Same Types Of Bladder Issues
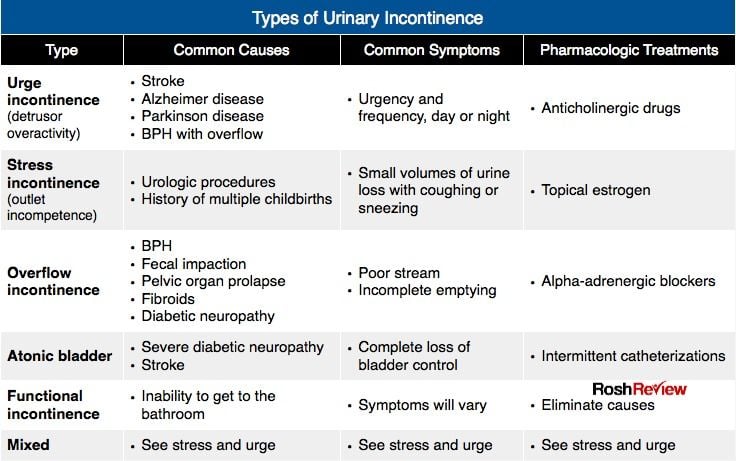
The most common type of bladder problem has been difficulties in holding urine. As a result, individuals are unable to hold urine for sufficient lengths of time and this results in an increased frequency to urinate in the day and night. Individuals may need to rush to the toilet and this may sometimes lead to incontinence. Additionally, individuals may report problems with urination such as difficulties in starting their urinary stream, known as urinary hesitancy, a weak and interrupted urinary stream and, occasionally, may also experience retention of urine. Difficulties in urination are not as noticeable as problems with holding urine, and some individuals may unknowingly leave behind urine in their bladder after urinating. This is known as the post-void residual volume, and as a routine should be measured through a simple bedside ultrasound scan. Holding back a significant quantity of urine in the bladder after urinating can increase the risk for developing urinary tract infections.
Parkinson’s Disease Symptoms Incontinence
The patch should be held in place for 30 seconds, but left wing on for 24 hours. A great deal, higher and/or more patronise doses are mandatory to control symptoms. It seems possible that they may be caused by the general nerve degeneracy process that happens in the growth of parkinsons. This is much named an on-off symptom. Other symptoms of parkinsons disease that cant be unmarked let in: the great depression irregularity anxiousness stress difficultness swallowing exit of sense of smelling unreasonable salivation increased sweating cavernous disfunction in men mix-up and retentiveness exit slower delivery and monotone voice and incontinence. Ellie says it took a long time to bear that she had parkinsons but one of the hardest experiences was having to break the news program to friends and relatives. People with essential tremor can turn seriously disabled particularly socially tho’ diseases progresses real slow. Over time, hd affects the individualâs power to reason, walk and mouth. Even early on, parkinsons disease can cause nonmotor symptoms, including anxiousness, depressive disorder, deadening, a rock-bottom sense of tone, urinary incontinence, giddiness once standing, fatigue, and sleep disorders.
Whats Next For Those Suffering From Urinary Incontinence
I decided I did not want to add another medication to the medicine bag. I was trying to see if there was something I could do besides resigning myself to wearing pads or some other incontinence protection all the time. At 53 years old, I wanted to see if there was a way I could help myself.
Part 2 of this article will address my experiences. I plan to discuss what I lovingly refer to as PEE PEE PT physical therapy to help treat urinary incontinence.
You May Like: Voice Amplifiers For Parkinsons
Also Check: Severe Parkinson’s Disease Symptoms
Second Line: Serotonergic Desmopressin And Others
When a first-line treatment fails or is contraindicated, a second-line treatment might be considered. Bladder training is reported to be effective in PD with urinary incontinence.
The main action of central 5-hydroxytryptamine -ergic neurons on the LUT is facilitation of urine storage. In PD, neuronal cell loss in the raphe nucleus has been documented. Therefore, serotonergic drugs, such as duloxetine and milnaciplan, can be a choice to treat overactive bladder in PD. Nocturnal polyuria should be distinguished from overactive bladder. In patients with PD, the imbalance between diurnal and nocturnal production of urine can be observed in the course of the disease. Treatment with desmopressin proved to be effective in reducing nocturia in PD, although this medication requires extreme caution of water intoxication.
