For Parkinson’s Disease
Insights From Reductionist Observations
As highlighted above, many reductionist studies comparing patients with and without FOG across clinical features and a range of biomarkers have provided insights into the role of many different physiological processes and anatomical regions. For example, a lesion analysis performed in a series of 14 patients who developed FOG, demonstrated discrete disturbances in the cerebellar locomotor region , an area functionally connected to the dorsal medial cerebellum . Work from a recent meta-analysis of neuroimaging studies in PD has also suggested that CLR activation may play a compensatory role in locomotion . As outlined above, other studies have suggested a more generalized pathophysiology, which has allowed a common final pathway to be postulated . However, the question must be raised as to whether all the relevant anatomical regions work together to produce a common input to this pathway or whether they speak separately to this single common pathway or multiple pathways.
Tips To Get Moving Again
When you get stuck, these tricks from the National Parkinson Foundation can help:
- Be aware of freezing triggers and prepare strategies in advance.
- Shift the weight of your body from one leg to another.
- Listen to music and step with the rhythm.
- Hum, sing, or count.
- Imagine a line to step over or focus on a target on the floor to step on.
- Use a mobile laser device to create a line in front of you to step over.
- Turn by walking half a circle instead of by a pivot turn.
You May Like: Neuropathy And Parkinson’s Disease
Ways To Manage Freezing
From treatments such as physiotherapy, to cueing techniques you can do yourself, there are different things that can help you manage freezing.
Speak to your GP, specialist or Parkinsons nurse about the best treatment for your freezing. They can also refer you for therapy that may help. Treatments include:
Understanding Phenomenology And Pathophysiology
Despite an abundance of clinical experience from direct observations, there are still a significant number of fundamental gaps in our understanding of FOG despite the proposal of several pathophysiological models . These range from the very basic grasp we have on phenomenology through to the more nuanced appreciation of its underlying neurobiology that manifests clinically.
Read Also: Drugs That Can Mimic Parkinson’s Disease
How Are Motor Fluctuations Treated
Motor fluctuations affect the quality of life of people with Parkinsons significantly by limiting their activities of daily living, mobility, and social interaction. The treatment aims to keep the person moving and make them carry their daily activities independently.
Doctors can use any of the following strategies to help the affected people to minimize or avoid motor fluctuations:
- Adjusting the dose of levodopa: The doctor can either increase the dose or change the number of times the drug is taken in a day.
- Introducing different medications: Adding different medications to the current medication can help maintain consistent levels of dopamine and thus, prevent off-times.
- These medications include
Noninvasive Vagus Nerve Stimulation
Recently, it has been reported that VNS administered for 10days improved locomotion in a rodent model of PD . Thus, an observational, open-label, pilot study explored the effect of single-dose, noninvasive VNS on gait pattern and FOG in 12 patients with FOG. A total of 2 VNS treatments were applied to the left vagus nerve in left side of the neck below the mandibular angle, medial to the sternocleidomastoid muscle and lateral to the larynx, with an interval of 15min between 2 VNS treatments. Each VNS treatment consisted of 120s of stimulation. Assessments were performed just before and 15min after the application of VNS. Video analysis showed that VNS significantly improved the number of steps taken while turning . The mechanism was still unknown. One possibility is that locus coeruleus noradrenergic neurons degenerate prior to substantia nigra dopaminergic neurons in PD, and VNS may activate locus coeruleus neurons . A multicenter, double-blind, placebo/sham-controlled randomized trial of noninvasive VNS in patients with PD are needed.
Recommended Reading: Exenatide Trials For Parkinson’s
Current Approaches And Hurdles In Parkinsons Disease Freezing Of Gait
In this 52-minute talk Lan Luo, MD, from the Parkinsons Disease and Movement Disorders Center at BIDMC explains freezing of gait , including how FOG manifests, FOG triggers, ‘on,’ vs. ‘off’ FOG, the brain pathways that are implicated in FOG, who gets FOG, several available treatments, and how to avoid falls.
Freezing Of Gait And Balance Disturbances: Lumping Versus Splitting
The concurrence of FOG and balance disturbances in advancing PD is hard to ignore but for the purposes of computational modeling, knowing if these features are related neurobiologically or are discrete, is of critical importance. Previous studies have identified the overlap between poor balance and FOG , as well as identifying that a deterioration in balance may be a useful predictor for those patients developing FOG .
Anatomically, it would seem intuitive that the neural pathways serving gait and balance do demonstrate a degree of meaningful overlap that could link these processes but this does not necessarily represent a fixed anatomical connection and may perhaps be more functional. For example, dopamine loss is the hallmark of PD but can also be seen in some people with vascular parkinsonism and normal pressure hydrocephalus, who also experience FOG and falls . Indeed, whilst both FOG and balance disturbances are frequently related in PD, they can occur independently, suggesting that their pathophysiologies may, to some degree, be separable. In one recent study, PD patients reported that 61% of falls were due to FOG rather than being attributed to slips, trips, balance loss, or syncope .
You May Like: Is Parkinson’s Disease Progressive
Research Reveals Cause Of ‘freezing’ Gait In Parkinson’s
- Dennis Thompson
MONDAY, Sept. 12, 2022 — Researchers think they’ve figured out why Parkinson’s disease causes a person’s limbs to become so stiff that at times they can feel frozen in place.
Using a robotic chair equipped with sensors, a research team has linked the activation of leg muscles in Parkinson’s patients with a region of the brain called the subthalamic nucleus.
This oval-shaped brain area is involved in movement regulation, and data from the chair show that it controls the start, finish and size of a person’s leg movements, according to research published Sept. 7 in Science Translational Medicine.
“Our results have helped uncover clear changes in brain activity related to leg movements,” said senior researcher Eduardo Martin Moraud, a junior principal investigator at the University of Lausanne in Switzerland.
Shake Off Your Stress
Freezing episodes are more frequent and intense when youre anxious. Anxiety leads you to tense up your hands, arms, shoulders and jaw which raises stress in your body and feeds your freezing, making you even more anxious!
To combat this vicious cycle, deliberately give your body a good shake before you start walking. Start with loosening and shaking your hands, arms, shoulders, neck and tongue. Take a deep breath, stay as relaxed as possible and set out towards your destination!
Don’t Miss: Nursing Diagnosis For Parkinson’s Disease
Nutrition Hydration And Gut Health
- A diet which supports your tummy motility can help avoid some of the associated complications of PD such as constipation.
- Being consistent with a Mediterranean diet may also be positive step.
- The problem with nutrition research to date is that there is a lack of quality and depth.
- The recommended approach is to work with a skilled Dietician or Nutritionist to help provide you with a personalized plan.
Also Check: Parkinsons Disease Fun Facts
How Do These Findings Fit Within Existing Models Of Freezing Of Gait
It is important to consider how some models of freezing of gait describe a downstream effect, without addressing the upstream cause. This might be why other models are not able to explain how anxiety or other processes might overload the basal ganglia, leading to increased freezing of gait. For example, the threshold model predicts that a motor deficit can accumulate to the point that reaches a threshold and freezing occurs . This model does not identify a root cause of the initial motor deficit. According to the current results, anxiety might be the key factor that initiates the motor deficit in the first place, and thus this model would be incomplete without the upstream cause having been identified. Similarly, the decoupling model does not identify the initial upstream event that leads to decoupling between preprogrammed and intended motor responses . Thus, in both cases identifying the upstream cause can elucidate why freezing of gait is the resultant behaviour.
You May Like: Anxiety And Parkinson’s Disease
What Can Be Done To Thaw One Out When Freezing Occurs
There are various cues and/or tricks that can be tried with your physical therapist to determine which cue will work best for you. Examples of such cues include:
- Visual cues: Provide feedback to through your eyes and visual system to provide you with a location to place your foot when stepping. Visual cues include: lasers on canes and U-step walkers, placing lines of tape on the floor, placing Xs of tape in a semi-circle in tight spaces, and stepping over the foot of the therapist while gait training.
- Auditory cues: We rely on feedback through our ears to establish a rhythm step to the beat. These cues come in the form of music, counting out loud 1,2, 3.., or using a metronome. There are also applications for smart phones that can provide sounds like a metronome that your therapist can demonstrate for you!
Not every cue works for every patient! But it is important to consult with your PT to find which one will help you.
References:Lohnes CA, Earhart GM. The impact of attentional, auditory, and combined cues on walking during single and cognitive dual tasks in Parkinson disease. Gait and Posture 33 478-483.
Plotnik M, Giladi N, Balash Y, Peretz C, Hausdorff J. Is freezing of gait in Parkinsons Disease Related to Asymmetric Motor Function? Annals of Neurology. Vol 57 No 5, May 2005
What Causes Freezing Of Gait In Parkinsons
There are significant differences between people with Parkinsons who experience freezing of gait and those who dont. However, there are some commonalities that may help to explain why some people with Parkinsons disease develop this symptom while others dont.
One theory is that freezing of gait occurs when certain brain areas are unable to properly process information from the body regarding movement. This can be due to damage to the parts of the brain that control movement, or it may be due to changes in the way that information is transmitted between the different parts of the brain.
Another theory is that freezing of gait may be a result of an imbalance in the neurotransmitters in the brain. Neurotransmitters are chemicals that help to transmit signals between the different parts of the brain. If there is an imbalance in the neurotransmitters, it can lead to problems with movement.
Yet, another theory involves the contribution that step length has to FOG.
Freezing of gait has been identified as one of the main contributors to gait disturbances in Parkinsons disease. While the pathophysiology remains enigmatic, several factors such as step length and the sequence effect may lead to the occurrence of FOG.
Freezing episodes can be triggered by factors such as fatigue, stress, anxiety, changes in the environment, or an uneven surface. In some cases, freezing may be a side effect of medication.
Recommended Reading: Jobs For Parkinson’s Patients
Passive Remote Patient Monitoring Of Physical Activity: Opal Actigraphy
In addition to active assessments, sponsors seek ways to capture continuous real-world patient activity measures via remote passive monitoring. Clarios Opal® actigraphy solution quantifies daily physical activity to complement QOL & ePRO data for any trial. Combining objective measurements from wearable sensors with qualitative ePRO creates a comprehensive picture. Data is collected passively from patients wearing a single Opal sensor on their wrist.