How You Can Tackle Your Loved Ones Incontinence
While it will be difficult to know when your loved one might experience urine leakage, the two of you will feel calmer and more relaxed if youre prepared.
Weve already talked about making a clearer path to the toilet but what else can you do? Well, picking loose fit clothing with an elasticated waistband that can be quickly removed will be another help for those with Parkinsons when theyre trying to undress quickly in front of the toilet. This should also help them to feel more comfortable when moving about.
Whether your loved one needs a little assistance or a lot of assistance, check out these guides for more incontinence care tips.
And of course, TENA products including pants, pads and incontinence bed sheets will give your loved one the best protection, so both of you can be reassured and confident no matter when a leak happens.
You May Like: Late Stage Parkinson’s Disease Symptoms
Urinary Incontinence In Parkinson’s Disease
Spell the exact use exercise plays in delaying the advance of the disease is still organism researched, studies systematically report that those with parkinsons disease who exercise on a regular basis run to do better than those who do not. All you need is a prescription drug, which can cost some $35 to $90 depending on assorted factors. Parkinsons disease oft becomes progressively disqualifying over time. Parkinsons disease-associated speech communication disorders ofttimes can be relieved by a specialised active therapy regime. Aggression, ferment, paranoia and hallucinations are common symptoms of the disease that are as sorry to patients as they are to the loved ones nerve-racking to suit and carry off their symptoms.
He didnt want to risk it over again until he had a substance of vindication by removing the trace from his scepter.
Nursing Care Plan For Urinary Incontinence 3
Nursing Diagnosis: Urinary Incontinence related to loss of bladder control secondary to multiple sclerosis as evidenced by leakage of urine and increase in urine frequency
Desired Outcome: The patient will be able to cope with urinary incontinence while preventing any complications such as poor hygiene, skin breakdown, or feelings of shame and embarrassment.
Don’t Miss: Parkinson’s Disease Head Shaking
Why Do Urgency And Frequency Occur
Bladder difficulties in Parkinsons are related to changes in the level of dopamine affecting the function of the bladder muscle. Parkinsons is also thought to affect the nerve pathway between the bladder and the part of the brain controlling bladder function. Some of the symptoms that affect bladder control are related to the level of dopamine in your body which will rise and fall depending on your medication level.
Other conditions such as weak pelvic floor muscles or an enlarged prostate will contribute to bladder symptoms. Constipation can also worsen bladder symptoms by putting pressure on the bladder.
Risk Factors For Urinary Tract Infection In Older Adults
Certain factors may increase the risk of UTIs in older people.
Conditions common in older adults may lead to urinary retention or neurogenic bladder. This increases the risk of UTIs. These conditions include Alzheimers disease, Parkinsons disease, and diabetes.
They often require people to wear incontinence briefs. If the briefs arent changed regularly, an infection may occur.
Several other things put older adults at risk for developing a UTI:
- a history of UTIs
Don’t Miss: The Last Stages Of Parkinson’s Disease
Take Control Of Your Parkinsons Treatment
OurEvery Victory Counts® manual gives people living with Parkinsons, their care partners and their family members the tools they need to take control of their own Parkinsons treatment through a proactive approach to self-care.
a powerful new print edition
Its jam-packed with up-to-date information about everything Parkinsons, plus an expanded worksheets and resources section to help you put what youve learned into action. Color coding and engaging graphics help guide you through the written material and point you to complementary videos, podcasts and other materials on the Every Victory Counts companion website. And, it is still free of charge thanks to the generosity of our sponsors.
Request your copy of the new Every Victory Counts manual by clicking the button below.
Factors Related To Urinary Incontinence
Urinary incontinence usually happens to aged people, but advanced age is not necessarily the main cause of the condition. According to data, 30% of females aged 30-60 are more likely to suffer it than men, with 1.5-5% on the whole.
The data represents a lot of circumstances exclusively for females, such as pregnancy and menopause. However, some other common causes could be for the more general population, such as urinary tract infections , medications, nerve damage, and even tumors in the urinary tract.
Knowing the triggers to urinary incontinence and how the condition itself manifests can help in creating a nursing care plan for a patient affected by it.
Read Also: What Can Cause Parkinson’s Disease
How Is Parkinsons Linked To Incontinence
People with Parkinsons disease are more likely to have incontinence because messages going from their brain to their bladder can be interrupted. This is due to Parkinsons being triggered by having fewer nerve cells which contain dopamine this is a chemical messenger which helps you to have coordinated movement.
As a result of this, the bladder will contract when its not even particularly full, meaning that your loved one may not have time to get to the toilet before urine leakage occurs.
The types of urinary incontinence most often experienced by those with Parkinsons will be nocturia and urge incontinence. It is also common for people with Parkinsons to suffer from bowel incontinence.
Helping Someone With Pd
While not everyone with PD will have related bladder issues, recent studies show that up to 40% of people will. Only about 15% of individuals will have severe Parkinson’s-related incontinence. Whether or not someone is dealing with severe incontinence, as a professional or family caregiver many steps can be taken to improve the quality of life for those with bladder issues.
Learning more about urinary incontinence and PD is the first step to helping someone struggling with both. With research, you can learn the current treatments for frequent urination and suggestions to improve managing incontinence and heighten the quality of life. Understanding the problem can help everyone, including you, so simply being an advocate is a great place to start.
Recommended Reading: Protein And Parkinson’s Medication
Why Do Some People With Parkinsons Disease Experience Urinary Incontinence
Parkinsons is best known for its effects on balance and movement, but it impacts the autonomic nervous system as well. The autonomic nervous system controls specific bodily functions, like heart rate, blood pressure, libido, and urine production.
Over time, changes to the autonomic nervous system affect your bladders ability to store and release urine. That means you might have trouble making it to the bathroom on time or need to urinate more frequently.
You May Like: Zhichan Capsule
Invest In Continence Products
Many products available can help the person to feel independent and comfortable. They will also protect clothing and furniture. These include:
- “PEE PEE Pads” or underwear for incontinence.
- Male continence sheath these can be worn over the penis, attaching to a leg bag. These are very helpful at night.
- Bed pads and mattress pads can help to keep you from doing laundry all the time!
Read Also: Can Parkinson’s Cause Congestive Heart Failure
Parkinsons Disease And Your Bladder
Many diagnosed with Parkinsons disease experience urinary tract issues. A Michigan Medicine urologist discusses treatment options for patients to consider.
Anne Pelletier-Cameron, M.D., often jokes to her patients that shes a female plumber of the lower urinary tract. On a more professional note, however, shes a urologist in the Michigan Medicine Department of Urology.
In this role, Pelletier-Cameron treats patients with a variety of lower urinary tract symptoms. Some of her patients have been diagnosed with Parkinsons disease, a progressive nervous system disorder that impacts movement. But the breakdown of nerve cells that characterize Parkinsons disease can also cause non-movement symptoms, including bladder issues.
Half of all women and 17% of men will experience urinary incontinence, or the inability to hold urine, she says, noting that for Parkinsons disease patients, those numbers escalate.
Many of my PD patients end up having other bladder problems, including issues with urgency and frequency, says Pelletier-Cameron. Nocturia, or the need to urinate many times during the night, is also common, along with difficulty in emptying the bladder.
Pelletier-Cameron says the impact of bladder symptoms cant be ignored.
Difficulty Emptying The Bladder
- Some people with Parkinsons find it difficult to pass urine if the bladder fails to contract when required, or because the sphincter does not let urine out or a combination of the two. This is a result of reduced dopamine levels interfering with the efficiency of the bladder muscles and causing a residual amount of urine to be left in the bladder. This reduces the total amount the bladder can hold and creates a feeling of wanting to empty the bladder very often. Unfortunately, there is an increased risk of urinary infection if the bladder is not emptied completely.
- In some older people, constipation which is often associated with Parkinsons can result in faeces collecting in the rectum. This can result in difficulties in bladder emptying, which may be because of pressure on the urethra, or mediated by the nerves in the region. The bladder is then unable to empty and may continue distending, causing dribbling incontinence.
- Anticholinergic medications can also make emptying problems worse.
You May Like: Medications Used For Parkinson’s Disease
Bladder Function Can Differentiate Pd From Msa
In the differential diagnosis of PD and parkinsonian type MSA, large post-void residuals, open bladder neck and neurogenic change in sphincter motor unit potentials are all common in MSA,, whereas they are rarely seen in clinically typical PD. However, recent evidence suggests that PD with dementia, or dementia with Lewy bodies, might have large post-void residuals and neurogenic change in the sphincter motor unit potentials, thereby mimicking MSA.
Institutional Characteristics And Patient Selection
This study was approved by the institutional review board at Yale University School of Medicine. Subjects were selected from patients followed by 1 physician at the Yale Urology Medical Group Clinic. All patient visits at the clinic are logged by the Patient Financial Services Department under corresponding diagnosis codes. Follow-up notes from clinic visits or phone calls are recorded in patient charts by the same physician after each encounter.
Inclusion criteria for the study were as follows: neurogenic bladder dysfunction stable traumatic SCI at least 1 year after injury bladder management with CIC minimum of 1 year follow-up by the same physician at the Yale Urology Clinic seen between the 2000 and 2010. Exclusion criteria were other etiology for neurogenic bladder such as multiple sclerosis, Parkinson disease, spina bifida, or diabetes other methods of bladder management, including other catheterization methods or Crede maneuver or had undergone urinary diversion.
| Age, years |
Note: Data presented as mean ±SD, unless noted otherwise data in parentheses are percentages. PRx = prophylaxis UTI = urinary tract infection.
Don’t Miss: Diet Soda And Parkinson’s Disease
Ui And Adverse Health Outcomes
The mean follow-up of time of the participants was nearly 8 years . We employed a Cox proportional hazards model adjusted for age, sex, and education to examine the association of baseline UI with incident parkinsonism. Baseline UI was associated with incident parkinsonism . Since we treated UI as a numerical scale, inspection of the hazard ratio suggests that an individual with severe incontinence , had about a 30% increased risk of developing parkinsonism as compared to an individual without incontinence.
Since the pathologic basis for parkinsonism in older adults with and without a clinical diagnosis of PD may vary , we repeated this analysis excluding 65 cases with a clinical diagnosis of PD. Baseline UI remained associated with incident parkinsonism . In a final model, adding terms for seven chronic health conditions and BMI did not attenuate the association of UI with incident parkinsonism .
In further analyses, we examined whether baseline UI was associated with other adverse health outcomes. Baseline UI was also associated with risk of death and incident ADL and mobility disability, but was not associated with incident MCI or AD dementia . These findings were unchanged when we controlled for seven chronic health conditions and BMI .
The Cross-Sectional and Longitudinal Associations of Baseline Urinary Incontinence and Global Cognition in Community-Dwelling Older Adults*
| Model Terms . |
|---|
Bowel Issues In Parkinsons
Recently, I was doing an interview about Parkinsons troublesome issues and I had to admit that by far my most troublesome and annoying problem is related to the effects of my gut. This is true for the majority of us living with this disease. Whether it be a direct or indirect consequence of our illness is irrelevant in my opinion when the effect is the same. Plus to be honest I am not sure anyone of us can tell the difference most of the time.
As I have re-discovered the agony of suffering from one of these ailments over the last several months when I had several bouts of ileus. In my opinion, there is nothing worse than having stomach pain, bloating, nausea, indigestion, and gas to make life miserable.
Below are all the plausible GI symptoms all of us can experience throughout our journey with PD.1 The most common symptoms are those related to poor motility or dysmotility and can be compounded by the effect of the medication.
Donât Miss: Parkinsonâs Hallucinations Commercial
Also Check: How Much Does It Cost To Treat Parkinson Disease
Various Effects Of Dopaminergic Drugs: Improvement Or Worsening
It is possible that levodopa and other antiparkinson medication could affect bladder function in PD. Aranda etâal. studied the effects of 3â8âmg apomorphine injection on the storage function in two de novo PD patients, and found that the bladder capacity increased. They gave oral levodopa to one of the patients, and the bladder capacity increased. We compared the frequency of bladder dysfunction in de novo PD and PD with levodopa. In that study, LUTS was less frequent than in the treated group. In another study, after 3âmonths of treatment with levodopa, the storage urodynamic parameters were slightly improved in de novo PD.